Case Report - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 11
Decremental Retrograde Conduction After Catheter Ablation of aPosterior Accessory Pathway
Mihai Puiu, Gabriel Cismaru*, Gelu Simu, Gabriel Gusetu, Dana Pop, Dumitru Zdrenghea and Radu RosuGabriel Cismaru, 5th Department of Internal Medicine, Cardiology-Rehabilitation, Iuliu Hatieganu Univer, Romania, Email: gabi_cismaru@yahoo.com
Received: 17-Oct-2022, Manuscript No. ijmrhs-22-77443; Accepted Date: Nov 15, 2022 ; Editor assigned: 18-Oct-2022, Pre QC No. ijmrhs-22-77443(PQ); Reviewed: 22-Oct-2022, QC No. ijmrhs-22-77443(Q); Revised: 28-Oct-2022, Manuscript No. ijmrhs-22-77443(R); Published: 30-Nov-2022, DOI: 0
Abstract
Atrioventricular accessory pathways are characterized by rapid non-decremental conduction from the atria to the ventricles. Following catheter ablation, conduction through the accessory route disappears completely. However, few case reports described decremental antegrade accessory pathway conduction after radiofrequency ablation as a result of insufficient thermal effect at the ablation site. We present the case of a 70-year-old female patient with a left posterior accessory pathway that acquired decremental retrograde conduction after insufficient catheter ablation. We repeated radiofrequency applications until we attained full ablation accompanied by the loss of retrograde decremental conduction in its totality.
Keywords
Catheter ablation, Ventricular tachycardia, Premature ventricular contractions, Syncope, RVOT
Introduction
The majority of atrioventricular accessory pathways display Kent bundle physiology, which is characterized by rapid and non-decremental conduction from the atria to the ventricles. Following catheter ablation, conduction through the accessory route disappears completely [1, 2]. Few case reports described decremental antegrade accessory pathway conduction after radiofrequency ablation as a result of insufficient thermal effect at the ablation site [3]. We describe the case of a patient with a concealed accessory pathway that developed decremental retrograde conduction following insufficient catheter ablation which subsequently resolved after complete ablation.
Case Presentation
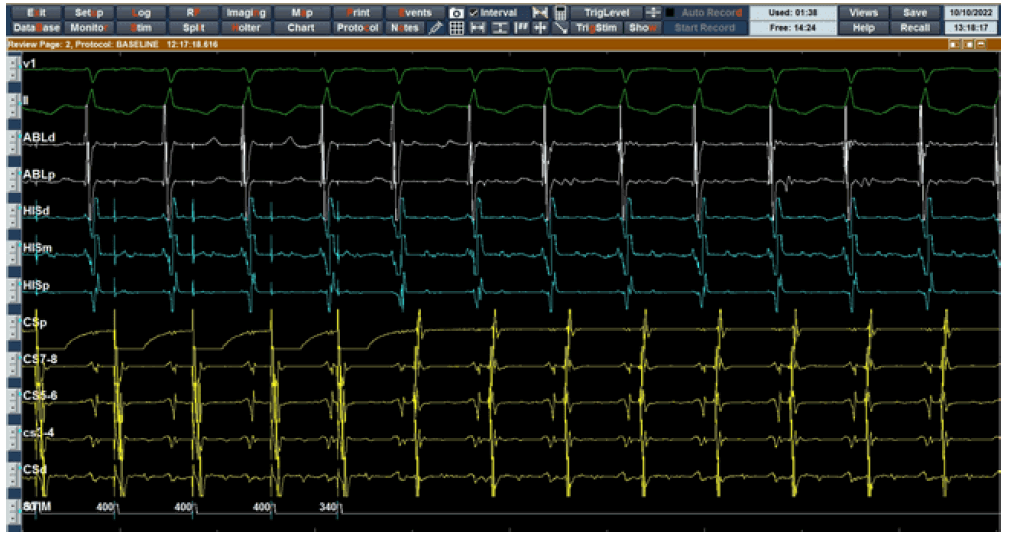
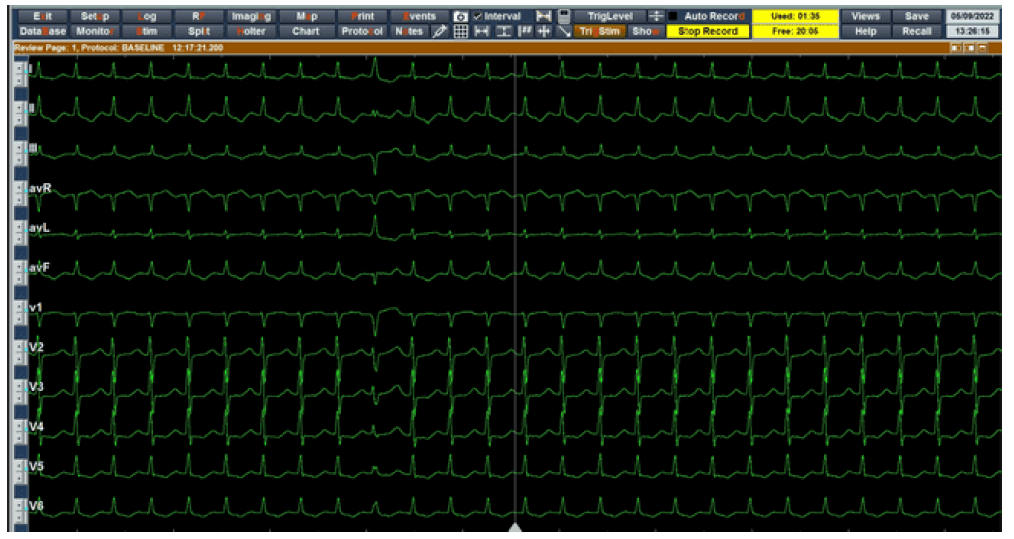
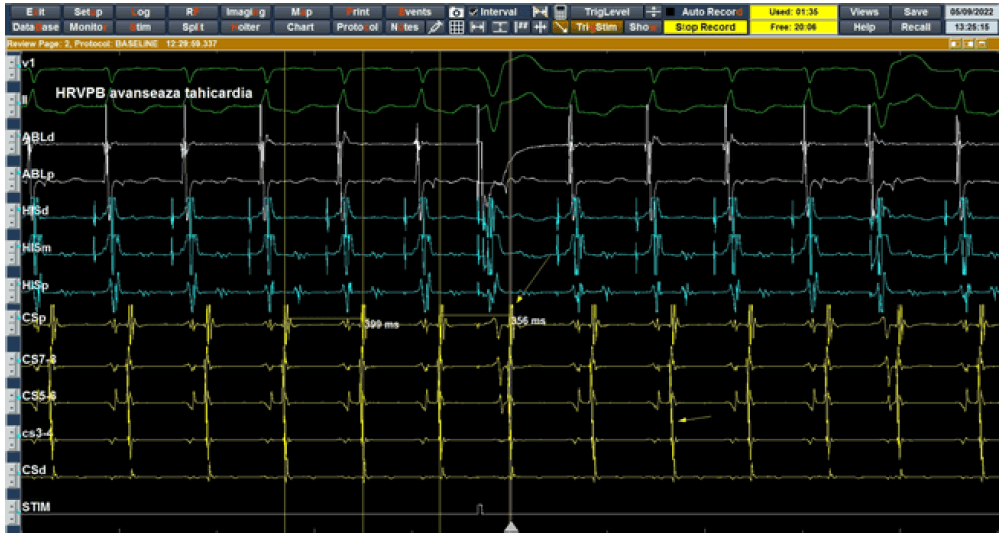
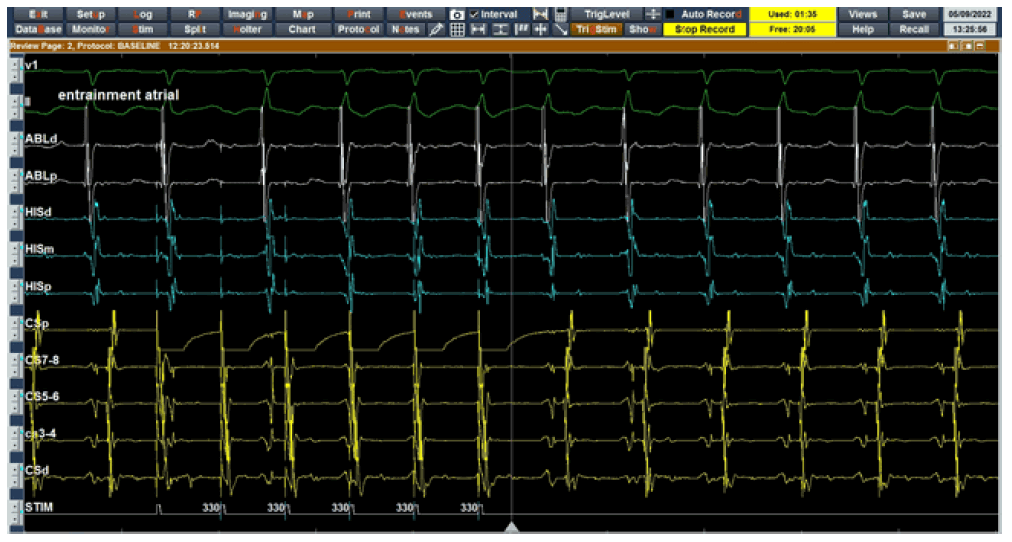
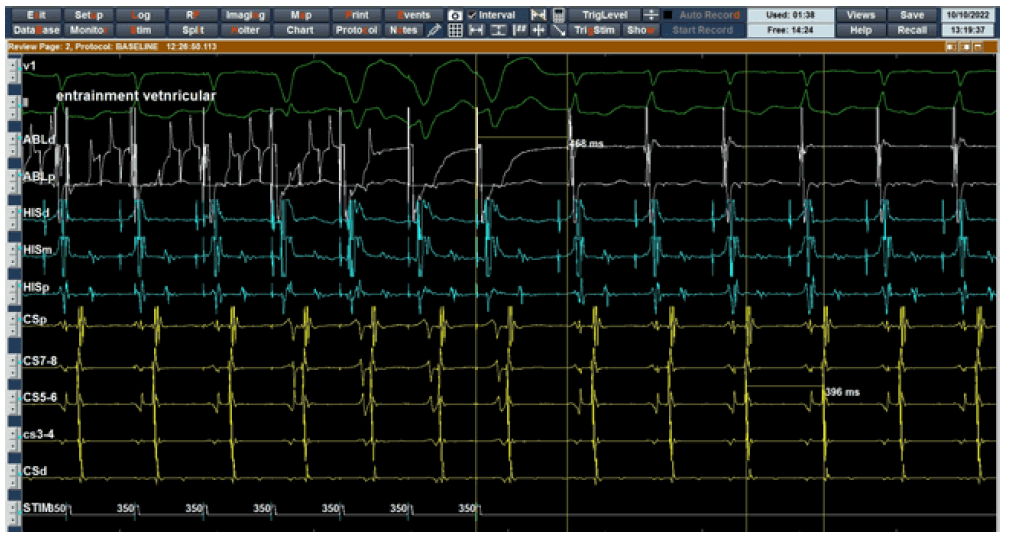
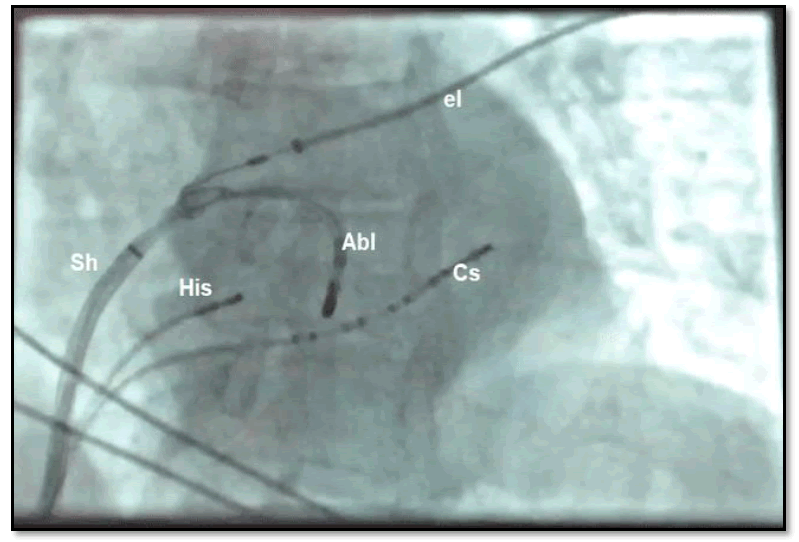
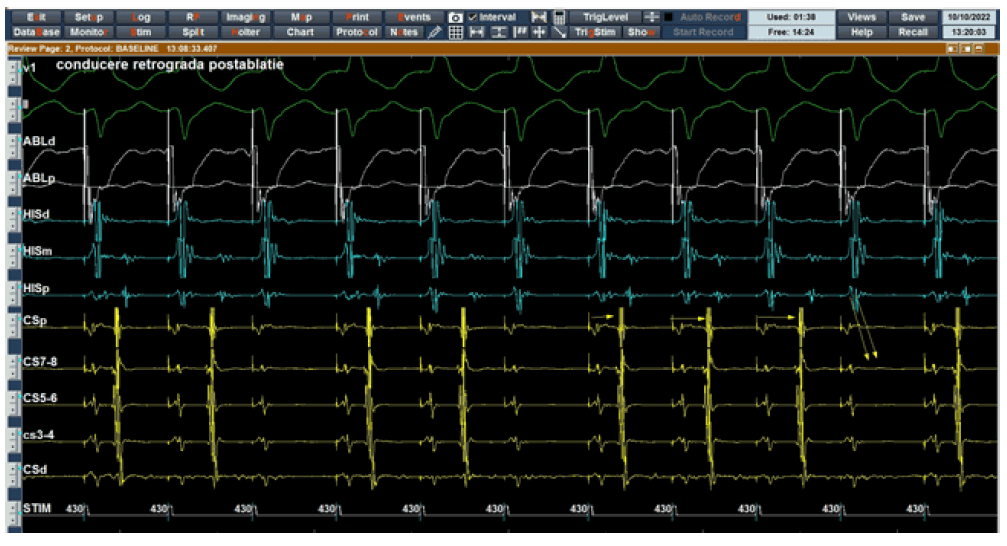
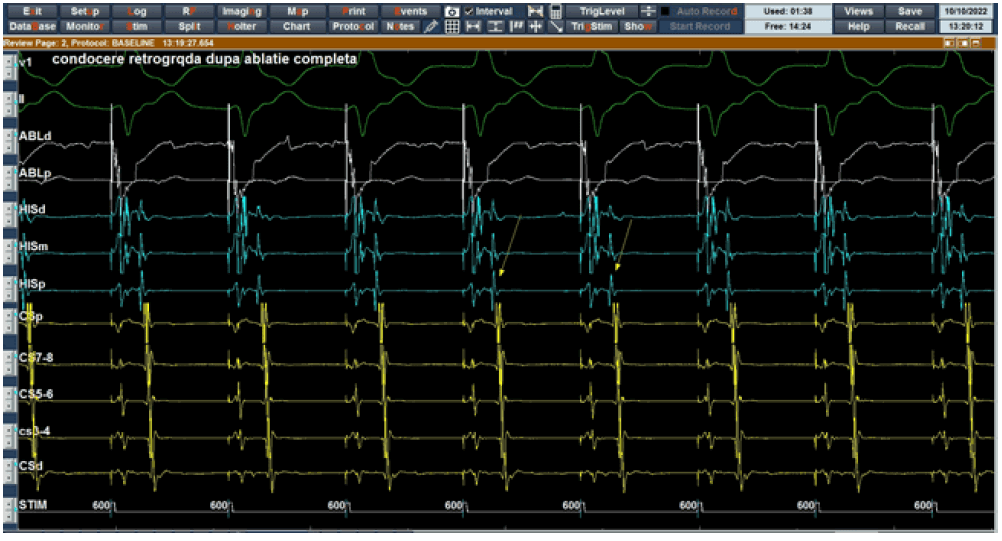
A 70-year-old female patient with frequent episodes of paroxysmal supraventricular tachycardia was hospitalized for an electrophysiological study and catheter ablation. Her last episode was 3 months before the hospitalization with a duration of 30 minutes. At presentation, her heart rate was 62 bpm with a BP of 130/70 mmHg, without any signs of heart failure. The ECG showed normal sinus rhythm with normal PR interval and absence of delta wave. An electrophysiological study was performed by using standard right and left heart catheterization techniques after the patient gave informed written consent. One quadripolar electrode catheter with was introduced percutaneously via the femoral vein and positioned at the level of the His bundle, a decapolar electrode catheter inside the coronary sinus, and the Ablation catheter at the level of tricuspid followed by the mitral ring. Tracings from the surface ECG leads (I, III, aVL, and V2) and bipolar intracardiac electrograms filtered at a bandpass of 50 Hz to 300 Hz were displayed on the Claris Saint Jude electrophysiological system screen which permitted exact measurements of the intracardiac intervals (Figure 1). The baseline rhythm was sinus, with a mean sinus cycle length of 640 ms. Incremental atrial pacing and the atrial extra stimulus were performed from the CS and high right lateral atrial wall, at the paced cycle lengths of 600 ms to 300 ms, without antegrade conduction through the accessory pathway. Ventricular stimulation showed retrograde fast non-decremental conduction through a posterior accessory pathway consistent with a concealed pathway with exclusive retrograde conduction. Programmed atrial stimulation induced supraventricular tachycardia which further demonstrated orthodromic reentrant tachycardia using a posterior accessory pathway as the retrograde limb as demonstrated by maneuvers: His-refractory ventricular premature beat, atrial entrainment, and ventricular entrainment. After the baseline electrophysiologic study, right and left endocardial mapping (using a transseptal approach) with an ablation catheter was performed to determine the earliest site of ventricular activation for radiofrequency ablation. The earliest site of ventricular activation was found to be located at the posterior mitral annulus, where the local ventricular electrogram preceded the delta wave by 20 ms with continuous ventricular and atrial electrograms during ventricular pacing (Figures 2-7). A 7-French quadripolar, Therapy Saint Jude deflectable tip catheter with a 4 mm distal electrode was used to deliver radiofrequency current from the distal electrode to a large skin electrode positioned on the posterior thorax of the patient. No recognizable accessory pathway potentials could be registered at the ablation site during ventricular stimulation. A single RF application of 30 W, 60 sec at the posterior mitral annulus abolished the 1:1 retrograde conduction. However, approximately 2 minutes after the ablation constant ventricular pacing from the right ventricular apex demonstrated retrograde decremental conduction through the accessory pathway (Figure 8). Therefore, new applications were performed at the same spot obtaining the absence of conduction through the accessory pathway and retrograde conduction through the AV node (Figure 9). After Atropine administration retrograde conduction through the accessory pathway did not recur. The patient was free of symptoms and the 12-lead ECG showed normal findings.
Figure 2. Programmed atrial stimulation produces an atrial echo through the accessory pathway followed by orthodromic reentrant tachycardia induction with a cycle length of 400 ms; Abl=Ablation catheter; His=catheter placed in hhe His bundle area; Cs=Coronary sinus catheter with 1,2=distal poles and 9-10=proximal poles
Figure 5. Atrial entrainment during supraventricular tachycardia shows the last entrained VA similar to the VA interval during tachycardia, which confirms the reentrant character of the tachycardia, excluding a focal type. Abl=Ablation catheter; His=catheter placed in hhe His bundle area; Cs=Coronary sinus catheter with 1,2=distal poles and 9-10=proximal poles
Figure 6. Ventricular entrainment during tachycardia demonstrates a post-pacing interval of 468 ms for a tachycardia cycle length of 396 ms. Therefore the PPI-TCL interval is <110 ms, which further confirms the tachycardia as a reentrant atrial-ventricular tachycardia using an accessory pathway; Abl=ablation catheter; His=catheter placed in hhe His bundle area; Cs=coronary sinus catheter with 1,2=distal poles and 9-10=proximal poles
Figure 7. Chest X-ray shows 3 catheters placed inside the heart chambers: His=quadripolar catheter placed in the His region; Cs=coronary sinus catheter, the most distal poles are Cs1-Cs2 placed in the lateral aspect of the mitral ring; Abl=ablation catheter which is placed at the posterior aspect of the mitral ring through a transseptal Sheath (Sh). In the X-ray picture, an external ECG Electrode (el) is also visible
Discussion
Normally, conduction from the atria to the ventricles occurs via the Atrioventricular (AV) node, which possesses decremental conduction (less and less propagation of atrial impulses to the ventricle due to a progressive decrease in membrane potential). Patients with an accessory pathway, which bypasses the AV node and connects the atria and ventricle directly, exhibit rapid non-decremental conduction [4].
Few cases reports described decremental accessory pathway conduction after radiofrequency ablation. Kawabata et al. described the case of a 60-year-old patient with decremental antegrade conduction of the accessory pathway after catheter ablation. They explained the findings by an insufficient thermal effect because of the power control mode with lower temperature ablation. In our case, permanent thermal damage to the accessory pathway developed after further applications at the level of the accessory pathway [3]. Five of the 136 participants in the Chen et al. investigation exhibited recurring pathways with decremental features after catheter ablation. Radiofrequency energy might damage the primary components of non-decremental accessory pathway fibers or alter the morphology and conduction properties of viable fibers distant from the lesion site, resulting in decremental conduction along the recurrent pathway [5].
Several studies demonstrate alterations in cellular electrophysiology properties produced by radiofrequency ablation [6, 7]. Decremental conduction may also be caused by nonspecific lesions to the per accessory pathway tissue, as well as the adjacent atrial or ventricular zones. Along the border zone of the RF lesion studies demonstrate a reduction in the action potential amplitude and action potential duration. These cellular electrophysiological abnormalities contribute to decremental conduction properties around the accessory pathway. Recent experimental electrophysiologic research revealed that hyperthermia causes progressive depolarization of membrane potential, a temperature-dependent increase in maximum upstroke velocity, temperature-dependent decreases in action potential duration and amplitude as well as loss of cellular excitability which can be reversible or irreversible leading to abnormal automaticity [8]. These electrophysiological effects may have altered the conduction properties of the concealed accessory pathway fibers in our patient, causing the accessory pathway to conduct decremental similar to an AV node.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Consent
Informed written consent was obtained from the mother of the patient for the publication of this case report and any accompanying medical images.
Data Availability
The data used and analyzed during the case report are available from the corresponding author upon request.
References
- Haissaguerre, Michel, et al. "Radiofrequency catheter ablation of accessory pathways: a contemporary review." Journal of cardiovascular electrophysiology, Vol. 5, No. 6, 1994, pp. 532-52.
Google Scholar Crossref - Murdock, Challon J., et al. "Characteristics of accessory pathways exhibiting decremental conduction." The American journal of cardiology, Vol. 67, No. 6, 1991, pp. 506-10.
Google Scholar Crossref - Kawabata, Mihoko, et al. "Marked anterograde decremental conduction over a rapidly conducting accessory pathway after radiofrequency ablation." Journal of electrocardiology, Vol. 33, No. 1, 2000, pp. 71-78.
Google Scholar Crossref - Deschamps, Hanna, and Elias B. Hanna. "Atrioventricular Accessory Pathways: Mechanisms, Electrocardiograms, and Associated Arrhythmias." Southern Medical Journal, Vol. 109, No. 10, 2016, pp. 670-76.
Google Scholar Crossref - Chen, Shil-Ann, et al. "Recurrent conduction in accessory pathway and possible new arrhythmias after radiofrequency catheter ablation." American Heart Journal, Vol. 125, No. 2, 1993, pp. 381-87.
Google Scholar Crossref - Bernstein, Scott A., et al. "Spatiotemporal electrophysiological changes in a murine ablation model." Europace, Vol. 13, No. 10, 2011, pp. 1494-1500.
Google Scholar Crossref - Moore, E. Neil, et al. "Electrophysiological studies on cardiac catheter ablation." Pacing and Clinical Electrophysiology, Vol. 12, No. 1, 1989, pp. 150-58.
Google Scholar Crossref - Nath, Sunil, et al. "Cellular electrophysiological effects of hyperthermia on isolated guinea pig papillary muscle. Implications for catheter ablation." Circulation, Vol. 88, No. 4, 1993, pp. 1826-31.
Google Scholar Crossref