Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Different Types of Bearing Surfaces in Primary Total Hip Arthroplasty: A Systematic Review
Abdulaziz Almaawi*, Fahad Saleh Alabdullatif, Nouf Alabdulkarim, Deema Benfaris, Nouf Alamari and Abduljabbar AlzuhairAbdulaziz Almaawi, Orthopedic Surgery Department, College of Medicine, King Saud University, Saudi Arabia, Email: aalmaawi@ksu.edu.sa
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Objectives: An ideal hip implant is biocompatible, withstands dynamic and static loads, and resists chemical and mechanical wear. This paper aims to address failure or revisions, complication rates among different types of bearing surfaces used in total hip arthroplasty.
Methods: This review comprised scientific literature published between 1995 and 2019. We searched PubMed, Scopus, Google Scholar, Embase, and Cochrane Library and included 44 studies on adults (>18 years), all are clinical studies presenting results with more than five years of mean follow-up, and studies including any type of arthritis-all written in English. We enrolled our proposal in the international database of prospectively registered systematic reviews (PROSPERO).
Results: With a total of 8023 hips, 44 studies formed the basis of our findings. For the total population, 77.5% were diagnosed with primary osteoarthritis. The mean age of patients included in this review for MOM, COC, MOP-Conventional, MOP-HXLPE, and COP was 64.2 (10.3), 62.3 (6.8), 62.2 (4.9), 55.14 (6.9), and 59.59 (7.0) respectively. Furthermore, no significant difference was found in the followup period across the bearing surface groups (p=0.209). The revision rate in the COP group was the highest with a percentage of 4.2%, compared to other bearing surfaces. Hips that utilized MOP-HXLPE bearings had the least revision rate of 1.4%.
Conclusion: Many factors can contribute to adverse outcomes in some patient populations. These factors must be considered by the surgeon to optimize patients’ postoperative results. Factors such as implant bearing surface need to be optimized to reduce the rate of revisions.
Keywords
Hip, Arthroplasty, Arthritis, Metal, Ceramic, Polyethylene, Bearing surfaces
Introduction
Total Hip Arthroplasty (THA) continues to be the definitive solution for degenerative arthritis of the hip [1]. The procedure promises tremendous improvements not only in pain but also in functionality and overall quality of life, offering a satisfactory clinical outcome at 15 to 20-year follow-up [2,3]. Advancements in technology and design, together with ongoing improvements in surgical techniques have played an integral part in the evolution of THA; making it one of the most common elective procedures worldwide [4-7].
In a primary THA, a metal stem is introduced into the femur with a modular head, made of metal or ceramic, which articulates with the acetabular component. The acetabular component is made of a metal cup with an internal liner made of polyethylene or ceramic. The components are integrated to host bone with or without cement. Although implants vary in material, design, and size, they are all made with the sole purpose of increasing functionality and decreasing wear [1,4]. Today, there are five different material couplings used today in THA, including Metal on Metal (MOM), the widely used Metal on Polyethylene (MOP) with its subtypes, namely, the conventional and the highlycross linked, Ceramic on Ceramic (COC), Ceramic on Polyethylene (COP) and the most recent, Ceramic on Metal (COM) [8].
An ideal prosthetic joint is biocompatible, withstands dynamic and static loads, resistant to chemical and mechanical wear, and strong enough not to break. There is no single bearing surface system that guarantees all the aforementioned features. However, the number of THA revision cases has been increasing steadily. The following complications have been detected as the most common causes of revision: instability/dislocation, mechanical loosening, increased blood metal ions levels, pseudotumors, and infection [9].
This paper aims to address the failures, revisions, or complication rates among different types of bearing surfaces used in THA, solely based on level I-IV clinical studies. We aim to conduct a systemic review that could highlight the advantages and disadvantages of each of the five bearing couplings used today in THA. We believe our results will aid in the selection of a more convenient bearing surface for THA.
Literature Review
We enrolled our systematic review in the International database of prospectively registered systematic reviews (PROSPERO, CRD42020141226). Moreover, we conducted this systematic review by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [10].
Inclusion and Exclusion Criteria
We looked for multiple factors that could lead to heterogeneity by using firm inclusion and exclusion criteria. All studies eligible for inclusion had to be a study on adults >18 years old, a clinical study presenting the results of THA with more than a five-year mean follow-up, and a study including any type of hip arthritis -all written in English. Case reports or case series with less than five cases were excluded. In addition, studies reporting the results of mixed cases of revision arthroplasty, or studies that do not present the main outcomes (number of revisions or failures) were excluded.
Search Strategy
The scientific literature published between 1995 and 2019 was systematically used. The following original research study types that reported data on the treatment effects were included: Randomized Clinical Trials (RCTs) as well as prospective and retrospective studies. No restrictions were set for sample size. Laboratory studies, descriptive studies, case reports, case series, reviews, and opinion articles were excluded. We searched PubMed, Scopus, Google Scholar, Embase, and Cochrane Library to find articles related to the topic. The search was restricted to the English language. We determined the search terms through group discussion and included a natural language search, as follows: total AND Hip AND (replacement OR arthroplasty) AND (Metal OR Polyethylene OR Ceramic). After excluding duplicate documents, two independent reviewers screened the articles by title and abstract. They then made the final selection through a full-text review. We also conducted citation tracking to find additional articles and checked newly published articles by performing a search update just before completing the review. Two independent reviewers (Nouf Alabdulkarim and Deemah Bin Faris) assessed the articles separately. The data were extracted from each article without blinding to the authors, and inter-examiner conflicts were resolved by discussion of each article to reach a consensus. Two independent reviewers performed the quality evaluation of the articles retrieved (Fahad Alabdullatif) with one author (Abdulkabbar Alzuhair) acting as the coordinator. All disagreements were solved by a group discussion involving three or more investigators.
Two independent reviewers extracted the following data from the selected articles: publication year, treated hips, several patients in each group, months of follow-up, age, sex, surgery, history of disease or surgery, diagnosis, name of implant and manufacturer, Harris Hip Score (HHS), osteolysis, loosening, post-surgical complications (dislocations, recurrent dislocations, bursitis, pseudotumor formation, nerve pareses, aseptic loosening, traumatic related complication, periprosthetic femoral fracture, hematoma, heterotopic bone and Deep Vein Thrombosis (DVT), and revision surgery (failure). Failure was defined as a case of revision surgery due to an implant-related problem. A critical review of the literature relevant primary studies was assessed for methodological quality using a tool developed and tested by the Effective Public Health Practice Project (EPHPP)-EPHPP Quality Assessment Tool for Quantitative Studies. It consists of six criteria: selection bias, allocation bias, control of confounders, blinding of outcome assessors, data collection methods, and withdrawals and dropouts.
Statistical Analysis
Statistical analysis in this systematic review focused on descriptive statistics. We tabulated frequencies for the appropriate implants. Percentages were calculated by using the total number of bearing surfaces used in the relevant population as the denominator. On the other hand, means and their corresponding standard deviations were calculated using the mean values reported for each population. For some studies that did not include quantitative results in the text, we were able to read results from survival curves presented in figures. Some studies did not present risk factors in a format consistent with our analysis. For these studies, we used the reported frequencies of exposure and revision to compute crude relative risk estimates. Fisher’s exact test or chi-square test was used for categorical variables. Kruskal- Wallis test was used to determine whether there were any significant differences between more than two independent groups. All outcome metrics and raw data were tabulated in an Excel spreadsheet (Excel; Microsoft Corporation, Redmond, WA, USA).
Results
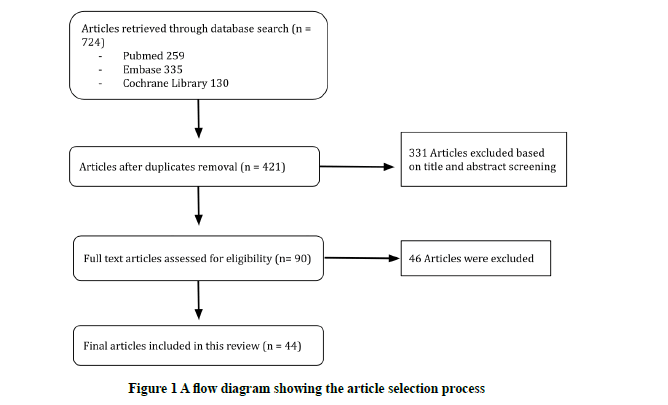
After applying the inclusion and exclusion criteria to 724 identified titles and abstracts, 724 articles were judged to be relevant and were critically reviewed. Ninety of these articles were deemed scientifically admissible. A total of 44 studies were considered overall, which formed the basis of the findings. The studies consisted of 11 Randomized Controlled Trials (RCTs) and 33-time series studies (Figure 1).
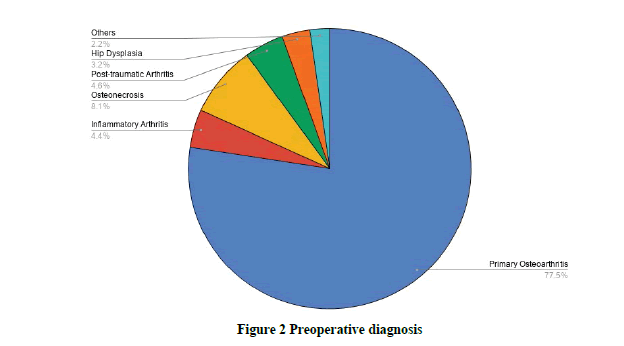
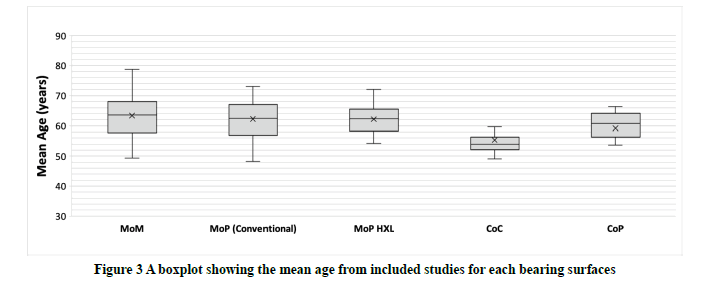
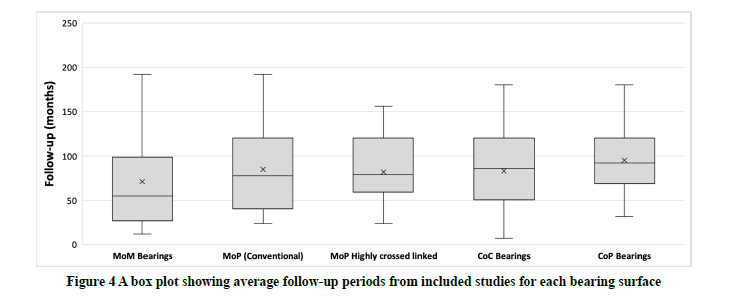
The study period for this review from the 44 included studies ranged from 1996 to 2019 (Table 1). About 8023 (THA) procedures were captured and reviewed in a total with 1691 (MOM), 1857 (MOP-Conventional), 847 (MOP-HXLPE), 3057 (COC), and 571 (COP) implants. For the total population, 77.5% were diagnosed with primary osteoarthritis (Figure 2). The mean age of patients included in this review for MOM, COC, MOP-Conventional, MOP-HXLPE, and COP was 64.2 (10.3), 62.3 (6.8), 62.2 (4.9), 55.14 (6.9), and 59.59 (7.0) respectively (Figure 3). There was a significant difference calculated when comparing age across the five studied bearing surfaces. Of these, MoM-bearing surface patients had the highest mean age compared to patients with other bearing surfaces (p-value=0.005). Moreover, the mean follow-up period in this review for MOM, COC, MOP-Conventional, MOP-HXLPE, and COP was 90.4 months (53.1), 97.8 (46.6), 93.7 (36.0), 98.8 (44.5), and 92.06 (40.4) respectively (Figure 4). Notably, no significant difference was found for the follow-up period across the bearing surface groups (p value=0.209).
| Author | Year | Hips | Pre op HHS | Post Op HHS | Loosening | Osteolysis | Revision | Age | Mean F/U |
|---|---|---|---|---|---|---|---|---|---|
| Metal on Metal | |||||||||
| Engh [11] | 2014 | 52 | N | N | 0 | 0 | 0 | 62.8 | 60 |
| Lombardi [12] | 2004 | 46 | 93.1 | N | 0 | 0 | 0 | N | 68.4 |
| Garellick [13] | 1999 | 204 | N | 82 | 4 | N | 7 | 70 | 120 |
| Dahlstrand [14] | 2017 | 41 | 38 | 91 | 1 | N | 2 | 65 | 192 |
| Borgwardt [15] | 2017 | 72 | 47.5 | 97.7 | 0 | N | 3 | 68.2 | 120 |
| Van Der Veen [16] | 2019 | 102 | N | N | 1 | N | 4 | 78.8 | 158.4 |
| Vendittoli [17] | 2013 | 100 | N | N | 0 | 30 | 4 | 51 | 96 |
| Higuchi [18] | 2018 | 134 | 55.6 | 92.65 | 1 | 8 | 0 | 62.65 | 60 |
| Desmarchelier [19] | 2013 | 125 | N | N | 1 | 0 | 2 | 63.7 | 100 |
| Bjorgul [20] | 2013 | 129 | N | 91.1 | 4 | N | 8 | 63.3 | 84 |
| Zijlstra, W. P. [21] | 2010 | 200 | 47 | 86.5 | 6 | 0 | 6 | 70.5 | 66.7 |
| Metal on Polyethylene (HXL) | |||||||||
| Engh [22] | 2012 | 116 | N | 88 | N | 1 | 2 | 62.5 | 120 |
| Engh [11] | 2014 | 33 | N | N | 0 | 0 | 1 | 61.6 | 60 |
| Engh [23] | 2006 | 116 | N | N | 0 | 7 | 0 | 62.5 | 67 |
| GarciaNRey [24] | 2013 | 42 | N | N | 0 | 0 | 1 | 67.4 | 120 |
| Nakahara [25] | 2010 | 47 | N | N | 0 | 0 | 0 | 56.9 | 79.2 |
| Garcia-Rey [26] | 2008 | 45 | N | N | 0 | 0 | 0 | 62.5 | 66.3 |
| Morison [27] | 2014 | 23 | 46.2 | 90.5 | N | N | 1 | 66 | 60 |
| Langlois [28] | 2015 | 50 | N | N | 0 | 0 | 0 | N | 109.2 |
| Matthew G. [29] | 2016 | 50 | 37.3 | 85.6 | 0 | 0 | 1 | 72 | 156 |
| Devane [30] | 2017 | 57 | N | N | N | N | 2 | 61 | 120 |
| 2017 | 55 | N | N | N | N | 0 | 62 | 72 | |
| Thomas [31] | 2011 | 22 | N | N | 0 | 1 | 0 | 68 | 84 |
| Triclot, P. [32] | 2007 | 33 | N | N | N | N | 1 | 70.6 | 58.8 |
| Zhi Li, MM [33] | 2018 | 28 | N | 88.9 | N | N | 1 | 59.16 | 81.9 |
| Geerdink [34] | 2009 | 17 | 39 | 95 | 0 | 0 | 0 | 64 | 96 |
| Atrey [35] | 2017 | 32 | NM | 91.1 | 0 | 0 | 1 | 55.06 | 120 |
| Higuchi [36] | 2016 | 81 | 55.4 | 86.4 | 3 | 2 | 1 | 54.2 | 123 |
| Metal on Polyethylene (CONVENTIONAL) | |||||||||
| Lombardi [12] | 2004 | 53 | N | 94.3 | 0 | 0 | 0 | N | 68.4 |
| Garellick [13] | 1999 | 206 | N | 81 | 5 | 0 | 8 | 70 | 120 |
| Marston [37] | 1996 | 213 200 |
46 | 91.3 | 16 | N | 16 | 67 | 77 |
| Engh [38] | 2006 | 116 | N | N | 0 | 7 | 0 | 62.5 | 67 |
| Garcia-Rey [24] | 2013 | 41 | N | N | 0 | 1 | 0 | 61.1 | 120 |
| Nakahara [25] | 2010 | 74 | N | N | 0 | 0 | 0 | 56.9 | 79.2 |
| Garcia-Rey [26] | 2008 | 45 | N | N | 0 | 0 | 0 | 62.5 | 66.3 |
| Langlois [28] | 2015 | 50 | N | N | 0 | 0 | 0 | N | 109.2 |
| Matthew G. [29] | 2016 | 50 | 37.5 | 89.5 | 0 | 1 | 1 | 72 | 156 |
| Devane [30] | 2017 | 59 | N | N | N | N | 10 | 61 | 120 |
| Dahlstrand [14] | 2017 | 44 | 37 | 95 | 1 | N | 2 | 65 | 192 |
| Stihsen [39] | 2008 | 67 | 43 | 91 | 1 | N | 1 | 73 | 60 |
| Devane [30] | 2017 | 55 | N | N | N | N | 1 | 61 | 72 |
| Thomas [31] | 2011 | 22 | N | N | N | 4 | 0 | 68 | 84 |
| Triclot [32] | 2007 | 69 | N | N | N | N | 1 | 70.6 | 58.8 |
| Vendittoli [40] | 2007 | 69 | N | N | 0 | 3 | 4 | 56.8 | 79 |
| 116 | 0 | 3 | 6 | 54.9 | 79 | ||||
| Geerdink [34] | 2009 | 23 | 40 | 93 | 1 | 1 | 1 | 64 | 96 |
| Haddad [41] | 2015 | 40 | 43.2 | 96 | 0 | 0 | 0 | 48.2 | 145 |
| Atrey [35] | 2017 | 36 | 49 | 81.9 | 0 | 4 | 1 | 52.58 | 120 |
| Dahlstrand [11] | 2017 | 44 | 37 | 95 | 1 | 0 | 2 | 67 | 192 |
| Bjorgul [20] | 2013 | 137 | N | 93.8 | 0 | N | 3 | 62.8 | 84 |
| D’Antonio [42] | 2012 | 72 | 49.8 | 96.5 | 0 | 3 | 10 | 53.5 | 120 |
| Ceramic on Ceramic | |||||||||
| R. P. Pitto [43] | 2002 | 10 | 55.6 | 96 | 0 | 0 | 0 | 57.8 | 61.2 |
| Ochs [44] | 2007 | 22 | N | 91 | 0 | 0 | 1 | 56 | 100.8 |
| Atrey [45] | 2018 | 29 | 50 | 94.6 | 1 | 0 | 5 | 41.5 | 180 |
| Buttaro [46] | 2017 | 939 | N | N | 2 | N | 9 | 49 | 63.6 |
| Mesko [47] | 2011 | 325 | N | N | N | N | 8 | 52.7 | 99.6 |
| 605 | N | N | N | N | 11 | 50.5 | 57.6 | ||
| Borgwardt [15] | 2017 | 76 | 47.9 | 90.3 | 0 | N | 19 | 69.1 | 120 |
| Atrey [35] | 2017 | 34 | 45.6 | 86.3 | 0 | N | 0 | 52 | 120 |
| Beaupre [48] | 2016 | 48 | N | N | 0 | 0 | 0 | 53 | 120 |
| Hamilton [49] | 2010 | 177 | 50.6 | 94.4 | 3 | 0 | 4 | 56.4 | 31.1 |
| Beaupre [48] | 2015 | 48 | N | N | N | N | 0 | 51.3 | 120 |
| Higuchi [36] | 2016 | 67 | 56.1 | 88.9 | 0 | 1 | 1 | 54 | 121 |
| Higuchi [18] | 2018 | 96 | 59.8 | 89.5 | 0 | 2 | 1 | 55.5 | 84 |
| Desmarchelier [19] | 2013 | 125 | N | N | 0 | 0 | 1 | 59.6 | 109.8 |
| D’Antonio [42] | 2011 | 73 | 50.6 | 96.8 | N | N | 2 | 54.9 | 120 |
| 71 | 47.9 | 96.2 | N | N | 4 | 54.8 | 120 | ||
| D’Antonio [50] | 2005 | 222 | N | 96.6 | 1 | 0 | 6 | 54 | 71 |
| D’Antonio [51] | 2005 | 109 | N | N | 1 | 0 | 4 | 54 | 68.4 |
| 113 | N | N | 0 | 2 | 2 | 53 | 67.2 | ||
| Ceramic on Polyethylene | |||||||||
| Ochs [44] | 2007 | 21 | N | 89 | 0 | 0 | 0 | 61.5 | 100.8 |
| Lombardi [52] | 2009 | 64 | 48 | 92 | 1 | N | 3 | 60 | 72 |
| Nakahara [25] | 2010 | 47 | N | N | 0 | 0 | 0 | 57.5 | 80.4 |
| Atrey [45] | 2018 | 29 | 48.8 | 88.7 | 0 | 4 | 5 | 42.8 | 180 |
| Morison [27] | 2014 | 21 | 43 | 84.9 | N | N | 1 | 64.8 | 60 |
| 22 | 49.2 | 91.4 | N | N | 1 | 63.9 | 60 | ||
| Sobti [53] | 2019 | 116 | 39 | 91 | 0 | 0 | 0 | 63.8 | 104 |
| Borgwardt [15] | 2017 | 76 | 39 | 94.7 | 1 | N | 10 | 66.4 | 120 |
| Hamilton [49] | 2010 | 87 | 50.7 | 92 | 0 | 0 | 0 | 57.3 | 31.5 |
| Beaupre [48] | 2015 | 44 | N | N | 0 | 0 | 3 | 53.6 | 120 |
| Bjorgul [20] | 2013 | 131 | N | 93.6 | 0 | N | 1 | 63.9 | 84 |
HXL: Highly Cross-Linked, N: Not recorded, HHS: Hip Harris Score, F/U: Follow up
Table 1: Clinical outcome of individual studies
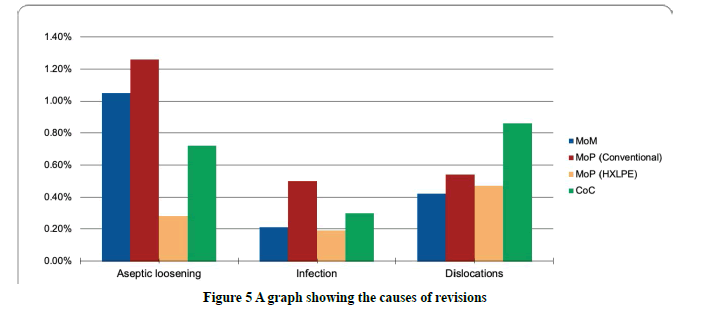
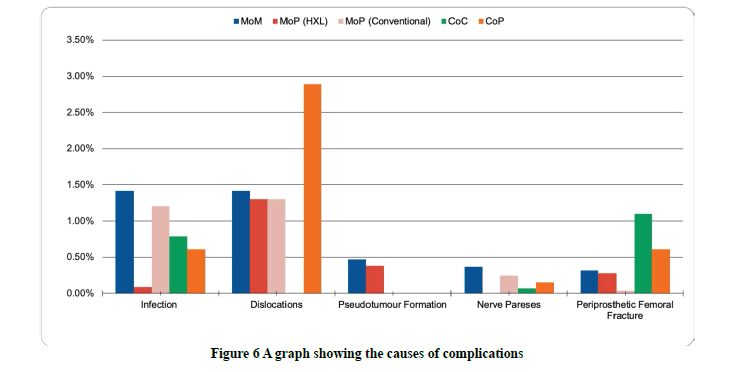
The revision rate in the COP group was the highest, scoring a percentage of 4.2% as compared to other bearing surfaces, in which the most common cause of revision was a dislocation. However, this rate was not considered significant compared to other groups (p-value=0.081). MOP-conventional bearing surfaces ranked third in regards to revision rates (3.5%) (range: 0%-17.0%), in which revisions were mainly due to aseptic loosening (21 cases; 1.1%). On the other hand, MOM-bearing surfaces had a revision rate of 3.1% (range: 0%-8.1%), among which 20 hips (1.2%) were revised because of aseptic loosening. However, this rate could be misleading given the difference in the number of hips in each group. Following that was the COC bearing surface followed by a revision rate of 2.5% (range: 0%-25%). Hips that utilized MOP-HXLPE bearings had the least revision rate of 1.4% (range: 0%-4.4%). Out of these revised hips, only 3 hips (0.28%) were due to aseptic loosening (Figures 5 and 6). Notably, dislocation was the most common cause for revision for COC bearing surfaces (26 cases; 0.8%) followed by MOP-conventional (13 cases; 0.7%). The difference in revision rate due to recurrent dislocation was considered statistically significant when comparing COC to the other bearing surfaces groups (p-value=0.003). Additionally, aseptic loosening rates were significantly lower for MOP-HXLPE bearing surface compared with MOP-Conventional (p-value=0.01). In terms of osteolysis, MOM (2.0%) bearing surfaces had higher rates compared to COP (1.2%) and COC (0.28%) bearing surfaces. However, this difference was not considered statistically significant. Finally, there was no significant difference in terms of the HHS between all the investigated bearing surfaces (p-value=0.439) (Table 2).
| MoM | MoP-Conventional | MOP-HXLPE | CoC | CoP | p-value | |
|---|---|---|---|---|---|---|
| Hips count | 1691 | 1857 | 847 | 3057 | 571 | - |
| Age, mean (± SD) | 64.2 (10.3) | 62.3 (6.8) | 62.2 (4.9) | 55.14 (6.9) | 59.59 (7.0) | 0.005b |
| HHS difference, mean (± SD) | 44.9 (6.9) | 47.6 (7.1) | 4 4.9 (7.3) | 41.5 (6.0) | 45.8 (6.5) | 0.439b |
| Follow-up, mean (± SD) | 90.4 (53.1) | 97.8 (46.6) | 93.7 (36.0) | 98.8 (44.5) | 92.06 (40.4) | 0.209b |
| Osteolysis | 40 (2.0) | 27 (1.45) | 11 (1.3) | 5 (0.28) | 4 (1.2) | 0.575c |
| Revision | 51 (3.1) | 65 (3.5) | 12 (1.4) | 77 (2.5) | 24 (4.2) | 0.081c |
MoM: Metal on Metal, MoP-Conventional: Metal on Polyethylene Conventional, MOP-HXLPE: Metal on Polyethylene (highly cross-linked polyethylene), CoC: Ceramic on Ceramic, CoP: Ceramic on Polyethylene, CoM: Ceramic on Metal. HHS: Harris Hip Score
All percentages were calculated using the total hips as the denominator unless stated otherwise.
b: Differences between groups were compared using the Kruskal-Wallis test.
c: Differences between groups were compared using the chi-square test.
Table 2: Demographic data and outcome measurement
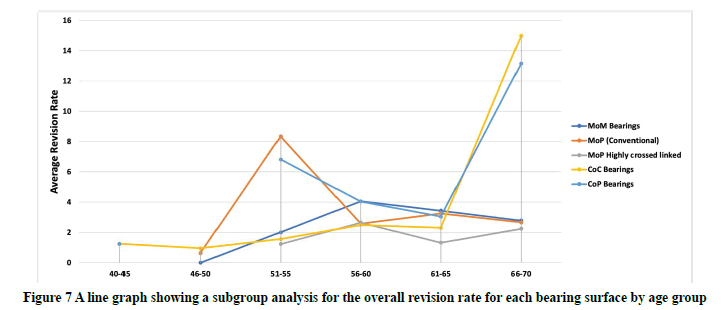
For patients aged less than 65 years, there was no significant difference in revision rates in all of the study groups (p-value=0.09); however, for the age group 51-55 years, higher revision rates were notable for the MOP-Conventional (8.3%) and COP (6.8%) bearing surfaces. For patients 66-year-old or older, exceptionally higher and statistically significant revision rates were seen for the COC (15.0%) and COP (13.1%) bearing surfaces when compared with lower age groups, with p values of 0.01 and 0.03 respectively. Moreover, MOP-HXLPE has a statistically significant lower revision rate compared with MOP-Conventional for all age groups. The difference increases with the increase of age (p-value=0.03) (Figure 7).
Discussion
The decision of choosing different bearing surfaces in THA, especially in young and active patients, has always been the main focus of arthroplasty surgeons in terms of which bearing surface has the least wear and the longest survival [2,4]. As an alternative to conventional polyethylene, Metal on Metal (MOM), Metal or Ceramic on high cross-linked Polyethylene (MOP) (COP), and Ceramic on Ceramic (COC) have become popular choices amongst arthroplasty surgeon, knowing the advantage and disadvantage of each bearing surface can aid in choosing the best combination for the better long-term survival of the implant [3-5].
MOM bearing surfaces used to be popularly utilized as bearing couple in THA, as they have low wear rate and enhanced stability making them a very efficacious bearing couple to be used in young patients. After multiple studies and increase in knowledge that was gained over the past years; it was found that this type of bearing surface indeed carries less wear rate and smaller particle size when compared to MOP; but had a 13- to 500-fold increase in particles generated than polyethylene per year [54,55]. The effects of these generated particles on the body were found on local soft tissue as pseudotumor formation which was documented to be in as high as 35% of patients. A pseudotumor is often painful and mimics infection with destructive effects on the bone and soft tissue [54,56,57]. Moreover, systemic increase in metal ion levels, which is increased due to many factors (Abduction angle >55, metal hypersensitivity, increased head size, and female sex). The effect of increased ion levels poses harmful effects to various organs in the body as well to females of childbearing age as metal ions can cross the blood placenta barrier and can cause harm to the fetus [11,14,54,56,58]. Therefore, the use of MOM was reduced and abandoned in some centers by most arthroplasty surgeons due to increased rates of revision rates and increased risks that outweigh the benefits [54,55].
In MOP bearing surfaces are the most commonly used bearing couple in THA worldwide about 80% of total hip replacements done in the United States of America are metal on XLP. Two different forms of PE are available (standard PE (SP)) and (cross-linked PE (XLP)). Both have the same material but different properties, the difference in properties are related to the difference in the manufacturing process. In SP, it is irradiated with doses of 2.5 to 40 KGray while XLP 50-100 KGray to increase cross-linking between free radicals and enhance the properties of the poly, crosslinking reaches the maximum at 100 KGray after this dose. That will increase the number of free radicals generated, the breakdown of material, and decreases the mechanical strength of the PE [59,60]. So to decrease the free radical generated and enhance cross-linking was done via thermal processing, re-melting to >137 °C. This process will trigger more free radicals to cross-link but will compromise the mechanical strength of the PE [59]. The other method of thermal processing is annealing which is heating the PE to <137 °C, which will heat the PE to temperatures below the melting point hence preserving the mechanical strength of the poly, increase durability, and lower crack propagation. In this process, a higher number of free radicals is produced and will be subjected later to oxidation and wear in vivo [61].
Both methods of thermal processing have resulted in reducing wear rate and enhancing the mechanical characteristics of the XLP when compared to SP [62,63]. In in vitro studies on wear rate were compared between SP and XLP. Findings indicate lower wear rates for metal with XLP bearing surface as compared to SP. Fisher, et al. found 8 folds increase in wear rate in SP when compared to 100 KGy irradiated XLP with smaller wear particles [63,64]. A systemic review by Kuzyk, et al. has shown that femoral head penetration in XLP is 0.042 mm/y in comparison to 0.137 mm/y in SP [63]. Polyethylene is used in a wide range in orthopedic surgery not only in THA as it carries many advantages, but they also work as shock absorbers, more forgiving when malalignment occurs and they well tolerate edge loading in THA, as well the lower cost and good wear rate makes it a good option to be used in elderly patients and patients with lower activity [65].
When comparing SP to XLP liners, the main complication was osteolysis secondary to an increase in the wear rate. In the literature, SP wears rate was (0.1-0.2 mm/year) with larger particulate, while in XLP wear rate was (0.051-0.025 mm/year) with smaller debris which was reflected also on our results. Osteolysis and active resorption of bone develop in response to particulate wear debris that is produced during the normal use of the total joint replacement. That leads to stimulation of local and systemic responses that causes chronic inflammation [63,66-69]. As part of the immune system, monocytes/macrophages initiate the inflammatory response by interacting with wear debris which releases pro-osteoclastic factors (RANKL) and other chemokines and ultimately activating of osteoclast bone resorption leading to osteolysis [66,68].
On the other hand, ceramic bearings were first introduced in 1970. They became popular because of their lower wear rates and increased mechanical strength. Unfortunately, early results were not promising as they carried increased rates of aseptic loosening and component fracture [59]. But after multiple in vivo, and in vitro studies, by changing the materials used in the manufacturing of ceramics, changing the process of fabrication and finishing increased the cost of the implant (average cost $3200) of this particular bearing surface [70,71]. Moreover, it led to an increase in resisting wear and scratching and to a decrease in the fracture rate of the head. However, when compared to other bearing surfaces it still has a higher rate of fracture (0.004% for third-generation COC bearing) [61,72]. The smooth surface and hydrophilic properties of ceramic surfaces had resulted in reducing the friction at the bearing surface; by attracting synovial fluids in, which led to reducing abrasive wear [64].
Another complication of ceramic bearing surfaces is the audible sounds (squeaking) reported by patients during normal daily activities. About 3% of patients who underwent COC THA in North America had squeaking. The reason behind it these sounds remain unclear, but many theories have been produced, one theory suggested by Reiker, et al. was that the sounds are due to a deficiency of fluid lubrication between the bearing surfaces. Another theory has suggested a mismatch between head and acetabular liner. A third theory supposes the sound is produced by metal debris entrapped between the bearing surfaces [73-75].
In comparison between COC to COP bearing surfaces in the literature, it was found that COC bearing has a higher rate of squeaking, fracture, and cost, while COP bearing carries a higher rate of wear. In terms of dislocation, loosening, hip function, osteolysis, and revision the rates were comparable between the two bearing surfaces which were reflected in the results of this study [71-73,76-78]. Since the ceramic bearing has the lowest wear rate among all bearing surfaces, it makes it the favorable bearing option to be used in young active patients to aid in increasing the longevity of the implant and decrease the chances of early revisions [61,64].
The different characteristics of different bearing surfaces have made choosing the best combination controversial. COC bearing surface has shown the best wear properties amongst all of the bearing surfaces but has a higher cost, squeaking sound, fracture, and less modularity with fewer neck lengths. While MOP had the lowest cost and most modularity but carries fewer wear properties than MoM. On the other hand, MOM had a better wear property than MOP, but they are more expensive (average cost of MOM is $2196, MOP is $2060), and carries the risk of forming pseudotumors and high metal ions in the serum and urine [55,56,70,71,76].
The long-term survival of THA is a multifactorial issue, in which factors other than the implant, such as diagnosis, patient factors (bone quality, deformity, age, activity levels), surgeon skill, and surgical technique are considered confounders of survival rates. The average rates of revision (6% after 5 years and 12% after 10 years) which is crucial to investigate the association between failure modes and patient-related factors, and the time of a revision to improve their THA outcomes [1]. Common causes of revision THA are wear, loosening, dislocation or instability, and infection [3]. A previous systematic review by Prokopetz, et al. shows that older age at primary THA, male gender and diagnosis of rheumatoid arthritis and avascular necrosis were all found to be important risk factors for implant failure, regardless of implant material [79]. In that sense, certain factors play a role in each of the different causes of revision. Liu KL, et al. have found that longer operating times and male gender were considered risk factors for infections postoperatively [80]. On the other hand, when revision for dislocation was considered, older age, smaller head sizes, and a posterior approach were found to have a higher risk of dislocation [81]. Alabdulkarim, et al. proved in their meta-analysis that fixation type was not a risk factor as measured by revision rates [81].
The Australian Orthopedic Association National Joint Replacement Registry annual report (2018) showed that the most common reasons for failure and revision of conventional THA are loosening (25.6%), dislocation (21.6%), fracture (19.5%), and infection (17.7%) [82]. Revision rates due to loosening were 44.1%, followed by infection (19.5%), fracture (13.6%) and dislocation (12.6%) [12].
Total hip arthroplasty is a highly successful intervention, presenting long-term functional benefits. However, with the increased life expectancy in a globally aging population; the number of THA procedures will increase and lead to an increased rate of revision THA. Many factors can contribute to adverse outcomes in some patient populations and these factors must be considered by the surgeon to optimize patients’ postoperative results. Factors such as implant bearing surface, age, gender, body mass index, and surgical technique, are considered confounders of survival rates. Thus, they represent current ar
The decision of choosing different bearing surfaces in THA, especially in young and active patients, has always been the main focus of arthroplasty surgeons in terms of which bearing surface has the least wear and the longest survival [2,4]. As an alternative to conventional polyethylene, Metal on Metal (MOM), Metal or Ceramic on high cross-linked Polyethylene (MOP) (COP), and Ceramic on Ceramic (COC) have become popular choices amongst arthroplasty surgeon, knowing the advantage and disadvantage of each bearing surface can aid in choosing the best combination for the better long-term survival of the implant [3-5].
MOM bearing surfaces used to be popularly utilized as bearing couple in THA, as they have low wear rate and enhanced stability making them a very efficacious bearing couple to be used in young patients. After multiple studies and increase in knowledge that was gained over the past years; it was found that this type of bearing surface indeed carries less wear rate and smaller particle size when compared to MOP; but had a 13- to 500-fold increase in particles generated than polyethylene per year [54,55]. The effects of these generated particles on the body were found on local soft tissue as pseudotumor formation which was documented to be in as high as 35% of patients. A pseudotumor is often painful and mimics infection with destructive effects on the bone and soft tissue [54,56,57]. Moreover, systemic increase in metal ion levels, which is increased due to many factors (Abduction angle >55, metal hypersensitivity, increased head size, and female sex). The effect of increased ion levels poses harmful effects to various organs in the body as well to females of childbearing age as metal ions can cross the blood placenta barrier and can cause harm to the fetus [11,14,54,56,58]. Therefore, the use of MOM was reduced and abandoned in some centers by most arthroplasty surgeons due to increased rates of revision rates and increased risks that outweigh the benefits [54,55].
In MOP bearing surfaces are the most commonly used bearing couple in THA worldwide about 80% of total hip replacements done in the United States of America are metal on XLP. Two different forms of PE are available (standard PE (SP)) and (cross-linked PE (XLP)). Both have the same material but different properties, the difference in properties are related to the difference in the manufacturing process. In SP, it is irradiated with doses of 2.5 to 40 KGray while XLP 50-100 KGray to increase cross-linking between free radicals and enhance the properties of the poly, crosslinking reaches the maximum at 100 KGray after this dose. That will increase the number of free radicals generated, the breakdown of material, and decreases the mechanical strength of the PE [59,60]. So to decrease the free radical generated and enhance cross-linking was done via thermal processing, re-melting to >137 °C. This process will trigger more free radicals to cross-link but will compromise the mechanical strength of the PE [59]. The other method of thermal processing is annealing which is heating the PE to <137 °C, which will heat the PE to temperatures below the melting point hence preserving the mechanical strength of the poly, increase durability, and lower crack propagation. In this process, a higher number of free radicals is produced and will be subjected later to oxidation and wear in vivo [61].
Both methods of thermal processing have resulted in reducing wear rate and enhancing the mechanical characteristics of the XLP when compared to SP [62,63]. In in vitro studies on wear rate were compared between SP and XLP. Findings indicate lower wear rates for metal with XLP bearing surface as compared to SP. Fisher, et al. found 8 folds increase in wear rate in SP when compared to 100 KGy irradiated XLP with smaller wear particles [63,64]. A systemic review by Kuzyk, et al. has shown that femoral head penetration in XLP is 0.042 mm/y in comparison to 0.137 mm/y in SP [63]. Polyethylene is used in a wide range in orthopedic surgery not only in THA as it carries many advantages, but they also work as shock absorbers, more forgiving when malalignment occurs and they well tolerate edge loading in THA, as well the lower cost and good wear rate makes it a good option to be used in elderly patients and patients with lower activity [65].
When comparing SP to XLP liners, the main complication was osteolysis secondary to an increase in the wear rate. In the literature, SP wears rate was (0.1-0.2 mm/year) with larger particulate, while in XLP wear rate was (0.051-0.025 mm/year) with smaller debris which was reflected also on our results. Osteolysis and active resorption of bone develop in response to particulate wear debris that is produced during the normal use of the total joint replacement. That leads to stimulation of local and systemic responses that causes chronic inflammation [63,66-69]. As part of the immune system, monocytes/macrophages initiate the inflammatory response by interacting with wear debris which releases pro-osteoclastic factors (RANKL) and other chemokines and ultimately activating of osteoclast bone resorption leading to osteolysis [66,68].
On the other hand, ceramic bearings were first introduced in 1970. They became popular because of their lower wear rates and increased mechanical strength. Unfortunately, early results were not promising as they carried increased rates of aseptic loosening and component fracture [59]. But after multiple in vivo, and in vitro studies, by changing the materials used in the manufacturing of ceramics, changing the process of fabrication and finishing increased the cost of the implant (average cost $3200) of this particular bearing surface [70,71]. Moreover, it led to an increase in resisting wear and scratching and to a decrease in the fracture rate of the head. However, when compared to other bearing surfaces it still has a higher rate of fracture (0.004% for third-generation COC bearing) [61,72]. The smooth surface and hydrophilic properties of ceramic surfaces had resulted in reducing the friction at the bearing surface; by attracting synovial fluids in, which led to reducing abrasive wear [64].
Another complication of ceramic bearing surfaces is the audible sounds (squeaking) reported by patients during normal daily activities. About 3% of patients who underwent COC THA in North America had squeaking. The reason behind it these sounds remain unclear, but many theories have been produced, one theory suggested by Reiker, et al. was that the sounds are due to a deficiency of fluid lubrication between the bearing surfaces. Another theory has suggested a mismatch between head and acetabular liner. A third theory supposes the sound is produced by metal debris entrapped between the bearing surfaces [73-75].
In comparison between COC to COP bearing surfaces in the literature, it was found that COC bearing has a higher rate of squeaking, fracture, and cost, while COP bearing carries a higher rate of wear. In terms of dislocation, loosening, hip function, osteolysis, and revision the rates were comparable between the two bearing surfaces which were reflected in the results of this study [71-73,76-78]. Since the ceramic bearing has the lowest wear rate among all bearing surfaces, it makes it the favorable bearing option to be used in young active patients to aid in increasing the longevity of the implant and decrease the chances of early revisions [61,64].
The different characteristics of different bearing surfaces have made choosing the best combination controversial. COC bearing surface has shown the best wear properties amongst all of the bearing surfaces but has a higher cost, squeaking sound, fracture, and less modularity with fewer neck lengths. While MOP had the lowest cost and most modularity but carries fewer wear properties than MoM. On the other hand, MOM had a better wear property than MOP, but they are more expensive (average cost of MOM is $2196, MOP is $2060), and carries the risk of forming pseudotumors and high metal ions in the serum and urine [55,56,70,71,76].
The long-term survival of THA is a multifactorial issue, in which factors other than the implant, such as diagnosis, patient factors (bone quality, deformity, age, activity levels), surgeon skill, and surgical technique are considered confounders of survival rates. The average rates of revision (6% after 5 years and 12% after 10 years) which is crucial to investigate the association between failure modes and patient-related factors, and the time of a revision to improve their THA outcomes [1]. Common causes of revision THA are wear, loosening, dislocation or instability, and infection [3]. A previous systematic review by Prokopetz, et al. shows that older age at primary THA, male gender and diagnosis of rheumatoid arthritis and avascular necrosis were all found to be important risk factors for implant failure, regardless of implant material [79]. In that sense, certain factors play a role in each of the different causes of revision. Liu KL, et al. have found that longer operating times and male gender were considered risk factors for infections postoperatively [80]. On the other hand, when revision for dislocation was considered, older age, smaller head sizes, and a posterior approach were found to have a higher risk of dislocation [81]. Alabdulkarim, et al. proved in their meta-analysis that fixation type was not a risk factor as measured by revision rates [81].
The Australian Orthopedic Association National Joint Replacement Registry annual report (2018) showed that the most common reasons for failure and revision of conventional THA are loosening (25.6%), dislocation (21.6%), fracture (19.5%), and infection (17.7%) [82]. Revision rates due to loosening were 44.1%, followed by infection (19.5%), fracture (13.6%) and dislocation (12.6%) [12].
Total hip arthroplasty is a highly successful intervention, presenting long-term functional benefits. However, with the increased life expectancy in a globally aging population; the number of THA procedures will increase and lead to an increased rate of revision THA. Many factors can contribute to adverse outcomes in some patient populations and these factors must be considered by the surgeon to optimize patients’ postoperative results. Factors such as implant bearing surface, age, gender, body mass index, and surgical technique, are considered confounders of survival rates. Thus, they represent current areas of research and deserve attention in today’s healthcare systems. This study has many limitations. First, remaining heterogeneity is a possibility between different studies. This issue has been discussed at the project design stage and data analysis and pooling were conducted after sufficient adjustment of bias. Second, loosening and other complications are defined using different criteria in each study. We used common and objective items and eliminated all the ambiguous data to increase credibility. The third limitation is the lack of longer follow-up among all studies included in this review.
eas of research and deserve attention in today’s healthcare systems. This study has many limitations. First, remaining heterogeneity is a possibility between different studies. This issue has been discussed at the project design stage and data analysis and pooling were conducted after sufficient adjustment of bias. Second, loosening and other complications are defined using different criteria in each study. We used common and objective items and eliminated all the ambiguous data to increase credibility. The third limitation is the lack of longer follow-up among all studies included in this review.Conclusion
Many factors can contribute to adverse outcomes in some patient populations. These factors must be considered by the surgeon to optimize patients’ post-operative results. Factors such as implant bearing surface need to be optimized to reduce the rate of revisions.
Recommendations
We emphasize the need for new randomized controlled trials with meticulous reporting on outcomes to enhance decision making leading to implant success.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Authors Contributions
Almaawi A. and Alabdullatif F. conceived and designed the study and conducted the literature review. Alabdulkarim N., Alfaris D., and Alamari N. provided research materials and data collection. Alzuhair A. analyzed and interpreted data. Alabdullatif F. wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript. All authors testify that all persons designated as authors qualify for authorship and have checked the article for plagiarism. If plagiarism is detected, all authors will be held equally responsible and will bear the resulting sanctions imposed by the journal thereafter.
References
- Pivec, Robert, et al. "Hip arthroplasty."The Lancet,Vol. 380, No. 9855, 2012, pp. 1768-77.
- Kremers, Hilal Maradit, et al. "Prevalence of total hip and knee replacement in the United States."The Journal of Bone and Joint Surgery. American, Vol.97, No. 17, 2015, pp. 1386-97.
- Karachalios, Theofilos, George Komnos, and Antonios Koutalos. "Total hip arthroplasty: Survival and modes of failure."EFORT Open Reviews,Vol. 3, No. 5, 2018, pp. 232-39.
- Learmonth, Ian D., Claire Young, and Cecil Rorabeck. "The operation of the century: Total hip replacement."The Lancet,Vol. 370, No. 9597, 2007, pp. 1508-19.
- Laupacis, Andreas, et al. "The effect of elective total hip replacement on health-related quality of life."The Journal of Bone and Joint Surgery. American, Vol.75, No. 11, 1993, pp. 1619-26.
- Morshed, Saam, et al. "Comparison of cemented and uncemented fixation in total hip replacement: A meta-analysis."Acta Orthopaedica,Vol. 78, No. 3, 2007, pp. 315-26.
- Pakvis, Dean, et al. "Is there evidence for a superior method of socket fixation in hip arthroplasty? A systematic review."International Orthopaedics,Vol. 35, No. 8, 2011, pp. 1109-18.
- Marques, Elsa MR, et al. "The choice between hip prosthetic bearing surfaces in total hip replacement: A protocol for a systematic review and network meta-analysis."Systematic Reviews,Vol. 5, No. 1, 2016, p. 19.
- Bozic, Kevin J., et al. "The epidemiology of revision total hip arthroplasty in the United States."Journal of Bone and Joint Surgery JBJS,Vol. 91, No. 1, 2009, pp. 128-33.
- Moher, David, et al. "Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement."PLoS Medicine,Vol. 6, No. 7, 2009, p. e1000097.
- Engh, C. A., et al. "Metal ion levels after metal-on-metal total hip arthroplasty: A five-year, prospective randomized trial."Journal of Bone and Joint Surgery,Vol. 96, No. 6, 2014, pp. 448-55.
- Lombardi Jr, Adolph V., et al. "Mid-term results of a polyethylene-free metal-on-metal articulation."The Journal of Arthroplasty,Vol. 19, No. 7, 2004, pp. 42-47.
- Garellick, Goran, Henrik Malchau, and Peter Herberts. "The Charnley versus the spectron hip prosthesis: Clinical evaluation of a randomized, prospective study of 2 different hip implants."The Journal of Arthroplasty,Vol. 14, No. 4, 1999, pp. 407-13.
- Dahlstrand, Henrik, et al. "Comparison of metal ion concentrations and implant survival after total hip arthroplasty with metal-on-metal versus metal-on-polyethylene articulations: A 16-year follow-up of a prospective randomized study."Acta Orthopaedica,Vol. 88, No. 5, 2017, pp. 490-95.
- Borgwardt, Arne, et al. "A randomised, controlled clinical study on total hip arthroplasty using 4 different bearings: Results after 10 years."Hip International,Vol. 27, No. 1, 2017, pp. 96-103.
- van der Veen, Hugo C., et al. "Pseudotumours, cobalt and clinical outcome in small head metal-on-metal versus conventional metal-on-polyethylene total hip arthroplasty."Hip International,Vol. 30, No. 1, 2020, pp. 56-63.
- Vendittoli, P. A., et al. "Metal-on-metal hip resurfacing compared with 28-mm diameter metal-on-metal total hip replacement: A randomised study with six to nine years’ follow-up."The Bone and Joint Journal,Vol. 95, No. 11, 2013, pp. 1464-73.
- Higuchi, Yoshitoshi, et al. "Same survival but higher rate of osteolysis for metal-on-metal Ultamet versus ceramic-on-ceramic in patients undergoing primary total hip arthroplasty after 8 years of follow-up."Orthopaedics andTraumatology: Surgery and Research,Vol. 104, No. 8, 2018, pp. 1155-61.
- Desmarchelier, Romain, et al. "Metasul vs. Cerasul bearings: A prospective, randomized study at 9 years."The Journal of Arthroplasty,Vol. 28, No. 2, 2013, pp. 296-302.
- Bjorgul, K., et al. "High rate of revision and a high incidence of radiolucent lines around Metasul metal-on-metal total hip replacements: Results from a randomised controlled trial of three bearings after seven years."The Bone and Joint Journal,Vol. 95, No. 7, 2013, pp. 881-86.
- Zijlstra, Wierd P., et al. "No clinical difference between large metal-on-metal total hip arthroplasty and 28-mm-head total hip arthroplasty?"International Orthopaedics, Vol. 35, No. 12, 2011, pp. 1771-76.
- Engh Jr, Charles A., et al. "A prospective, randomized study of cross-linked and non-cross-linked polyethylene for total hip arthroplasty at 10-year follow-up."The Journal of Arthroplasty,Vol. 27, No. 8, 2012, pp. 2-7.
- Engh Jr, C. Anderson, et al. "A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked Marathon and non-cross-linked Enduron polyethylene liners."The Journal of Arthroplasty,Vol. 21, No. 6, 2006, pp. 17-25.
- Garcia-Rey, E., E. García-Cimbrelo, and A. Cruz-Pardos. "New polyethylenes in total hip replacement: A ten-to 12-year follow-up study."The Bone and Joint Journal,Vol. 95, No. 3, 2013, pp. 326-32.
- Nakahara, Ichiro, et al. "Minimum five-year follow-up wear measurement of longevity highly cross-linked polyethylene cup against cobalt-chromium or zirconia heads."The Journal of Arthroplasty,Vol. 25, No. 8, 2010, pp. 1182-87.
- Garcia-Rey, E., et al. "New polyethylenes in total hip replacement: a prospective, comparative clinical study of two types of liner."The Journal of Bone and Joint Surgery. British, Vol.90, No. 2, 2008, pp. 149-53.
- Morison, Zachary A., et al. "A randomized controlled trial comparing Oxinium and cobalt-chrome on standard and cross-linked polyethylene."The Journal of Arthroplasty,Vol. 29, No. 9, 2014, pp. 164-68.
- Langlois, J., et al. "A randomised controlled trial comparing highly cross-linked and contemporary annealed polyethylene after a minimal eight-year follow-up in total hip arthroplasty using cemented acetabular components."The Bone and Joint Journal, Vol. 97, No. 11, 2015, pp. 1458-62.
- Teeter, Matthew G., et al. "Thirteen-year wear rate comparison of highly crosslinked and conventional polyethylene in total hip arthroplasty: long-term follow-up of a prospective randomized controlled trial."Canadian Journal of Surgery,Vol. 60, No. 3, 2017, pp. 212-16.
- Devane, Peter A., et al. "Highly cross-linked polyethylene reduces wear and revision rates in total hip arthroplasty: A 10-year double-blinded randomized controlled trial."Journal of Bone and Joint Surgery,Vol. 99, No. 20, 2017, pp. 1703-14.
- Thomas, Geraint ER, et al. "The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: A double-blind, randomized controlled trial using radiostereometric analysis."Journal of Bone and Joint Surgery, Vol. 93, No. 8, 2011, pp. 716-22.
- Triclot, P., et al. "A comparison of the penetration rate of two polyethylene acetabular liners of different levels of cross-linking: A prospective randomised trial."The Journal of Bone and Joint Surgery. British, Vol.89, No. 11, 2007, pp. 1439-45.
- Li, Zhi, et al. "Comparative mid-term follow-up study of primary total hip arthroplasty with metal-on-metal and metal-on-polyethylene bearings."Orthopaedic Surgery,Vol. 10, No. 4, 2018, pp. 312-20.
- Geerdink, Carel H., et al. "Cross-linked compared with historical polyethylene in THA: An 8-year clinical study."Clinical Orthopaedics and Related Research,Vol. 467, No. 4, 2009, pp. 979-84.
- Atrey, A., et al. "Ten-year follow-up study of three alternative bearing surfaces used in total hip arthroplasty in young patients: A prospective randomised controlled trial."The Bone and Joint Journal,Vol. 99, No. 12, 2017, pp. 1590-95.
- Higuchi, Yoshitoshi, et al. "Significantly lower wear of ceramic-on-ceramic bearings than metal-on-highly cross-linked polyethylene bearings: A 10-to 14-year follow-up study."The Journal of Arthroplasty,Vol. 31, No. 6, 2016, pp. 1246-50.
- Marston, ROBERT A., ANDREW G. Cobb, and G. E. O. R. G. E. Bentley. "Stanmore compared with Charnley total hip replacement: A prospective study of 413 arthroplasties."The Journal of Bone and Joint Surgery. British, Vol.78, No. 2, 1996, pp. 178-84.
- Lombardi Jr, Adolph V., et al. "Short-term results of the M2a-taper metal-on-metal articulation."The Journal of Arthroplasty,Vol. 16, No. 8, 2001, pp. 122-28.
- Stihsen, Christoph, et al. "Migration of the Duraloc cup after 5 years."International Orthopaedics,Vol. 32, No. 6, 2008, pp. 791-94.
- Vendittoli, P-A., et al. "A prospective randomized clinical trial comparing metal-on-metal total hip arthroplasty and metal-on-metal total hip resurfacing in patients less than 65 years old."Hip International,Vol. 16, No. 4_suppl, 2006, pp. 73-81.
- Haddad, F. S., S. Konan, and J. Tahmassebi. "A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years: A ten-year follow-up."The Bone and Joint Journal,Vol. 97, No. 5, 2015, pp. 617-22.
- D’Antonio, James A., William N. Capello, and Marybeth Naughton. "Ceramic bearings for total hip arthroplasty have high survivorship at 10 years."Clinical Orthopaedics and Related Research®,Vol. 470, No. 2, 2012, pp. 373-81.
- Pitto, R. P., D. Blanquaert, and D. Hohmann. "Alternative bearing surfaces in total hip arthroplasty: zirconia-alumina pairing. Contribution or caveat?"Acta Orthopaedica Belgica,Vol. 68, No. 3, 2002, pp. 242-50.
- Ochs, U., et al. "Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating."Journal of Orthopedics and Trauma Surgery,Vol. 145, No. S 1, 2007, pp. S3-S8.
- Atrey, Amit, et al. "The ideal total hip replacement bearing surface in the young patient: A prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene: 15-year follow-up."The Journal of Arthroplasty,Vol. 33, No. 6, 2018, pp. 1752-56.
- Buttaro, Martin A., et al. "Primary total hip arthroplasty with fourth-generation ceramic-on-ceramic: Analysis of complications in 939 consecutive cases followed for 2-10 years."The Journal of Arthroplasty,Vol. 32, No. 2, 2017, pp. 480-86.
- Mesko, J. Wesley, et al. "Ceramic-on-ceramic hip outcome at a 5-to 10-year interval: Has it lived up to its expectations?"The Journal of Arthroplasty,Vol. 26, No. 2, 2011, pp. 172-77.
- Beaupre, Lauren A., Amro Al-Houkail, and Donald William C. Johnston. "A randomized trial comparing ceramic-on-ceramic bearing vs ceramic-on-crossfire-polyethylene bearing surfaces in total hip arthroplasty."The Journal of Arthroplasty,Vol. 31, No. 6, 2016, pp. 1240-45.
- Hamilton, William G., et al. "THA with Delta ceramic on ceramic: Results of a multicenter investigational device exemption trial."Clinical Orthopaedics and Related Research®,Vol 468, No. 2, 2010, pp. 358-66.
- D’Antonio, James A., et al. "A titanium-encased alumina ceramic bearing for total hip arthroplasty: 3-to 5-year results."Clinical Orthopaedics and Related Research®,Vol. 441, 2005, pp. 151-58.
- Capello, William N., et al. "Arc-deposited hydroxyapatite-coated cups: Results at four to seven years."Clinical Orthopaedics and Related Research®,Vol. 441, 2005, pp. 305-12.
- Lombardi, Adolph V., et al. "Delta ceramic-on-alumina ceramic articulation in primary THA: Prospective, randomized FDA-IDE study and retrieval analysis."Clinical Orthopaedics and Related Research®, Vol. 468, No. 2, 2010, pp. 367-74.
- Sobti, Anshul S., et al. "Early to mid-term outcome of Oxinium on Verilast highly cross-linked polyethylene bearing surface in uncemented total hip arthroplasty."HIP International,Vol. 29, No. 6, 2019, pp. 660-64.
- Silverman, Edward J., Blair Ashley, and Neil P. Sheth. "Metal-on-metal total hip arthroplasty: Is there still a role in 2016?"Current Reviews in Musculoskeletal Medicine,Vol. 9, No. 1, 2016, pp. 93-96.
- Dumbleton, John H., and Michael T. Manley. "Metal-on-metal total hip replacement: What does the literature say?"The Journal of Arthroplasty,Vol. 20, No. 2, 2005, pp. 174-88.
- Liow, Ming Han Lincoln, and Young-Min Kwon. "Metal-on-metal total hip arthroplasty: Risk factors for pseudotumours and clinical systematic evaluation."International Orthopaedics,Vol. 41, No. 5, 2017, pp. 885-92.
- Daniel, J., P. B. Pynsent, and D. J. W. McMinn. "Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis."The Journal of Bone and Joint Surgery. British, Vol.86, No. 2, 2004, pp. 177-84.
- Ziaee, H., et al. "Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: A controlled study."The Journal of Bone and Joint Surgery. British, Vol.89, No. 3, 2007, pp. 301-05.
- Campbell, Pat, Fu-Wen Shen, and Harry McKellop. "Biologic and tribologic considerations of alternative bearing surfaces."Clinical Orthopaedics and Related Research®,Vol. 418, 2004, pp. 98-111.
- Kurtz, Steven M., Heather A. Gawel, and Jasmine D. Patel. "History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene."Clinical Orthopaedics and Related Research®,Vol. 469, No. 8, 2011, pp. 2262-77.
- Di Puccio, Francesca, and Lorenza Mattei. "Biotribology of artificial hip joints."World Journal of Orthopedics,Vol. 6, No. 1, 2015, pp. 77-94.
- Kurtz, Steven M., et al. "Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study."Clinical Orthopaedics and Related Research®,Vol. 471, No. 10, 2013, pp. 3270-82.
- Garvin, Kevin L., et al. "Low wear rates seen in THAs with highly crosslinked polyethylene at 9 to 14 years in patients younger than age 50 years."Clinical Orthopaedics and Related Research®,Vol. 473, No. 12, 2015, pp. 3829-35.
- Fisher, John, et al. "Presidential guest lecture: Tribology of alternative bearings."Clinical Orthopaedics and Related Research®,Vol. 453, 2006, pp. 25-34.
- Lim, Seung-Jae, et al. "High survivorship of highly cross-linked polyethylene in revision total hip arthroplasty: A minimum 10-year follow-up study."Arthroplasty,Vol. 1, No. 1, 2019, pp. 1-7.
- Nich, Christophe, and Stuart B. Goodman. "Role of macrophages in the biological reaction to wear debris from joint replacements."Journal of Long-Term Effects of Medical Implants,Vol. 24, No. 4, 2014, pp. 259-65
- McCalden, Richard W., et al. "Wear rate of highly cross-linked polyethylene in total hip arthroplasty: A randomized controlled trial."Journal of Bone and Joint Surgery,Vol. 91, No. 4, 2009, pp. 773-82.
- García-Rey, Eduardo, and Eduardo García-Cimbrelo. "Polyethylene in total hip arthroplasty: Half a century in the limelight."Journal of Orthopaedics and Traumatology,Vol. 11, No. 2, 2010, pp, 67-72.
- Jacobs, Cale A., et al. "Clinical performance of highly cross-linked polyethylenes in total hip arthroplasty."Journal of Bone and Joint Surgery,Vol. 89, No. 12, 2007, pp. 2779-86.
- Fawsitt, Christopher G., et al. "Choice of prosthetic implant combinations in total hip replacement: Cost-effectiveness analysis using UK and Swedish hip joint registries data."Value in Health,Vol. 22, No. 3, 2019, pp. 303-12.
- Carnes, Keith J., et al. "Cost analysis of ceramic heads in primary total hip arthroplasty."Journal of Bone and Joint Surgery,Vol. 98, No. 21, 2016, pp. 1794-1800.
- Im, Chulsoon, et al. "Revision total hip arthroplasty after ceramic bearing fractures in patients under 60-years old; mid-term results."Hip and pelvis,Vol. 30, No. 3, 2018, pp. 156-61.
- Jarrett, Christopher A., et al. "The squeaking hip: A phenomenon of ceramic-on-ceramic total hip arthroplasty."Journal of Bone and Joint Surgery,Vol. 91, No. 6, 2009, pp. 1344-49.
- Levy, Yadin David, et al. "Review on squeaking hips."World Journal of Orthopedics,Vol. 6, No. 10, 2015, pp. 812-20.
- Ecker, T. M., et al. "Squeaking in total hip replacement: No cause for concern."Orthopedics,Vol. 31, No. 9, 2008, pp. 875-76.
- Lachiewicz, Paul F., Lindsay T. Kleeman, and Thorsten Seyler. "Bearing surfaces for total hip arthroplasty."JAAOS-Journal of the American Academy of Orthopaedic Surgeons,Vol. 26, No. 2, 2018, pp. 45-57.
- Gallo, Jiri, et al. "Advantages and disadvantages of ceramic on ceramic total hip arthroplasty: A review."Biomedical Papers,Vol. 156, No. 3, 2012, pp. 204-12.
- Dong, Yu-Lei, et al. "Ceramic on ceramic or ceramic-on-polyethylene for total hip arthroplasty: A systemic review and meta-analysis of prospective randomized studies."Chinese Medical Journal,Vol. 128, No. 9, 2015, pp. 1223-31.
- Prokopetz, Julian JZ, et al. "Risk factors for revision of primary total hip arthroplasty: A systematic review."BMC Musculoskeletal Disorders,Vol. 13, No. 1, 2012, pp. 1-13.
- Liu, Kuan-Lin, et al. "When and how do prosthetic hips fail after total hip arthroplasties?-A retrospective study."Journal of the Formosan Medical Association,Vol. 115, No. 9, 2016, pp. 786-93.
- Abdulkarim, Ali, et al. "Cemented versus uncemented fixation in total hip replacement: A systematic review and meta-analysis of randomized controlled trials."Orthopedic Reviews,Vol. 5, No. 1, 2013, p. e8.
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). "Hip, knee & shoulder arthroplasty - Annual Report 2018." 2018. https://aoanjrr.sahmri.com/documents/10180/576950/Hip%2C%20Knee%20%26%20Shoulder%20Arthroplasty