Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
Detection of Lymphocyte Subsets and Inflammatory Cytokines in Mild and Severe COVID-19 Patients
Samah M Fathy1* and Mona I Ahmed22Chest diseases and tuberculosis Department, Fayoum University, Fayoum, Egypt
Samah M Fathy, Zoology Department, Fayoum University, Fayoum, Egypt, Email: smm01@fayoum.edu.eg
Received: 25-Nov-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021, DOI: O
Abstract
Background and objectives: The pandemic Coronavirus Disease 2019 (COVID-19) is the most threatening infectious disease nowadays that affecting people’s health worldwide. The disease symptoms were attributed to infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The current article aimed to discriminate different lymphocyte subtypes and pro-inflammatory mediators in COVID-19 patients with an emphasis on variations in their levels in mild and severely infected individuals that might help in the disease early intervention. Subjects and methods: The count of the Cluster of Differentiation (CD)3+ T, CD4+ T, CD8+ T cells, B lymphocytes, and Natural Killer (NK) cells were measured in the blood of healthy control and COVID-19 people with mild and severe symptoms using a flow cytometer. The plasma levels of Nuclear Factor kappa B (NF-κB), Tumor Necrosis Factor-α (TNF-α), Interleukin (IL)-6, IL-1β, IL-8, Procalcitonin (PCT), and Platelet-Activating Factor (PAF) were also detected by Enzyme-Linked Immunosorbent Assay (ELISA). Results: Total lymphocyte count and lymphocyte subsets significantly decreased in the blood of COVID-19 patients with more decrements in severely infected patients. The inflammatory markers levels remarkably increased in COVID-19 patients with higher increments in severe COVID-19 infected patients. Conclusion: In conclusion, the reduced level of the lymphocyte subsets and the induced pro-inflammatory response were vital signs that were concomitant with COVID-19. Besides, they were associated with the severity of the disease.
Keywords
COVID-19, Lymphocyte subsets, Pro-inflammatory response, SARS-CoV-2
Introduction
Wuhan is a city in China where Coronavirus Disease 2019 (COVID-19) started and spread into other cities and countries all over the world [1,2]. COVID-19 was recognized by The World Health Organization (WHO) as a pandemic disease on 11 March 2020 [3]. It has been grouped with other acute respiratory syndromes into Class B infectious diseases as described by the Law of the People’s Republic of China on Prevention and Treatment of Infectious Diseases. However, it was dealt with as a Class A infectious disease [4]. The etiology for COVID-19 is due to infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [5]. The infection spread from the newly infected or the asymptomatic infected individuals via close contact and respiratory droplets [4].
Despite the genetic manifestations of SARS-CoV-2 are crucially different from Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV), most information about COVID-19 was extracted from studies about SARS and MERS [4,5]. Acute Respiratory Distress Syndrome (ARDS) by lung biopsy as a result of cytokines infiltration was proven in SARS and MERS patients [5]. Similarly, ARDS was observed in lung biopsy of COVID-19 patients hypothesizing that the secretion of an extensive amount of different pro-inflammatory cytokines and chemokines as the main predisposition for ARDS, multiple organ failure, and possible death at the end [3]. However, cytokines and chemokines’ types are different from those released in SARS and MERS patients [6,7].
The plasma of COVID-19 patients exhibited higher levels of interleukin (IL)-7, IL-10, IL-2, interferon γ-Inducible Protein (IP)10, Granulocyte-Colony Stimulating Factor (GSCF), Monocyte Chemoattractant Protein (MCP)1, Tumor Necrosis Factor (TNF)-α, Macrophage Inflammatory Protein (MIP)1A, IL-6, serum ferritin, and C-Reactive Protein (CRP) [2,8].
Moreover, lymphopenia as a consequence of lymphocytes’ apoptosis attributed to the excessive release of cytokines is a salient feature in COVID-19 patients and might be ascribed with the severity of symptoms with eventual death [2,8,9]. A report study has shown a remarkable decline of the Cluster of Differentiation (CD)4+ and CD8+ T cells’ number in the peripheral blood of a SARS-CoV-2-infected patient [5]. Another recent study proved a significant reduction of all lymphocyte subtypes in severe COVID-19 patients [3].
The present study objective was to characterize different lymphocyte subsets and inflammatory agents in COVID-19 patients. We also aimed to highlight the variation in the inflammatory response associated with mild and severe SARSCoV- 2 infection as a trial for the detection of clues that may help in the early intervention for COVID-19 patients.
Material and Methods
Patients and Samples
36 patients (20 male and 16 female, age from 31-59) were suspected of COVID-19 disease and were assured by Real- Time fluorescent RT-PCR. The patients attended Fayoum University Hospital and were enrolled in the current study. They were classified into mild and severe pneumonia (with 18 patients in each group) by following the Diagnosis and Treatment Protocol of New Coronavirus Pneumonia (trial version 7) from the National Health Commission of China [4]. Moreover, 36 normal individuals with matching age and sex were chosen as the control group.
Patients with mild infection were enrolled with a low fever, respiratory rate from (20-25) breaths/min, and good pulmonary imaging. On the contrary, patients with severe viral infection were suffering from fever or respiratory symptoms with imaging findings of viral pneumonia, in addition to one or both of the following signs: respiratory rate >30 breaths/min and their pulmonary imaging progress >50% in (24-48) hours.
The full history of patients had been taken. Seven patients who had type 2 diabetes and ten had hypertension were included in the present research. All patients with a previous history of tumors, autoimmune diseases, or hematologic disorders were excluded from the current study.
This study was approved by the Medical Ethics Committee of the Faculty of Medicine, Fayoum University. All participants were asked to give written informed consent, and the study was carried out following the Declaration of Helsinki.
Detection of Lymphocyte Subset Count by Flow Cytometer
Collection of the patients’ whole blood was performed in Ethylene Diamine Tetra Acetic Acid (EDTA) coated tubes. The hemocytometer was used to detect the total number of lymphocytes in peripheral blood. The percentages of different lymphocytes’ subsets among the total lymphocytes were detected using Canto I flow cytometer (Becton Dickinson, New Jersy, USA). First, dilution of 100 μl of whole blood with 400 μl of IMDM medium was performed. Afterward, different antibodies (Peridinin Chlorophyll protein complex (PerCp)-conjugated Monoclonal Antibodies (MAb) to CD3, Fluorescein Isothiocyanate (FITC)-conjugated MAb to CD4 and CD16, Phycoerythrin (PE)-conjugated MAb to CD8, CD19, and CD56) were prepared based on the manufacturer’s instructions (Beckman Coulter Electronics, Hialeah, FL) and were incubated with whole blood for 5 min at 25°C. Lysis and fixation of the cells were carried out as described by the protocol’s instructions then they were kept at 4°C for 24 h before the cells were analyzed by the flow cytometer.
The absolute number of each lymphocyte subset was determined by multiplying the percentage of each subset by the total count of lymphocytes (CD4+ T lymphocytes count=total lymphocyte count × CD3+CD4+CD8-%, CD8+ T lymphocytes count=total lymphocyte count × CD3+CD4-CD8+%, B lymphocytes count=total lymphocyte count × CD3- CD19+%, NK cell count=total lymphocyte count × CD3-CD16+CD56+%).
Determination of Inflammatory Cytokines by Enzyme-Linked Immunosorbent Assay (ELISA)
The protein level of nuclear factor kappa B (NF-κB), TNF-α, IL-1β, IL-6, IL-8, Procalcitonin (PCT), and Platelet- Activating Factor (PAF) were detected in plasma by ELISA kits (Merck Millipore, San Francisco, California, USA) by following the manufacturer’s protocol. Protein levels were estimated using the microplate ELISA reader at 450 nm.
Statistical Analysis
Statistical analyses were achieved using GraphPad PRISM (version 6.01; Graph Pad Software, USA). Data were expressed as the mean ± SD and analyzed using an unpaired t-test. Differences were considered significant at p<0.05.
Results
Blood and Lymphocyte Subsets Count in COVID-19 Patients
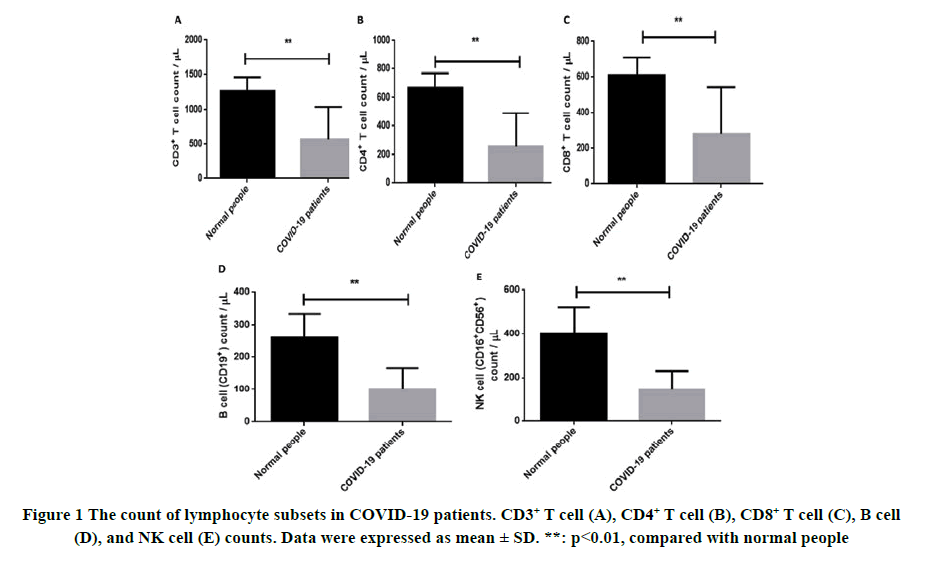
Lymphocyte count and all lymphocyte subsets significantly reduced in the blood of COVID-19 patients when compared with normal people (p<0.01). The difference in WBCs, neutrophils, and platelet count was non-remarkable in patients with COVID-19 when compared to healthy control (Figure 1 and Table 1).
Table 1 Blood count in normal individuals and COVID-19 patients (mean ± SD)
| Normal people | COVID-19 patients | p-value | |
|---|---|---|---|
| WBCs (× 109/L) | 5.32 ± 1.17 | 4.91 ± 2.22 | 0.717 |
| Lymphocytes (× 109/L) | 2.80 ± 1.21 | 1.07 ± 0.46 | 0.002 |
| Neutrophils (× 109/L) | 4.27 ± 0.89 | 3.70 ± 1.91 | 0.519 |
| Platelet count (× 109/L) | 200 ± 104.80 | 189 ± 62.76 | 0.81 |
The Count of Blood and Lymphocyte Subsets in Mild and Severe Cases with COVID-19
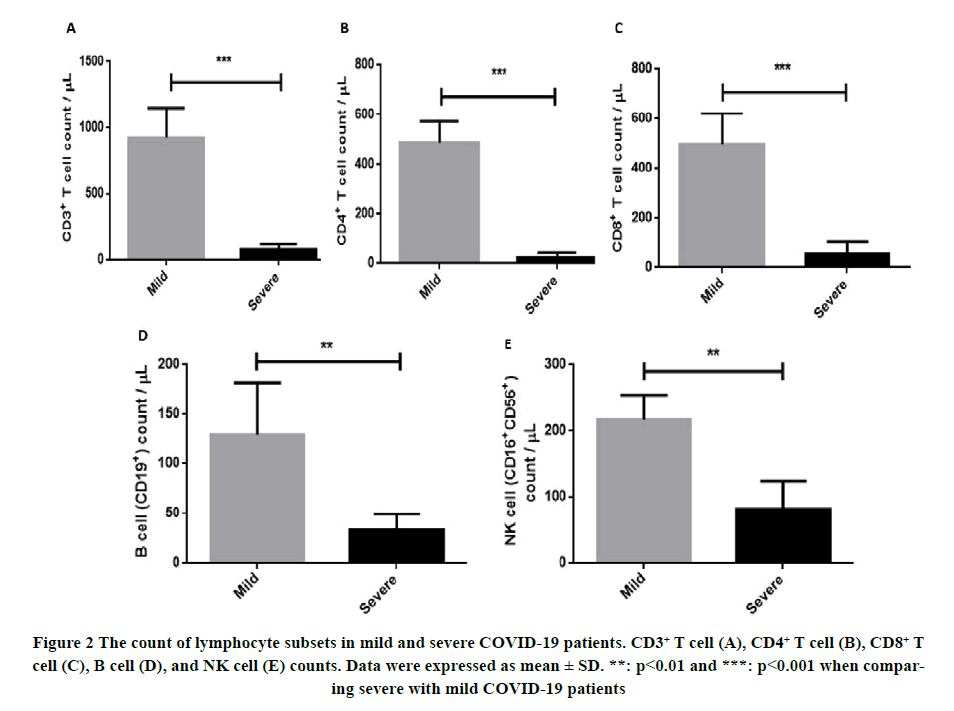
A significant difference in the total lymphocyte count (p<0.01) and in platelet count (p<0.05) was observed in severe cases when compared with mild COVID-19 patients. Regarding WBCs and neutrophils, there was a non-remarkable difference in their levels between the mild and severe groups of individuals. T and B lymphocytes substantially decreased in patients with severe symptoms when compared to patients with mild symptoms (p<0.001 and p<0.01 for CD3+ T and CD19+ B lymphocytes, respectively). CD4+ and CD8+ T lymphocytes remarkably diminished in severe COVID-19 patients as compared with mild COVID-19 people (p<0.001). Moreover, NK cells were reduced in in dividuals with severe COVID-19 with a conceivable difference (p<0.01) in their count as regard to mildly infected patients (Figure 2 and Table 2).
Table 2 Blood count in mild and severe COVID-19 patients (mean ± SD)
| Mild | Severe | p-value | |
|---|---|---|---|
| WBCs (× 109/L) | 5.12 ± 3.40 | 4.70 ± 0.81 | 0.845 |
| Lymphocytes (× 109/L) | 1.43 ± 0.32 | 0.71 ± 0.20 | 0.008 |
| Neutrophils (× 109/L) | 3.84 ± 2.93 | 3.55 ± 0.71 | 0.815 |
| Platelet count (× 109/L) | 235 ± 55.61 | 143 ± 22.07 | 0.022 |
Inflammatory Cytokine Levels in COVID-19 Patients
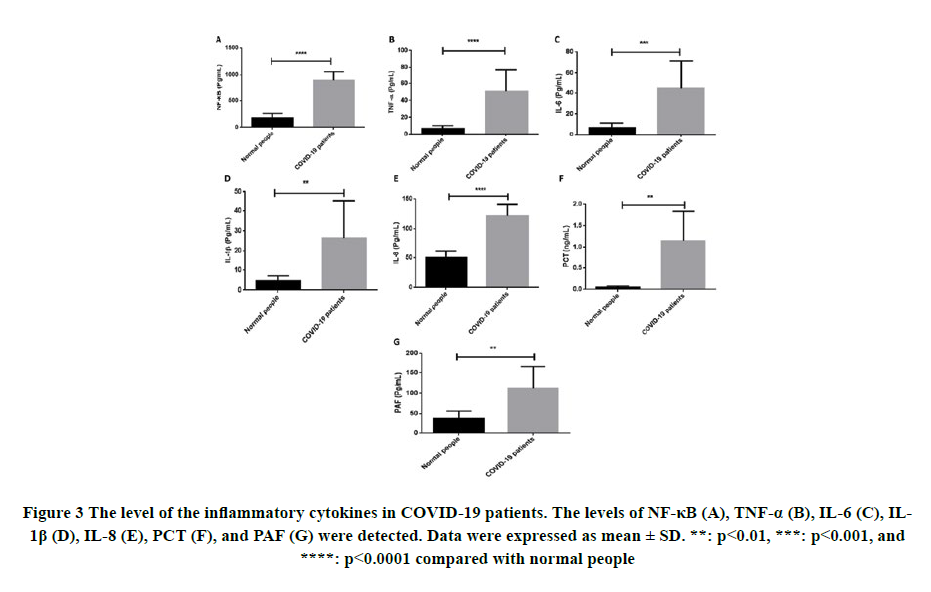
The inflammatory parameters; NF-κB, TNF-α, IL-6, IL-1β, IL-8, PCT, and PAF were measured in the plasma of COVID- 19 patients. All cytokines exhibited a highly significant elevation in cytokine levels as compared to normal healthy control (p<0.0001 for NF-κB, TNF-α, and IL-8, p<0.001 for IL-6, and P < 0.01 for IL-1β, PCT, and PAF) (Figure 3).
Inflammatory Cytokine Levels in Mild and Severely Infected Patients with Sars-Cov-2 Virus
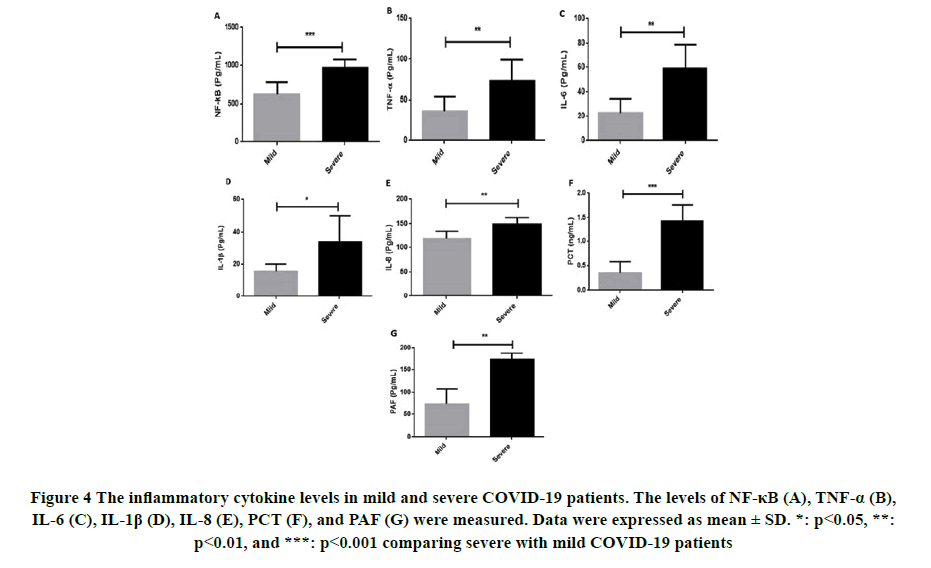
There was a significant increment in the cytokine levels in severely infected patients with SARS-CoV-2 when compared with mild cases (p<0.001 for NF-κB and PCT, p<0.05 for IL-1β, and p<0.01 for TNF-α, IL-8, IL-6, and PAF) (Figure 4).
Figure 4. The inflammatory cytokine levels in mild and severe COVID-19 patients. The levels of NF-κB (A), TNF-α (B), IL-6 (C), IL-1β (D), IL-8 (E), PCT (F), and PAF (G) were measured. Data were expressed as mean ± SD. *: p<0.05, **:
p<0.01, and ***: p<0.001 comparing severe with mild COVID-19 patients
Discussion
The pandemic COVID-19 is considered a vital threatening disease nowadays. It has been recorded that immune responses exhibit crucial effects in the regulation of viral infections of the respiratory system [10]. Subsequently, the current article aimed to investigate the variation in the subsets of lymphocytes and the pro-inflammatory mediators between mild and severe COVID-19 patients to get better ideas about disease propagation and consequences.
The function of the immune system was proven to be preserved by the lymphocytes and their subsets [11]. Their levels were disturbed in response to viral infection [12,13]. In the present study, lymphopenia was detected in an infected individual with SARS-CoV-2 with a significant decrease in severe cases that was attributed to direct viral contact or indirectly via recruitment of inflammatory mediators [11]. Our results were in line with Wang et al., Wong, et al. and Peiris, et al. who indicated decreased total lymphocyte levels in severely infected cases than mild patients [11,14,15]. Different lymphocyte subsets were reported to be related to cytotoxic and humoral immunity towards viral infection. The current outcomes showed that total lymphocyte count, the levels of all lymphocyte subtypes; CD4+ T cells, CD8+ T cells, B cells, and NK cells were lower in COVID-19 patients with a prominent reduction in severely infected patients with SARS-CoV-2 than mild cases. The previous findings were in agreement with Wong, et al. and Peiris, et al. who observed the same variations in SARS [14,15]. Reduced CD4+ T and especially CD8+ T lymphocytes elucidate disordered adaptive immune response in COVID-19 patients [3,16]. It has been shown that particularly CD8+ T lymphocyte is an important cellular immune component against viral respiratory infections and might be a possible indicator for the severity and clinical efficiency [11,17,18]. Moreover, the histological lung sections of COVID-19 dead people revealed infiltration of the adaptive inflammatory cells [19]. Subsequently, the reduced peripheral blood CD4+ T and CD8+ T cells count in our study was attributed to the recruitment of these lymphocyte subsets into the infected lung tissue of COVID-19 patients [3]. In addition to the adaptive immune cells, NK cells are innate effector lymphocytes that diminished in the peripheral blood of the present investigated COVID-19 patients. Various reports showed similar findings in moderately and severely infected patients with SARS-CoV-2 [11,20-23]. B lymphocyte count was significantly decreased in the current investigation and was associated with the disease severity which was supported by the previous investigations [11,24].
The disturbed immune response is associated with many symptoms and the main reason behind coronavirus mortality is the uncontrollable cytokine infiltration. Vigorous immune response was reported to be triggered by SARS-CoV-2 infection via the secretion of huge quantities of pro-inflammatory cytokines and chemokines, which were also prominent symptoms in SARS-CoV and MERS-CoV infections [25]. In the current study, higher levels of NF-κB, IL-6, TNF-α, IL-1β, and IL-8 were recorded in the plasma of COVID-19 patients with higher elevation in severe cases. The excessive secretion of the pro-inflammatory cytokines was correlated with lung injury and was reported to induce ARDS [26,27]. IL-6 was recorded to be correlated with the severity of the disease via complementing the function of CD8+ T cells [10,28]. It has been documented that TNF-α is the main cytokine that controls chemokine secretions and leukocyte adhesion molecule expressions on the vascular endothelium with subsequent induction of leukocytes infiltration towards the inflammation sites [29,30]. Moreover, the levels of TNF-α in serum were reported to be induced by a viral infection in murine models of SARS virus through the NF-κB pathway which may interpret the up-regulated protein expressions of pro-inflammatory cytokines upon SARS-CoV-2 infection [31,32]. Noteworthy, TNF-α via NF- κB activation stimulates cell apoptosis that may contribute to the decreased count of both CD4 and CD8 along with lymphopenia that was recorded in the current study [33,34]. Moreover, NF-κB is an important pro-inflammatory factor that regulates the expression and the secretion of different inflammatory cytokines such as TNFâ??α, IL-18, IL-6, IL-8, and IL-1β [35,36]. Various reports indicated the involvement of IL-1β in COVID-19 pathogenesis and its correlation along with IL-6 and IL-8 to ARDS propagation [2,27,37,38]. Our findings were consistent with the previous outcomes.
Patients who suffered from SARS-CoV-2 infection with severe COVID-19 were reported to be susceptible to blood coagulation and thrombosis formation [39,40]. Thrombi formation is triggered through platelets with their main inducer is PAF [40]. In the current research, both platelet count and the level of PAF increased upon infection with SARS-CoV-2 in severely infected patients than mild cases. Our outcomes were consistent with Hottz, et al. and Salamanna, et al. who recorded platelet stimulation and aggregation in COVID-19 patients [39,41]. Moreover, PAF levels were shown to increase in allergic rhinitis and chronic urticaria as well as it plays an eminent part in inflammation [42-45]. Through PAF secretion, platelets stimulate the activation of perivascular mast cells attributing to inflammation [40]. Since PAF are extensively found in mast cells especially those inside the lungs, they may contribute to COVID-19 [46,47].
PCT is among the factors that are known to be susceptible to bacterial infections and can be used as a predictor for inflammation propagation [48]. In the current experiment, the PCT level remarkably increased in patients with COVID- 19 with higher levels in severe cases. The clinical efficiency of this parameter was controversial and the highest value for PCT did not exceed the normal PCT level which was referred to as the small sample size [28,49,50].
Conclusion
In conclusion, total lymphocyte count and all lymphocyte subsets were reduced, while pro-inflammatory markers were induced upon infection with SARS-CoV-2. The variations in the inflammatory response in COVID-19 patients were correlated with the severity of the disease and might be targeted to interfere with the disease pathway.
Declerations
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-forprofit sectors
Conflict of Interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Heymann, David L., and Nahoko Shindo. "COVID-19: what is next for public health?." The Lancet, Vol. 395, No. 10224, 2020, pp. 542-45.
- Huang, Chaolin, et al. "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China." The Lancet, Vol. 395, No. 10223, 2020, pp. 497-506.
- Ni, Ming, et al. "Characteristics of inflammatory factors and lymphocyte subsets in patients with severe COVIDâ?19." Journal of Medical Virology, Vol. 92, No. 11, 2020, pp. 2600-06.
- Wei, Pei-Fang. "Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7)." Chinese Medical Journal, Vol. 133, No. 9, 2020, pp. 1087-95.
- Tay, Matthew Zirui, et al. "The trinity of COVID-19: immunity, inflammation and intervention." Nature Reviews Immunology, Vol. 20, No. 6, 2020, pp. 363-74.
- Cameron, Mark J., et al. "Human immunopathogenesis of Severe Acute Respiratory Syndrome (SARS)." Virus Research, Vol. 133, No. 1, 2008, pp. 13-19.
- Min, Chan-Ki, et al. "Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity." Scientific Reports, Vol. 6, No. 1, 2016, pp. 1-12.
- Chen, Nanshan, et al. "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study." The Lancet, Vol. 395, No. 10223, 2020, pp. 507-13.
- Guan, Wei-jie, et al. "Clinical characteristics of coronavirus disease 2019 in China." New England Journal of Medicine, Vol. 382, No. 18, 2020, pp. 1708-20.
- Nüssing, Simone, et al. "Innate and adaptive T cells in influenza disease." Frontiers of Medicine, Vol. 12, No. 1, 2018, pp. 34-47.
- Wang, Fan, et al. "Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia." The Journal of Infectious Diseases, Vol. 221, No. 11, 2020, pp. 1762-69.
- Chan, M. H. M., et al. "Serum LD1 isoenzyme and blood lymphocyte subsets as prognostic indicators for severe acute respiratory syndrome." Journal of Internal Medicine, Vol. 255, No. 4, 2004, pp. 512-18.
- Su, Rui, et al. "Imbalance between Th17 and regulatory T cells in patients with systemic lupus erythematosus combined EBV/CMV viraemia." Clinical and Experimental Rheumatology, Vol. 38, No. 5, 2019, 864-73.
- Wong, Raymond SM, et al. "Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis." BMJ, Vol. 326, No. 7403, 2003, pp. 1358-62.
- Peiris, J. S. M., et al. "Coronavirus as a possible cause of severe acute respiratory syndrome." The Lancet, Vol. 361, No. 9366, 2003, pp. 1319-25.
- Guo, Lingxi, et al. "Clinical features predicting mortality risk in patients with viral pneumonia: the MuLBSTA score." Frontiers in Microbiology, Vol. 10, 2019, pp. 2752.
- Wells, M. A., F. A. Ennis, and P. Albrecht. "Recovery from a viral respiratory infection. II. Passive transfer of immune spleen cells to mice with influenza pneumonia." The Journal of Immunology, Vol. 126, No. 3, 1981, pp. 1042-46.
- Cannon, M. J., et al. "Clearance of persistent respiratory syncytial virus infections in immunodeficient mice following transfer of primed T cells." Immunology, Vol. 62, No. 1, 1987, pp. 133-38.
- Xu, Zhe, et al. "Pathological findings of COVID-19 associated with acute respiratory distress syndrome." The Lancet Respiratory Medicine, Vol. 8, No. 4, 2020, pp. 420-22.
- Giamarellos-Bourboulis, Evangelos J., et al. "Complex immune dysregulation in COVID-19 patients with severe respiratory failure." Cell Host and Microbe, Vol. 27, No. 6, 2020, pp. 992-1000.
- Wilk, Aaron J., et al. "A single-cell atlas of the peripheral immune response in patients with severe COVID-19." Nature Medicine, Vol. 26, No. 7, 2020, pp. 1070-76.
- Jiang, Yujie, et al. "COVID-19 pneumonia: CD8+ T and NK cells are decreased in number but compensatory increased in cytotoxic potential." Clinical Immunology, Vol. 218, 2020, pp. 108516.
- Mazzoni, Alessio, et al. "Impaired immune cell cytotoxicity in severe COVID-19 is IL-6 dependent." The Journal of Clinical Investigation, Vol. 130, No. 9, 2020, pp. 4694-703.
- He, Ruyuan, et al. "The clinical course and its correlated immune status in COVID-19 pneumonia." Journal of Clinical Virology, Vol. 127, 2020, p. 104361.
- Yao, Zhixian, et al. "Immune environment modulation in pneumonia patients caused by coronavirus: SARS-CoV, MERS-CoV and SARS-CoV-2." Aging (Albany NY), Vol. 12, No. 9, 2020, p. 7639.
- Das, D., et al. "Viruses detected by systematic multiplex polymerase chain reaction in adults with suspected community-acquired pneumonia attending emergency departments in France." Clinical Microbiology and Infection, Vol. 21, No. 6, 2015, pp. 608-e1.
- Jiang, Yong, et al. "Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome." American Journal of Respiratory and Critical Care Medicine, Vol. 171, No. 8, 2005, pp. 850-57.
- Liu, Fang, et al. "Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19." Journal of Clinical Virology, Vol. 127, 2020, p. 104370.
- Bradley, J. R. "TNFâ?mediated inflammatory disease." The Journal of Pathology: A Journal of the Pathological Society of Great Britain and Ireland, Vol. 214, No. 2, 2008, pp. 149-60.
- Wang, Xinkang, et al. "Interleukin-1β induces expression of adhesion molecules in human vascular smooth muscle cells and enhances adhesion of leukocytes to smooth muscle cells." Atherosclerosis, Vol. 115, No. 1, 1995, pp. 89-98.
- Wang, Wei, et al. "Up-regulation of IL-6 and TNF-α induced by SARS-coronavirus spike protein in murine macrophages via NF-κB pathway." Virus Research, Vol. 128, No. 1-2, 2007, pp. 1-8.
- Pearce, Lucie, Sean M. Davidson, and Derek M. Yellon. "The cytokine storm of COVID-19: a spotlight on prevention and protection." Expert Opinion on Therapeutic Targets, Vol. 24, No. 8, 2020, pp. 723-30.
- Schett, Georg, Michael Sticherling, and Markus F. Neurath. "COVID-19: risk for cytokine targeting in chronic inflammatory diseases?." Nature Reviews Immunology, Vol. 20, No. 5, 2020, pp. 271-72.
- Jamilloux, Yvan, et al. "Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions." Autoimmunity Reviews, Vol. 19, No. 7, 2020, p. 102567.
- Wang, Wen-Ying, et al. "Role of pro-inflammatory cytokines released from microglia in Alzheimer’s disease." Annals of Translational Medicine, Vol. 3, No. 10, 2015, pp. 136.
- Tuller, T., et al. "Common and specific signatures of gene expression and protein-protein interactions in autoimmune diseases." Genes and Immunity, Vol. 14, No. 2, 2013, pp. 67-82.
- Toniato, E., R. Ross, and SK Kritas. "How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1." Journal of Biological Regulators and Homeostatic Agents, Vol. 34, No. 2, 2020, pp. 11-16.
- Kritas, S. K., et al. "Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy." Journal of Biological Regulators and Homeostatic Agents, Vol. 34, No. 1, 2020, pp. 9-14.
- Hottz, Eugenio D., et al. "Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19." Blood, The Journal of the American Society of Hematology, Vol. 136, No. 11, 2020, pp. 1330-41.
- Theoharides, Theoharis C., Smaragdi Antonopoulou, and Constantinos A. Demopoulos. "Coronavirus 2019, microthromboses, and platelet activating factor." Clinical Therapeutics, Vol. 42, No. 10, 2020, pp. 1850-52.
- Salamanna, Francesca, et al. "Platelet functions and activities as potential hematologic parameters related to Coronavirus Disease 2019 (Covid-19)." Platelets, Vol. 31, No. 5, 2020, pp. 627-32.
- Labrakis-Lazanas, K., et al. "PAF of biological fluids in disease: blood levels in allergic rhinitis." Haematologica, Vol. 73, No. 5, 1988, pp. 379-82.
- Ulambayar, Bastsetseg, et al. "Increased platelet activating factor levels in chronic spontaneous urticaria predicts refractoriness to antihistamine treatment: an observational study." Clinical and Translational Allergy, Vol. 9, No. 1, 2019, pp. 1-8.
- Camussi, Giovanni, and Jan R. Brentjens. "The role of platelet-activating factor in inflammation." Platelet-Activating Factor and Related Lipid Mediators, 1987, pp. 299-322.
- Antonopoulou, Smaragdi, et al. "PAF, a potent lipid mediator." Bioactive phospholipids. Role in Inflammation and Atherosclerosis, 2008, pp. 85-134.
- Theoharides, Theoharis C., Peter Valent, and Cem Akin. "Mast cells, mastocytosis, and related disorders." New England Journal of Medicine, Vol. 373, No. 2, 2015, pp. 163-72.
- Theoharides, Theoharis C. "COVIDâ?19, pulmonary mast cells, cytokine storms, and beneficial actions of luteolin." Biofactors, Vol. 46, No. 3, 2020, pp. 306-08.
- Covington, Elizabeth W., Megan Z. Roberts, and Jenny Dong. "Procalcitonin monitoring as a guide for antimicrobial therapy: a review of current literature." Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, Vol. 38, No. 5, 2018, pp. 569-81.
- Kim, Byung Geun, et al. "A comparison of the BISAP score and serum procalcitonin for predicting the severity of acute pancreatitis." The Korean Journal of Internal Medicine, Vol. 28, No. 3, 2013, pp. 322-29.
- Simsek, Osman, et al. "Inflammatory mediators in the diagnosis and treatment of acute pancreatitis: pentraxin-3, procalcitonin and myeloperoxidase." Archives of Medical Science: AMS, Vol. 14, No. 2, 2018, pp. 288-96.