Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
COVID-19 Vaccination Acceptability among Hospital Staff
Ayesha Shahid1*, Muhammad Ikram1, Haroon Javaid Majid2, Amna Javed1, Rukiya Tariq3 and Hamza Ahmad42Surgery and Surgical Oncology Department, Shaikh Zayed Hospital, Lahore, Pakistan
3Department of Public Health, University of the Punjab, Lahore, Pakistan
4Surgery and Allied Department, Shaikh Zayed Hospital, Lahore, Pakistan
Ayesha Shahid, Obstetrics and Gynecology Department, Shaikh Zayed Hospital, Lahore, Pakistan, Email: ayeshashahidred@gmail.com
Received: 13-May-2021 Accepted Date: Jun 22, 2021 ; Published: 30-Jun-2021
Abstract
Background: Concerns about rushed cases of Coronavirus in the country; vaccination is considered to be a significant measure to combat the Corona pandemic. But as soon the vaccine is available; complexity exists for its acceptance as well as willingness among individuals. Objective: To explore the relationships between socio-demographics and the willingness of respondents towards COVID-19 vaccination. Methods: The research was conducted on hospital staff. Both quantitative (convenient sampling) and qualitative research (in-depth interviews) method was used and data was analyzed through SPSS version 21. Results: Significant predictors for COVID-19 vaccine acceptance were age, gender, education, marital status, occupation, and monthly household of respondents whereas; predictors affecting willingness were exposure to patients and for protection and refusal i.e. availability, affordability, effectiveness, social media influence, trial phase, less research, distrust, safety issues and side effects with corona vaccine. Thus, the study highlights 52% and 48% of the hospital staff were willing and had refused for corona vaccination respectively. Conclusion: Vaccine hesitancy remains a significant defy and disseminating appropriate information through health education programs and campaigns on corona vaccine-related misconception and reinforcing benefits would improve vaccine acceptability and willingness among individual.
Keywords
COVID-19, Vaccine, Refusal, Health Care Workers, Acceptability, Misconceptions
Introduction
Globally up till now, 150,110,310 people with confirmed cases of Coronavirus and 3,158,792 deaths have occurred; but still many cases were unreported and undetected [1,2]. Like many other countries, Pakistan has also experienced the burden economically, in terms of morbidity and mortality; had 820,823 people been affected by COVID-19, and 17,811 deaths have been reported so far [3,4]. Health care providers including doctors, nurses, paramedical staff, and community health workers remain at high risk due to exposure and contact with the patients and had become an unexpected target in the fight against COVID-19; and to manage the COVID-19 pandemic; vaccination is considered as a key protective behavior against Coronavirus [5]. Soon the vaccine is available; its acceptability was found to be critical among individuals. So its a need of an hour to find out people’s acceptability for vaccines or to determine factors that can affect their acceptability because such data would be useful to develop strategies to improve acceptability following vaccine availability [6]. Vaccine hesitancy remains a substantial challenge for Pakistan as well [7]. According to a survey; 40% of Pakistanis are reluctant to get vaccinated against COVID-19 [8]. This study aims to assess a willingness to get the COVID-19 vaccine among health care providers and other hospital staff, as they are more exposed and vulnerable to contracting this deadly virus.
Methodology
It is mixed-method research involving both quantitative and qualitative studies with fifteen days duration i.e. 01-01- 2021 to 15-01-2021. Doctors, Nurses, paramedical staff, janitors currently working in Shaikh Zayed Hospital, Lahore, Pakistan were selected. Whereas, staff diagnosed with COVID-19 currently or previously by RT-PCR or Antibody testing were excluded from the study. In a quantitative study, convenient sampling was done. A structured questionnaire was designed which was previously pre-tested through pilot testing; data was collected and analyzed through SPSS version 21. Whereas, in qualitative study in-depth interviews were conducted from the same respondents who were already included in the study and filled the questionnaire. As a result, themes emerged through probing, and data was collected till the saturation point was reached in the study. Ethical approval was taken from the Gynecology and Obstetrics Department, Hospital Ethical Committee of Shaikh Zayed Hospital, Lahore, Pakistan.
Results
This study investigated the willingness of hospital staff to get COVID-19 vaccination with socio-demographic factors (age, gender, education, marital status, occupation and monthly income, COVID-19 Status) and determinants affecting their willingness and refusal towards COVID-19 vaccination. The study identified 52% of health care providers were in favor to get the COVID-19 vaccine; whereas; 48% of them had refused vaccination.
Socio-demographic Characteristics of Respondents and its Association with COVID-19 Vaccination Willingness
Respondents’ socio-demographic characteristics towards willingness of COVID-19 vaccine was shown in Table 1; was analyzed through descriptive statistics i.e. frequency and percentages as well as p-values were also analyzed in Table 1.
Table 1 Respondents socio-demographic characteristics and its association towards COVID-19 vaccine willingness (N=23)
| Socio-demographic characteristics | Willingness to get COVID-19 Vaccination | Total | p-value | |
|---|---|---|---|---|
| Yes (n=12) | No (n=11) | |||
| Age of respondents (years) | ||||
| 20-30 | 8 (67%) | 3 (27.3%) | 11 (48%) | p<0.036* |
| 31-40 | 2 (17%) | 3 (27.3%) | 5 (22%) | |
| 41-50 | 1 (8%) | 2 (18.1%) | 3 (13%) | |
| 51-60 | 1 (8%) | 3 (27.3%) | 4 (17%) | |
| Gender | ||||
| Male | 8 (67%) | 4 (36%) | 12 (52%) | p<0.001*** |
| Female | 4 (33%) | 7 (64%) | 11 (48%) | |
| Education | ||||
| No Formal | 0 (0%) | 2 (18.2%) | 02 (9%) | p<0.0003*** |
| Primary and Secondary | 1 (8%) | 3 (27.3%) | 04 (17%) | |
| Higher Secondary and above | 11 (92%) | 6 (54.5%) | 17 (74%) | |
| Marital Status | ||||
| Married | 7 (58%) | 3 (27%) | 10 (43%) | p<0.006** |
| Single | 5 (42%) | 8 (73%) | 13 (57%) | |
| Occupation | ||||
| Medics | 10 (83%) | 4 (36%) | 14 (61%) | p<0.012** |
| Non Medics | 2 (17%) | 7 (64%) | 9 (39%) | |
| Monthly Household | ||||
| Less than 25,000 | 1 (8%) | 0 (0%) | 01 (4.3%) | p<0.044* |
| 25,000-50,000 | 3 (25%) | 7 (64%) | 10 (43.5%) | |
| More than 50,000 | 8 (67%) | 4 (36%) | 12 (52.2%) | |
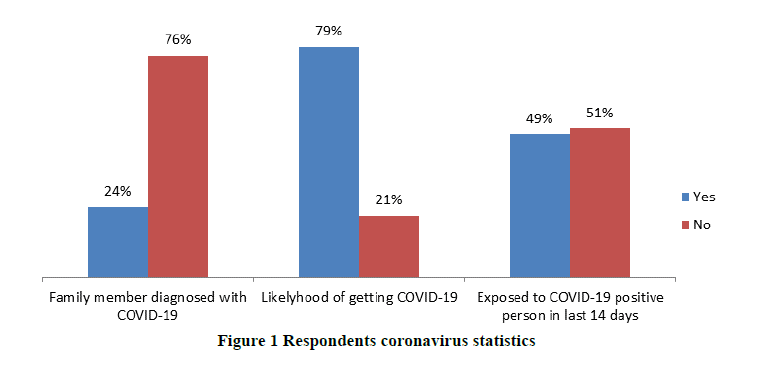
Respondents Corona Virus Statistics
Respondents’ detail on Coronavirus statistics were described in Figure 1. Respondent’s family members who were and were not diagnosed with COVID-19 virus were 24% and 76% respectively. The likelihood of getting Coronavirus was 79% and not having a chance of getting a virus was 21%. Respondents exposed to and not exposed to COVID-19 virus-positive person in the last 14 days were 49% and 51% respectively.
The willingness of Respondents to get COVID-19 Vaccination
We interviewed all participants in detail and asked about their views regarding COVID 19 vaccine and its acceptability till the saturation point reached. The results are divided into different themes and sub-themes.
Theme 1: Willingness: 12/23 participants were willing for the vaccination. They have different perspectives which made them willing to get vaccinated. These are divided into the following sub-themes.
Exposure to patients: Out of 12, 7 participants said that they are exposed to this deadly virus daily due to working in a hospital so they need this vaccine. One participant said:
‘I am exposed to many patients during my duty hours including both diagnosed and undiagnosed, so I think I should go for it.’
These participants included both doctors and nurses. But unfortunately, due to lack of awareness and compromised socioeconomic status of staff other than medical wasn’t willing to get vaccinated.
For protection: Out of 12 participants, 4 participants said that the vaccine will give us protection from COVID-19. One of the participants quoted:
‘I am worried about the likelihood of getting this virus in near future. Hence, I need some sort of protection for me as well as for my family. This vaccine not only protects me but also my family who are at the same risk of getting COVID-19 as me.’
Volunteer: Only 1 participant belonging to the nursing department presented as a volunteer to get the vaccination done.
Theme 2: Refusal: 11 out of 23 people refused to get themselves vaccinated. Following subthemes are the probable causes of their refusal.
Affordability: 5 out 11 participants including both medics and non-medics said that they don't want vaccines because of affordability issues. One of the participants had no idea whether he would afford it or not while another had doubts about him being able to afford it.
When inquired about ‘What if the vaccine is free for hospital staff.’,
4 out of 11 unwilling candidates were happy to get themselves vaccinated if it would be provided free. 6 still did not want that and one was concerned about the distributor of vaccines.
Availability: Availability can be an issue.
When asked about availability issue, as many things become short supplied when they are in high demand mostly in developing countries, One wanted it to be ensured by the government to not have any issue, while one said, ‘During the first phase of distribution, it would be an issue.’
One of the janitors has concerns that only doctors will get it while no one will ensure the providence of vaccine to workers.
Effectiveness: One of the participants has doubts about its effectiveness, so he remained unwilling.
No need for it: 2 said we just don't need it. Both of them belonged to non-medical staff who does not know much about vaccination.
Clueless: One was clueless about it.
Social media influence: One of the doctors was reluctant to get the vaccination done due to social media influence and said, ‘Have you watched that girl, getting a vaccine and dying because of that?’
Trial Phase: One said, ‘It’s still in the trial phase with no known potential benefits, so I’d decline the offer to get myself vaccinated’
Less research: One said there is not much research or literature available for that.
Distrust: 11/12 participants have trust issues with different pharmaceutical companies. One said that ‘Such companies are fraudulent’
While one said, ‘Local companies can't be trusted’
And one stated; ‘I can trust only certified companies.’
Theme 3: Safety
Concerns: 7 out of 12 willing participants considered it safe. One participant said,‘Pfizer is safe as it's approved by the USA. So, I’ll go for it. But I have concerns about other pharmaceutical companies.’
5 out of 11 unwilling participants have safety concerns about vaccines.
One of the participants said,‘I have safety concerns about vaccines because social media has shown many negative aspects about it.’
The rest of the participants has doubts about its safety.
Necessary for everyone: When asked about,
‘What If vaccine should be necessary for everyone….’
All willing candidates gave positive response while one has reservation that; ‘First, the safety of vaccines should be ensured before giving to all.’
Unwilling candidates had mixed responses; they were not going for a shot of vaccination but nearly half of them wanted everyone to get vaccinated, while others didn't want such atrocity of pinching everyone with a needle, 2 of them wanted only high-risk people to get vaccinated. One said; ‘I think only high-risk patients and healthcare workers should be getting this vaccine.’
Further Testing: When inquired whether we should wait for further testing or start vaccinating people 11 willing participants said we should go for further testing first before applying nationwide. Among them one said, ‘We should start it in small groups only.’
1/12 wanted to get a vaccine right now while testing simultaneously.
10/11 unwilling said we need further testing, one stated; ‘It’s too early to start on a large scale’
1/11 wanted not to be further tested.
Theme 4: Side effects: 4/12 willing participants didn't think there would be any potential side effects, as one said; ‘the virus in vaccines is not alive so no worries’ while 5 were concerned about side effects as one said ‘There is not much literature available’ while 3 did not have any idea about their side effects.
7 out of 11 unwilling participants think there are many side effects. One said,‘This vaccine needs further research.’
2 said there might not be any side effects, one of which thinks; ‘It's not even effective so why would it have any side effects?’
2 have doubts about it.
Chance of getting COVID-19 after vaccine: Willing: 5/12 thinks there is a chance of getting COVID-19 after vaccination because of strain adaptability while one thinks; ‘After some time virus will be different and we need another vaccine’
4/12 think only one vaccine will be enough to eradicate COVID-19 while 2 said they don't know. One has doubts about it.
Unwilling: 8/11 thinks one can get COVID-19 after vaccination as it's not effective while 2 thinks they don't think that one can get COVID-19 after the vaccine but they have other concerns, while one stated that he doesn't know.
Discussion
In our research, fear is an influential driver against corona vaccination thus, poses more apprehensiveness than the virus itself. The decline in immune function, auto-immune diseases, allergies, facial paralysis, and death; thus unveiled low levels of COVID-19 vaccination acceptance among the old age group i.e. 51 to 60 years [9-11]. Similarly, convincing females to accept the COVID-19 vaccine was found to be more crucial for slowing the persuasiveness of the novel Coronavirus; were more concerned about vaccine potential side effects i.e. vaccine may be experimental, was not safe for pregnant women, people with allergies and will compromise their ability to care for children [12-16].
The level of education thus signified appropriate knowledge and awareness among respondents towards the COVID-19 Pandemic and its prevention. Respondents with lower levels of education were engaged fewer towards COVID-19 protective behaviors, low trust and confidence in vaccine and healthcare system, less interaction with healthcare professionals, and were more concerned with vaccine cost; thus requires effective educational campaigns in raising public awareness and willingness towards COVID-19 vaccination [13,16-19]. Marital status had also been identified as a major determinant for misconceptions towards COVID-19 vaccination; thus revealed more willingness among married respondents than single respondents; was found congruent with Al-Mohaithef research; that vaccination will considerably block transmission, reduces fatality, and saves lives of high-risk groups [20-22].
Additionally, occupation also forecasts differences in knowledge and attitudes of respondent’s towards vaccine acceptance; for this healthcare professionals must take an active part in disseminating appropriate information on vaccination among individuals [23,24]. Economic status is the substantial determinant for upholding one’s health; research stated that low-income individuals were less likely to get vaccinated; thus requires equity in prioritizing the vaccine distribution, build trust through vaccine campaigns that emphasize vaccine transparency and adherence to scientific standards that will encourage population towards vaccine acceptance [12-14].
As, with the upsurge of Coronavirus cases; the safe and effective vaccine is considered to be an effective approach among health care workers towards COVID-19 prevention and control because they being frontlines fighters risk their lives against virus whereas, lack of confidence in the vaccine may delay or refusal to get vaccination among respondents [25-28]. To add further, research also revealed that vaccine safety acts as a considerable barrier especially because of newly launched; but if appropriate information was disseminated it will ensure more vaccine acceptance and its coverage among respondents [26,29].
Vaccine convenience such as access, distribution, coverage, and equity are the pre-requisites in addressing vaccine hesitancy [30]. The research revealed that respondents were willing to get a vaccination if the vaccine was available at affordable prices or free of cost; was found significant with Chen and his co-author's findings who suggested that most of the respondents were not willing to pay for the corona vaccine because of its market price [26]. Whereas, in another research, respondents had more willingness for the Corona vaccine if it was provided free of cost by the government [28]. But unfortunately, people in Pakistan had the misconception that vaccines that were launching as volunteers or free of cost were for clinical practice which turns down people's approval to get the vaccination.
Fear of side effects was also the reason for respondent’s hesitancy towards vaccination acceptance; concerns about vaccine safety from trustworthy sources and doctor’s recommendations and successful herd immunity in the population [30,31]. Nevertheless, the vaccine launched in Pakistan against the COVID-19 virus catches thriving attention but mainly among those individuals who had daily exposure with people while others with less awareness had more refusals because the vaccine does not build trust and guarantee to not have corona in future.
Conclusion
Vaccine acceptance plays a pivotal role in combating the Coronavirus pandemic. But as soon as the vaccine was available, its acceptance became a challenge among the community, and vaccine hesitancy became a major confounder on its acceptance because of the spread of misconception towards vaccine convenience, effectiveness, safety, and side effects. Therefore, the vaccine is needed for an hour and we must develop awareness through health education programs and campaigns to get ourselves self-vaccinated not only to protect us but also our family and community.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgments
We authors thank Dr. Humza Anwar and Mr. Obaid Ullah Ahmad for their massive efforts in data acquisition and digital assistance respectively, making our case proficient.
References
- WHO Coronavirus (COVID-19) Dashhboard. https://covid19.who.int/
- Rippinger, Claire, et al. "Evaluation of undetected cases during the COVID-19 epidemic in Austria." BMC Infectious Diseases, Vol. 21, No. 1, 2021, pp. 1-11.
- Atif, Muhammad, and Iram Malik. "Why is Pakistan vulnerable to COVID‐19 associated morbidity and mortality? A scoping review." The International Journal of Health Planning and Management, Vol. 35, No. 5, 2020, pp. 1041-54.
- COVID-19 Health advisory platform by Ministry of National Health Services Regulations and Coordination. http://covid.gov.pk/stats/pakistan
- Iyengar, Karthikeyan P., Vijay Kumar Jain, and Raju Vaishya. "Current situation with doctors and healthcare workers during COVID-19 pandemic in India." Postgraduate Medical Journal, 2020.
- Reiter, Paul L., Michael L. Pennell, and Mira L. Katz. "Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated?" Vaccine, Vol. 38, No. 42, 2020, pp. 6500-07.
- Khan, Yusra Habib, et al. "Threat of COVID-19 vaccine hesitancy in Pakistan: The need for measures to neutralize misleading narratives." The American Journal of Tropical Medicine and Hygiene, Vol. 103, No. 2, 2020, pp. 603-04.
- The Express Tribune. "40% Pakistanis wary of coronavirus vaccine." 2020. https://tribune.com.pk/story/2275994/40-pakistanis-wary-of-coronavirus-vaccine
- Chen, Yiyin, et al. "Aging in COVID-19: Vulnerability, immunity and intervention." Ageing Research Reviews, Vol. 65, 2020, p. 101205.
- World Economic Forum. "The COVID-19 disinformation divide: Understanding vaccine attitudes." https://www.weforum.org/agenda/2021/02/disinformation-covid19-vaccine-attitudes/
- Guidry, Jeanine PD, et al. "Willingness to get the COVID-19 vaccine with and without emergency use authorization." American Journal of Infection Control, Vol. 49, No. 2, 2021, pp. 137-42.
- Murphy, Jamie, et al. "Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom." Nature Communications, Vol. 12, No. 1, 2021, pp. 1-15.
- Paul, Elise, Andrew Steptoe, and Daisy Fancourt. "Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications." The Lancet Regional Health-Europe, Vol. 1, 2021, p. 100012.
- Lin, Cheryl, Pikuei Tu, and Leslie M. Beitsch. "Confidence and receptivity for COVID-19 vaccines: A rapid systematic review." Vaccines, Vol. 9, No. 1, 2021, p. 16.
- Neumann-Böhme, Sebastian, et al. "Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19." The European Journal of Health Economics, Vol. 21, 2020, pp. 977-82.
- Khubchandani, Jagdish, et al. "COVID-19 vaccination hesitancy in the United States: A rapid national assessment." Journal of Community Health, Vol. 46, No. 2, 2021, pp. 270-77.
- Lazarus, Jeffrey V., et al. "A global survey of potential acceptance of a COVID-19 vaccine." Nature Medicine, Vol. 27, No. 2, 2021, pp. 225-28.
- Center for Infectious Disease Research and Policy. "Survey: COVID vaccine willingness waned since April." 2020. https://www.cidrap.umn.edu/news-perspective/2020/12/survey-covid-vaccine-willingness-waned-april
- Mannan, Dr Kazi Abdul, and Khandaker Mursheda Farhana. "Knowledge, attitude and acceptance of a COVID-19 vaccine: A global cross-sectional study." International Research Journal of Business and Social Science, Vol. 6, No. 4, 2020.
- Al-Mohaithef, Mohammed, and Bijaya Kumar Padhi. "Determinants of COVID-19 vaccine acceptance in Saudi Arabia: A web-based national survey." Journal of Multidisciplinary Healthcare, Vol. 13, 2020, pp. 1657-63.
- Bubar, Kate M., et al. "Model-informed COVID-19 vaccine prioritization strategies by age and serostatus." Science, Vol. 371, No. 6532, 2021, pp. 916-21.
- European Centre for Disease Prevention and Control (ECDC). "COVID-19 vaccination and prioritisation strategies in the EU/EEA." 2020, p. 22.
- Wang, Kailu, et al. "Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: Repeated cross-sectional surveys." Vaccines, Vol. 9, No. 1, 2021, p. 62.
- Al-Qerem, Walid A., and Anan S. Jarab. "COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population." Frontiers in Public Health, Vol. 9, 2021, p. 34.
- Gan, Lin, et al. "Willingness to Receive SARS-CoV-2 vaccination and associated factors among Chinese adults: A cross sectional survey." International Journal of Environmental Research and Public Health, Vol. 18, No. 4, 2021, p. 1993.
- Chen, Musha, et al. "An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination." Human Vaccines & Immunotherapeutics, 2021, pp. 1-10.
- Rutten, Lila J. Finney, et al. "Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy." Mayo Clinic Proceedings, Vol. 96, No. 3, 2020, pp. 699-707.
- Qattan, Ameerah, et al. "Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia." Frontiers in Medicine, Vol. 8, 2021, p. 83.
- Wang, Jiahao, et al. "Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China." Vaccines, Vol. 8, No. 3, 2020, p. 482.
- Wang, Jiahao, et al. "The changing acceptance of COVID-19 vaccination in different epidemic phases in China: A longitudinal study." Vaccines, Vol. 9, No. 3, 2021, p. 191.
- Karlsson, Linda C., et al. "Fearing the disease or the vaccine: The case of COVID-19." Personality and Individual Differences, Vol. 172, 2021, p. 110590.