Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 2
Diabetes in Children and Adolescents in Saudi Arabia: Systematic Review
Nazim Faisal Hamed Ahmed1*, Awad Alqahtani1, Badriah Abdulrahamn Alsabah2, Areej Mohammed Alatawi2 and Aljawharah Ibrahim Alghuraydh22Resident of Pediatrics, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia
Nazim Faisal Hamed Ahmed, Consultant of Pediatrics Endocrine, King Fahd Specialized Hospital, Tabuk, Saudi Arabia, Tel: 8001277000, Email: nagah_aboelfotooh@med.sohag.edu.eg
Received: 30-Dec-2020 Accepted Date: Feb 11, 2021 ; Published: 18-Feb-2021
Abstract
Background: Diabetes is widely recognized as an emerging epidemic that has a growing influence on almost every country, age group, and economy across the world. Children and adolescents have gained attention lately due to the increasing prevalence of both types’ diabetes mellitus. Aim: To highlight the prevalence, risk factors, and complications of both types of diabetes among Saudi children and to compare Saudi results to international results. Methodology: This is a systematic review was carried out, including PubMed, Google Scholar, and EBSCO that examining randomized controlled trials, observational, and experimental studies which study diabetes in children and adolescent in Saudi Arabia. Results and Conclusion: Findings of previous studies indicate a growing prevalence of T1DM and T2DM among children and adolescents. More attention should be paid to this catastrophe as risk factors should be controlled as possible. Health education to mothers and caregivers of children and adolescents with increased risk for developing diabetes mellitus should be done through health campaigns and conferences.
Keywords
Prevalence, Diabetes, T1DM, T2DM, Children, Adolescents, Saudi Arabia
Introduction
Genetic and environmental contributions lead to immune-mediated loss of beta-cell function resulting in hyperglycemia and life-long insulin dependence in children known as type 1 diabetes. Type 1 diabetes may be diagnosed at nearly any age, though peaks in presentation occur between ages 5 to 7 and around puberty [1]. Type 2 diabetes mellitus is a metabolic disorder characterized by peripheral insulin resistance and a failure of beta cells to compensate, leading to hyperglycemia [2]. Type 2 diabetes mellitus is estimated to occur in one in three (20% to 33%) of new diagnoses of diabetes in children today. The rate of type 2 diabetes mellitus in children continues to rise even as the obesity rates have plateaued in these age groups [3].
Factors contributing to insulin resistance include obesity/sedentary lifestyle, race/ethnicity, and family history. Puberty is another important factor leading to the development of T2DM. A hyperglycemic clamp study showed that both early and late responses to hyperglycemia were enhanced during puberty (leading to hyperinsulinemia). Childhood obesity has more than doubled in children and quadrupled in adolescents in the past 30 years. A strong link between obesity, insulin resistance, and metabolic syndrome has been reported. Bogalusa Heart Study showed that children with parental DM had a higher Body Mass Index (BMI) and increased Systolic Blood Pressure (SBP) from childhood, increased fasting insulin and glucose and insulin resistance index from puberty, increased Triglycerides (TGs), and low-density lipoprotein, and decreased High-Density Lipoprotein (HDL) in adulthood [4-6].
DM is associated with serious complications, but the early diagnosis and initiation of therapy may prevent or delay the onset of long-term complications [7]. Cataracts, retinopathy, gastroparesis, renal failure, hypertension, premature coronary disease, peripheral vascular disease, neuropathy, and increased susceptibility to infections are complications of diabetes in children [8].
Continuous Glucose Monitoring (CGM) has become more common in children and adolescents, and measures of “time in range” and glucose variability are likely to be even more valuable than Hemoglobin A1c, although insurance does not universally cover CGM and is not always desired by patients [9]. All patients and their families need com-prehensive education about the disease and its potential complications. Also, all diabetics should be referred to an ophthalmologist, nephrologist, cardiologist, and neurologist for baseline workup of their respective organ systems [10].
Aim of the Study
To highlight the prevalence, risk factors, and complications of both types of diabetes among Saudi children and to compare Saudi results to international results.
Methodology
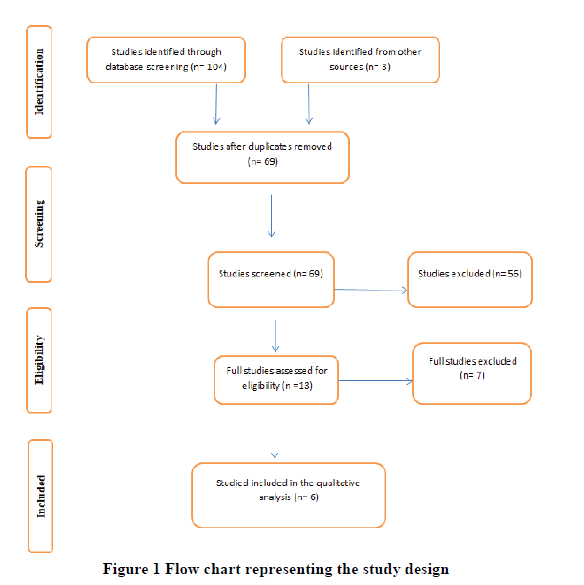
A systematic review was carried out, including PubMed, Google Scholar, and EBSCO using the following terms in different combinations: diabetes in children and adolescents, childhood diabetes, diabetes in Saudi children, diabetes in Saudi adolescents. We included all full texts randomized controlled trials, observational, and experimental studies in the English language. The authors extracted the data, and then the author’s names, year and region of publication, the study type, period of study, and the result were reported (Table 1).
Statistical Analysis
No software has been utilized to analyze the data. The data was extracted based on a specific form that contains (Author’s name, publication year, country, methodology, and results). These data were reviewed by the group members to determine the initial findings and the modalities of performing the surgical procedure. Double revision of each member’s outcomes was applied to ensure validity and minimize the mistakes.
Results
The search of the mentioned databases returned a total of 107 studies that were included for title screening. 69 of them were included for abstract screening, which leads to the exclusion of 56 articles. The remaining 13 publications full-texts were reviewed. The full-text revision leads to the exclusion of 7 studies, and 6 were enrolled for final data extraction (Table 1).
| Author, Year, Region | Study type, Objective | Outcomes |
|---|---|---|
| Al-Rubeaan K. [11] Saudi Arabia | A population-based study included 23 523 children to assess the prevalence of type 1 and type 2 diabetes as well as Impaired Fasting Glucose (IFG) among children and adolescents. | Prevalence of type 1 diabetes was 10.84%, 0.45% type 2 diabetes age, male gender, obesity, urban residency, high family income, and presence of dyslipidemia were found to be significant risk factors for diabetes. |
| Aqeel A. Alaqeel [12] Saudi Arabia | The review summarizes the pediatric and adolescent diabetes studies in Saudi Arabia to date and explores the country-specific treatment challenges and potential solutions. | Prevalence of the disease and DKA incidence at diagnosis is hugely variable in each region. There is a lack of screening programs and programs to increase awareness of T1D, and a lack of clinical trials and multicenter research collaboration. |
| Robert, Asirvatham Alwin, et al. [13] Saudi Arabia | Review article aimed to discuss different aspects of T1DM in Saudi Arabia drawing on the published literature currently available. | 35,000 children and adolescents in Saudi Arabia suffer from T1DM, which makes Saudi Arabia ranked the 8th in terms of numbers of TIDM patients and 4th country in the world in terms of the incidence rate (33.5 per 100,000 individuals) of TIDM. |
| Ghandoora MM [14] Saudi Arabia | A systematic search of published literature that has addressed T1DM in pediatrics and adolescents was carried out to shed more lights on T1DM among Pediatrics and Adolescent patients | The number of children with T1DM in KSA is 16,100 cases. The incidence rate is growing by 3% yearly and Saudi Arabia ranked as 5th in incidence rate. |
| Al-Mendalawi M [15] Saudi Arabia | Comment | The total number of cases of type 1 DM in children under the age of 12 years was 22 with an estimated prevalence of 106.7/100,000. |
| Alghamdi AH [16] Saudi Arabia | A prospective study included 372 children to describe and compare the epidemiological criteria of children with diabetes from 2007 to 2014. | The year 2012 had the highest incidence rate, with 59 children and adolescents affected at an incidence rate of 25.48/100000. Al-Baha region had the highest number of cases constituting 37.7 % of cases. Diabetic ketoacidosis was the first presentation and constituted 44.2% of cases. |
| AlBuhairan F, et al. [17] Saudi Arabia | A cross-sectional study was conducted involving 315 adolescent to measure the health-related quality of life among Saudi Arabian adolescents with T1DM | Mean HRQoL score of 64.8, Female gender, and late adolescent age were predictors of lower HRQoL for adolescents with T1DM. |
| Alanazi KM, et al. [18] Saudi Arabia | A cross-sectional study to estimate the prevalence of type I diabetes and to describe some related characteristics of cases in a sample of adolescent primary and secondary school girls | The prevalence of type I diabetes among the studied adolescent girls was 5.2% with the Mean (± SD) age was 14.08 (± 3.4). All diabetic girls were Saudi. Only 25% of the cases were using hormonal contraception. |
Table 1: Author, country, year of publication, region, study type, objective, and outcomes
The included studies had different study designs.
Al-Rubeaan K concluded that diabetes and IFG are highly prevalent in this society with the majority of the patients being unaware of their disease, which warrants urgent adoption of early detection, treatment, and prevention programs [11].
Aqeel A. Alaqeel reported that; the main challenges in treating children and adolescents with diabetes in Saudi Arabia are a lack of patient and parent awareness of T1D and its complications, poor psychosocial support, limited resources for school support, and poor self-management techniques [12].
Robert, Asirvatham Alwin, et al. considering the increasing prevalence of T1DM in Saudi Arabia, especially in infants and young children, the research interventions need to be significantly improved [13]. Moreover, it is critical to developing appropriate management programs for controlling T1DM and allocating health resources appropriately for this traumatic condition.
Ghandoora MM found that; the clinical presentation at diagnosis includes polydipsia, polyuria, and weight loss with a high incidence of DKA [14]. T1DM is commonly associated with autoimmune thyroiditis and coeliac disease. T1DM is associated also with disturbance of lung function, hepatopathy, and vitamin D deficiency among the T1DM population.
Alghamdi AH reported that; diabetes in children is increasing significantly in recent years, requiring more detailed analysis of its epidemiological factors to find out any significant correlations which may help in its prevention [16].
AlBuhairan F, et al. findings emphasize the importance of an interdisciplinary, biopsychosocial, and family-centered care approach to adolescents with a chronic disease [17].
Discussion
Few community-based surveys are looking into the prevalence of type 1 and type 2 diabetes concurrently among children and adolescents worldwide [19,20]. Internationally, more than 96,000 children and adolescents aged less than 15 years develop T1DM each year, and 13%-80% of them present with DKA at the time of diagnosis [21,22]. A nationwide Saudi Arabian survey reported that the prevalence rate identified was 109.5 per 100,000 children and adolescents (highest in the central region (126 cases per 100,000; mostly urban) and lowest in the Eastern region (48 cases per 100,000; mostly rural) of Saudi Arabia) [23]. Other studies’ estimates indicated the prevalence of 586,000 children aged less than 15 years with T1DM worldwide, with the highest percentages in Europe and North America [21,24]. Al-Rubeaan, who conducted a study in Saudi Arabia reported that (77.2%) of cases of T1DM were documented in urban rather than rural areas (22.7%) [11]. Another Saudi study reported that the incidence of T1DM in Saudi children was 27.5 per 100,000 and 29 per 100,000, higher than several other countries [25,26].
Regarding risk factors; a study in Riyadh among children reported that 64% were overweight or obese, 34% had a sign of insulin-resistance such as acanthosis nigricans, 57% were found to have a family history of DM, and only 52% were shown to have positive pancreatic antibodies. Additionally, in follow-up, 46% of the patients were managed solely on metformin. All of these factors are likely to indicate T2D or double diabetes [27]. Also; age ≥ 13 years revealed a major risk factor for abnormal glucose metabolism in a previous Taiwanese study. This could be supported by the growing evidence that puberty is associated with increased insulin resistance as proved by other epidemiological studies when looking for hyperinsulinemia in pubertal-age adolescents [28]. A study screening for diabetes in 23,523 children 6-18 years of age from 2007 to 2009 confirmed that 0.07% were known to have T2D while 4.27% were established incidentally to have diabetes based on fasting blood glucose >125 mg/dL which were likely to be T2D based on associated findings such as for overweight, family history, and signs of metabolic syndrome. The study was limited in that enrolled participants might not have adhered to the instructions of strict overnight fasting for the diagnostic blood glucose test [11]. Another study reported that the male gender was also found to be a significant risk factor for this age group. This finding contradicts the observation in other ethnicities like Taiwanese, Native American, and Jamaican, which could either be the result of the ethnicity effect or the significantly increased prevalence of obesity among males in this cohort [29-31].
The most commonly reported complications are retinopathy, nephropathy, neuropathy, and cardiovascular disease. The Diabetes Control and Complications Trial (DCCT) confirmed that diabetic patients on intensive insulin therapy had better glycemic control and significantly lower complication rates than those on conventional therapy. Intensive therapy reduced retinopathy by 76%, microalbuminuria by 39%, and neuropathy by 60% [32]. One study found a 65.4% correlation between DKA and inadequate glycemic control and a 68.9% correlation between hypoglycemia episodes and poor glycemic control. However, hypoglycemia decreased with higher HbA1c [33]. The highest frequencies for DKA at the presentation of T1DM are seen in Saudi Arabia (44.9%) and the United Arab Emirates (80%) [34,35]. A cross-sectional study in Jeddah of 228 children and adolescents with T1D showed the association of dyslipidemia (8.3%) and microalbuminuria (16.2%) with poor glycemic control while retinopathy was not related to HbA1c (4.4%) [36]. In Saudi Arabia, a study examined 218 adults with T1DM at a large center and found a 7.3% prevalence of the celiac disease in them [37]. A study in Riyadh demonstrated lower academic performance in T1D patients compared to healthy students and claimed that this was due to cognitive impairment secondary to DM, but further studies are required to confirm this finding [38]. Other studies also reported a prevalence of the celiac disease in patients with T1DM in Saudi Arabia to be 4.8%-11.3% [39]. A study of 103 adolescents with established T1D in one center in Riyadh showed that 54.4% had one episode of DKA, 39.8% had two episodes, and 5.8% had three episodes [40]. A study undertaken in different regions of Saudi Arabia reported that in the southern region 10.4%, in the central region 11.3%, and western region 11.2% of patients with T1DM possess celiac disease [41]. A meta-analysis review of data for 26,605 patients projected a worldwide prevalence of the biopsy-proven celiac disease among T1DM to be 6%. However, an extensive variation was noted as in France it was 1.6%, in USA 4.6%-7.0%, in Italy 3.6%-6.6%, in Sweden 9%-9.7%, and in the United Kingdom 3.3%-4.0%. This variation could be attributed to the duration of the disease and the age at diagnosis, in addition to genetic susceptibility [42].
Conclusion
Findings of previous studies indicate a growing prevalence of T1DM and T2DM among children and adolescents. More attention should be paid to this catastrophe as risk factors should be controlled as possible. Health education to mothers and caregivers of children and adolescents with increased risk for developing diabetes mellitus should be done through health campaigns and conferences. Physicians should also consider screening for this age group to early diagnose and manage these patients to limit further complications.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Insel, Richard A., et al. "Staging presymptomatic type 1 diabetes: A scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association."Diabetes Care,Vol. 38, No. 10, 2015, pp. 1964-74.
- Chen, Yong, et al. "Prevalence of type 1 and type 2 diabetes among US pediatric population in the MarketScan Multi-State Database, 2002 to 2016."Pediatric Diabetes,Vol. 20, No. 5, 2019, pp. 523-29.
- Jensen, Elizabeth T., and Dana Dabelea. "Type 2 diabetes in youth: New lessons from the SEARCH study."Current Diabetes Reports,Vol. 18, No. 6, 2018, pp. 1-7.
- National Center for Health Statistics (US). "Health, United States, 2011: With special feature on socioeconomic status and health." 2012.
- Ogden, Cynthia L., et al. "Prevalence of childhood and adult obesity in the United States, 2011-2012."JAMA,Vol. 311, No. 8, 2014, pp. 806-14.
- Krebs, Nancy F., et al. "Assessment of child and adolescent overweight and obesity."Pediatrics,Vol. 120, No. Supplement 4, 2007, pp. S193-S228.
- Lee, Yung Seng, Jimmy BY So, and Mabel Deurenberg-Yap. "Confronting the obesity epidemic: Call to arms."Annals Academy of Medicine,Vol. 38, No. 1, 2009, pp. 1-2.
- American Diabetes Association. "Adverse events and their association with treatment regimens in the diabetes control and complications trial."Diabetes Care,Vol. 18, No. 11, 1995, pp. 1415-27.
- Dabelea, Dana, et al. "Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009."JAMA,Vol. 311, No. 17, 2014, pp. 1778-86.
- Al-Hakami, Ahmed M. "Pattern of thyroid, celiac, and anti-cyclic citrullinated peptide autoantibodies coexistence with type 1 diabetes mellitus in patients from Southwestern Saudi Arabia."Saudi Medical Journal,Vol. 37, No. 4, 2016, pp. 386-91.
- Al-Rubeaan, Khalid. "National surveillance for type 1, type 2 diabetes and prediabetes among children and adolescents: A population-based study (SAUDI-DM)."Journal of Epidemiology and Community Health,Vol. 69, No. 11, 2015, pp. 1045-51.
- Alaqeel, Aqeel A. "Pediatric diabetes in Saudi Arabia: Challenges and potential solutions. A review article."International Journal of Pediatrics and Adolescent Medicine,Vol. 6, No. 4, 2019, pp. 125-30.
- Robert, Asirvatham Alwin, et al. "Type 1 diabetes mellitus in Saudi Arabia: A soaring epidemic."International Journal of Pediatrics,Vol. 2018, 2018.
- Ghandoora, M. M., et al. "Type 1 diabetes mellitus among pediatrics and adolescents in Saudi Arabia: A systematic review."International Journal of Advanced Research,Vol. 5, No. 2, 2017, pp. 1352-58.
- Al-Mendalawi, Mahmood D., and Abdullah Al-Herbish. "Prevalence of type 1 diabetes mellitus in Saudi Arabian children and adolescents."Saudi Medical Journal,Vol. 30, No. 2, 2009, pp. 310-11.
- Alghamdi, Ahmed H., et al. "Trends of diabetes in children and adolescents in pediatric endocrinology clinic and clinical pediatric diabetes center at Al Baha central hospital in Saudi Arabia."Journal of Preventive Medicine and Care,Vol. 1, No. 3, 2016, pp. 09-21.
- AlBuhairan, Fadia, et al. "Health related quality of life and family impact of type 1 diabetes among adolescents in Saudi Arabia."Diabetes Research and Clinical Practice,Vol. 114, 2016, pp. 173-79.
- Alanazi, Khulud Falah M., et al. "Type 1 Diabetes Mellitus among Adolescent Girls in Riyadh City, Saudi Arabia."The Egyptian Journal of Hospital Medicine,Vol. 70, No. 3, 2018, pp. 458-63.
- Zimmet, Paul, K. G. M. M. Alberti, and Jonathan Shaw. "Global and societal implications of the diabetes epidemic."Nature,Vol. 414, No. 6865, 2001, pp, 782-87.
- Amed, Shazhan, et al. "Type 2 diabetes in children and adolescents."Expert Review of Cardiovascular Therapy,Vol. 8, No. 3, 2010, pp. 393-406.
- Atlas, IDF Diabetes. "Brussels, Belgium: International diabetes federation; 2013."International Diabetes Federation (IDF),2017, p. 147.
- Usher-Smith, J. A., et al. "Variation between countries in the frequency of diabetic ketoacidosis at first presentation of type 1 diabetes in children: A systematic review."Diabetologia,Vol. 55, No. 11, 2012, pp. 2878-94.
- Al-Herbish, Abdullah S., et al. "Prevalence of type 1 diabetes mellitus in Saudi Arabian children and adolescents."Saudi Medical Journal,Vol. 29, No. 9, 2008, pp. 1285-88.
- Patterson, Chris, et al. "Diabetes in the young-a global view and worldwide estimates of numbers of children with type 1 diabetes."Diabetes Research and Clinical Practice,Vol. 103, No. 2, 2014, pp. 161-75.
- Abduljabbar, Mohammad A., et al. "Incidence trends of childhood type 1 diabetes in eastern Saudi Arabia."Saudi Medical Journal,Vol. 31, No. 4, 2010, pp. 413-18.
- Habeb, Abdelhadi M., et al. "High incidence of childhood type 1 diabetes in Al-Madinah, North West Saudi Arabia (2004-2009)."Pediatric Diabetes,Vol. 12, No. 8, 2011, pp. 676-81.
- Braham, Rim, et al. "Double diabetes in Saudi Arabia: A new entity or an underestimated condition."World Journal of Diabetes,Vol. 7, No. 20, 2016, pp. 621-26.
- Wei, Jung-Nan, et al. "National surveillance for type 2 diabetes mellitus in Taiwanese children."JAMA,Vol. 290, No. 10, 2003, pp. 1345-50.
- Caprio, Sonia, et al. "Increased insulin secretion in puberty: A compensatory response to reductions in insulin sensitivity."The Journal of Pediatrics,Vol. 114, No. 6, 1989, pp. 963-67.
- Dabelea, D., et al. "Increasing prevalence of type II diabetes in American Indian children."Diabetologia,Vol. 41, No. 8, 1998, pp. 904-10.
- Barrett, Sheila C., et al. "A cross-sectional study of Jamaican adolescents’ risk for type 2 diabetes and cardiovascular diseases."BMJ Open,Vol. 3, No. 7, 2013, pp. 1-9.
- Diabetes Control and Complications Trial Research Group. "The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus."New England Journal of Medicine,Vol. 329, No. 14, 1993, pp. 977-86.
- Al-Fifi, Suliman H. "Intensive insulin treatment versus conventional regimen for adolescents with type 1 diabetes, benefits and risks."Saudi Medical Journal,Vol. 24, No. 5, 2003, pp. 485-87.
- Ahmed, Ahmed M., et al. "Reduced frequency and severity of ketoacidosis at diagnosis of childhood type 1 diabetes in Northwest Saudi Arabia."Journal of Pediatric Endocrinology and Metabolism,Vol. 29, No. 3, 2016, pp. 259-64.
- Shaltout, Azza Aly, et al. "Ketoacidosis at first presentation of type 1 diabetes mellitus among children: A study from Kuwait."Scientific Reports,Vol. 6, No. 1, 2016, pp. 1-9.
- Al-Agha, Abdulmoein E., Maram Alafif, and Ihab A. Abd-Elhameed. "Glycemic control, complications, and associated autoimmune diseases in children and adolescents with type 1 diabetes in Jeddah, Saudi Arabia."Saudi Medical Journal,Vol. 36, No. 1, 2015, pp. 26-31.
- Alshareef, M. A., et al. "The prevalence of celiac disease in Saudi patients with type 1 diabetes mellitus: Cross sectional study."International Journal of Diabetes and Metabolic Disorders,Vol. 1, No. 1, 2016, pp. 1-4.
- Meo, Sultan Ayoub, et al. "Impact of type 1 diabetes mellitus on academic performance."Journal of International Medical Research,Vol. 41, No. 3, 2013, pp. 855-58.
- Al-Hussaini, Abdulrahman, et al. "High prevalence of celiac disease among Saudi children with type 1 diabetes: A prospective cross-sectional study."BMC Gastroenterology,Vol. 12, No. 1, 2012, pp. 1-7.
- Al-Hayek, Ayman A., et al. "Frequency and associated risk factors of recurrent diabetic ketoacidosis among Saudi adolescents with type 1 diabetes mellitus."Saudi Medical Journal,Vol. 36, No. 2, 2015, pp. 216-20.
- Saadah, Omar I., et al. "Prevalence of celiac disease in children with type 1 diabetes mellitus screened by anti-tissue transglutaminase antibody from Western Saudi Arabia."Saudi Medical Journal,Vol. 33, No. 5, 2012, pp. 541-46.
- Elfström, P., Johan Sundström, and Jonas F. Ludvigsson. "Systematic review with meta-analysis: associations between coeliac disease and type 1 diabetes."Alimentary Pharmacology and Therapeutics,Vol. 40, No. 10, 2014, pp. 1123-32.