Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 10
Comparison of Once-Daily Triple Therapy versus Conventional Triple Therapy for Patient Compliance and the Eradication of Helicobacter pylori Infection
Naila Mohiuddin1*, Sumaiya Al Hajree1, Ruqiya Fatima1, Mohammed Mustaneer Akmal1, Syed Ibrahim Hassan2, Asif Rasheed1 and Aleem Ahmed Khan32Department of Gastroenterology, Princess Esra Hospital, Hyderabad, India
3Centre for Liver Research and Diagnostics, Owaisi Hospital and Research Centre, Hyderabad, India
Naila Mohiuddin, Department of Pharmacology, Deccan School of Pharmacy, Hyderabad, India, Email: nmohiuddin.pharmd@gmail.com
Received: 28-Sep-2021 Accepted Date: Oct 22, 2021 ; Published: 29-Oct-2021
Abstract
Aim: To compare the effectiveness of once-daily triple therapy with conventional triple therapy for the eradication of H. pylori. Materials and methods: A prospective comparative study in the gastroenterology unit of a tertiary care hospital was conducted for 6 months. 180 patients with active peptic disease tested positive for rapid urease test or 13C-UBT and concomitantly positive for anti-H. pylori antibodies IgG and IgM were given either once-daily (Tinidazole 1000 mg+Azithromycin 500 mg+Rabeprazole 40 mg) or twice-daily (Amoxicillin 500 mg+Clarithromycin 500 mg+Esomeprazole 40 mg) first-line therapy for ten days. Ten weeks after the completion of therapy rapid urease test and 13C-UBT were repeated. Adherence and adverse events were evaluated using pill count, structured questionnaires, and exit interviews. Results: The patient compliance was found to be better in the once-daily group (84.8%) when compared to the twice-daily group (68.8%). However, after treatment with the once-daily regimen, 74.6% of the subjects were tested negative for H. pylori and showed symptomatic relief. Whereas, with the conventional regimen, 68.7% of the subjects were tested negative for RUT and showed symptomatic relief (p=0.4063). Conclusion: We found that there was no significant difference in the eradication rates between both regimens. However, the once-daily regimen resulted in better medication compliance than the conventional regimen, suggesting that it can be considered as a safe and well-tolerated alternative to conventional triple therapies, especially for non-compliant patient groups. Further studies should be performed to confirm the results.
Keywords
Eradication, Helicobacter pylori, Medication compliance, Patient compliance, Triple therapy, India
Introduction
Helicobacter pylori also referred to as H. pylori is a bacterial pathogen that commonly colonizes in the gastric mucosa and is responsible for causing a plethora of disease conditions [1]. Its infection is among the leading gastrointestinal problems in developing countries. According to a recent report, the prevalence of H. pylori infection varied from 18.9% in Switzerland to 87.7% in Nigeria with approximately 4.4 billion individuals infected worldwide [2].
The presence of Helicobacter pylori is associated with gastritis, peptic ulcers, duodenal ulcers, and the development of gastric cancer [3]. The first-line therapy for the eradication of H. pylori usually consists of two antibiotics and a PPI administered for a period of 3 to 14 days [4]. Higher costs and longer time requirements make the in-vitro susceptibility testing and individualized treatment strategies based on MIC difficult to implement in practice. Therefore, various consensus groups worldwide support multidrug regimens as the standard way forward.
In many countries for the past few years, where Clarithromycin, Amoxicillin, and a PPI constituted as the standard therapy. But due to increasing Clarithromycin resistance, the success of this therapy has been reduced by 80% or even lower leading to considerable re-assessment of the present therapies [5].
Unfortunately, a significant proportion of patients fail to respond to therapy for a variety of reasons including bacterial resistance, poor compliance, the incidence of adverse events, and several other treatment-related factors.
The primary and secondary resistance to antibiotics including clarithromycin, metronidazole, and levofloxacin within the WHO regions has reached worrisome levels in the past decade, making their inclusion in the first-line regimen difficult [6].
Compliance is a multifactorial process directly related to eradication success and indirectly resulting in antibiotic resistance. Previous studies have suggested that 10% of patients prescribed H. pylori eradication therapy will fail to take even 60% of the medications [7]. Patients on triple therapy have to take about 6 tablets a day which adds up to 60 tablets throughout the treatment. Due to the complexity of treatment in addition to adverse effects related to medicines such as acidity patients are often compelled to become non-compliant. Simplified treatment and cost reduction aided by a once-daily regimen could potentially improve patient compliance. Additionally, as suggested by in-vitro studies, long dosing intervals associated with higher doses could prevent the development of antibiotic resistance [8].
This study was conducted to establish a simple regimen to strengthen adherence with effective and nontoxic agents which can be given with longer dosing intervals and are applicable initial therapy for H. pylori eradication.
Materials and Methods
Study Population
An initial 200 dyspeptic patients aged 18 years or older, with no history of recent antibiotic use, PPIs, bismuth, Non-Steroidal Anti-inflammatory Drugs (NSAIDs), anticoagulants, or steroids use for at least four weeks who were planned to undergo Esophagogastroduodenoscopy (EGD) were assessed in this prospective study.
Patients with impaired liver function, abnormal renal function, malignancies, and pregnant or lactating women were excluded. Patients who had pyloric stenosis or bleeding ulcer were also excluded. Fully informed consent was obtained from each patient entering the study.
Study Design
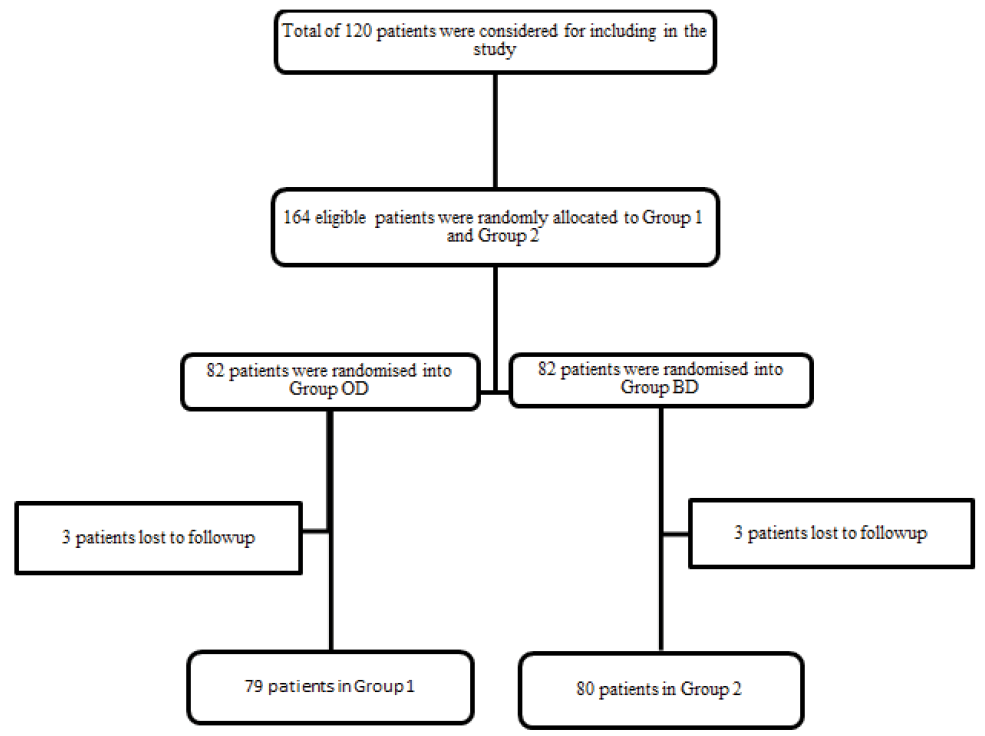
160 of the above patients who fulfilled the inclusion criteria and tested positive for RUT or 13C-UBT and anti- H. pylori antibodies IgG, IgM were relocated to one of the two treatment regimens: (i) Twice Daily (BD): Amoxicillin 500 mg, Clarithromycin 500 mg, Esomeprazole 40 mg for 10 days, or (ii) Once Daily (OD): Azithromycin 500 mg for 7 days, Tinidazole 1000 mg and Rabeprazole 40 mg for 10 days. After the end of 10 days treatment period, compliance was assessed using pill count, MMAS-8 score, and exit interview. The patients were called for follow-up after 10 weeks post-treatment during which the patients were free of medication. Each patient underwent EGD with Rapid Urease Test (RUT) or 13C Urea Breath Test (13C-UBT) after 10 weeks. Negative results 10 weeks after the treatment were defined as successful eradication treatment. Figure 1 shows the schematic flowchart of the study.
Efficacy Assessment
The primary clinical outcome measure was the eradication of H. pylori bacteria described by a negative RUT or 13C-UBT after 10 weeks of treatment completion. The compliance was assessed by counting pills at the end of the therapy and by using Morisky Medication Mdherence Scale (MMAS). Good compliance was defined as the consumption of more than 90% of the prescribed drugs as assessed by the interview held at the follow-up visit after the completion of treatment. Reasons for low compliance and adverse events of the drug therapy were also assessed and recorded at the interview.
Statistical Analysis
We determined the sample size needed to detect a difference of 8% in the compliance rate between the once-daily triple therapy group and the conventional triple therapy group, with a power of 85% and a significance level of 0.05 (α=0.05, two-sided). The final calculated sample size for each group was 73 with an effect size of 0.5, obtained from the pilot study.
Descriptive statistics were used to analyze the demographic profile, baseline, and clinical characteristics of the study population. Outcome variables were represented as percentages. Continuous variables are reported as numbers and percentages and compared using one-way ANOVA. Categorical variables were compared using Pearson’s Chi-square test or Fischer’s exact test.
Symptom assessment was done with an actual number of patients. Comparison of symptoms before and after within a group was done using McNemar’s test. Chi-square or Fischer exact method was used to compare the change in symptoms of groups I and II.
Adherence was assessed by Mann Whitney U-test. The results were depicted in the form of tables and graphs. Microsoft Word and Excel were used to generate graphs and tables. Statistics were performed using SPSS software version 20.0. A p-value less than 0.05 was considered statistically significant.
Results
Patients
The mean patient age was 38.53 ± 12.6 years. The demographic characteristics (Table 1) of the populations were similar between the two groups. However, hypothyroidism was more common in group OD. A literature review was done to obtain information regarding the association of hypothyroidism with H. pylori infection. The reports linking thyroid levels with the presence of H. pylori are controversial with none of those describing an influence of hypothyroidism on the eradication rate.
| Variables | Group I (n=79) | Group II (n=80) | p-value* | |
|---|---|---|---|---|
| Age (years), (mean, SD) | 38.52 ± 12.49 | 38.78 ± 13.0 | 0.889a | |
| Sex | Male, n (%) | 38 (48.1) | 36 (45) | 0.695 |
| Female, n (%) | 41 (51.9) | 44 (55) | ||
| Smoking, n (%) | 7 (8.86) | 7 (8.75) | 0.980 | |
| Alcohol consumption, n (%) | 2 (2.5) | 3 (3.75) | 1.000 | |
| Risk Factors | Ingestion of coffee or tea, n (%) | 49 (62.0) | 41 (51.25) | 0.170 |
| Mixed diet, n (%) | 75 (94.9) | 77 (96.2) | 0.719 | |
| NSAID use, n (%) | 2 (2.5) | 3 (3.75) | 0.681 | |
| Co-morbidities | Hypertension, n (%) | 20 (25.3) | 12 (15.2) | 0.105 |
| Diabetes Mellitus, n (%) | 11 (13.9) | 8 (10.1) | 0.446 | |
| Hypothyroidism, n (%) | 11 (13.9) | 2 (2.5) | 0.009 | |
| Endoscopic findings | Gastritis, n (%) | 65 (82.3) | 63 (78.6) | 0.779 |
| Reflux esophagitis, n (%) | 6 (7.6) | 6 (7.5) | ||
| Ulcer (duodenal or gastric), n (%) | 8 (10.1) | 11 (13.75) | ||
| *Chi-square test or Fischer test; a: One-way ANOVA | ||||
Of the 82 patients in the once-daily regimen group, 3 were lost to follow-up. Similarly, of the 82 patients of the twicedaily (conventional) regimen group, 2 were lost to follow-up (represented in the flow-chart). No patient discontinued the therapy due to adverse events. The endoscopy findings at the baseline are shown in Table 1. 82% of patients in group OD and 79% patients in group BD revealed gastritis. 10% of patients in the OD group and 14% of those in the BD group had either duodenal or gastric ulcers. Normal endoscopy was revealed in 8% of group OD patients and 8% of group BD patients (Table 2).
| Symptoms at baseline | Group I (n) | Group II (n) | p-value* |
|---|---|---|---|
| Heartburn | 48 | 33 | 0.014 |
| Belching | 46 | 33 | 0.032 |
| Bloating | 49 | 45 | 0.459 |
| Fatty food intolerance | 10 | 16 | 0.221 |
| Nausea | 19 | 12 | 0.139 |
| Abdominal cramps | 42 | 41 | 0.809 |
| Lethargy | 39 | 53 | 0.031 |
| SOB | 35 | 24 | 0.062 |
| *Chi-square test or Fischer test; SOB: Shortness of Breath; n: Number of patients | |||
H. pylori Eradication Rates
The overall eradication rates of the two treatment arms in all subjects (ITT) and subjects with good compliance (PP) are summarized in Table 3. By ITT analysis, the eradication rates were 74.7% in the OD group and 68.8% in the BD group; among patients with good compliance, the eradication rates were 77.6% in the OD group and 76.4% in the BD group, respectively (p>0.05).
| Variables | Group I | Group II | p-value | ||
|---|---|---|---|---|---|
| Eradication rate | All subjects, n (%) | 59/79 (74.7) | 55/80 (68.8) | 0.406* | |
| A subset of subjects with good compliance, n (%) | 52/67 (77.6) | 42/55 (76.4) | 0.436* | ||
| Compliance | >80% of medications taken, n (%) | 67/79 (84.8) | 55/80 (68.8) | 0.024* | |
| MMA Scale | Mean score (SD) | 7.44 (1.52) | 6.93 (1.14) | 0.009a | |
| High adherence, n (%) Score 8 | 56/79 (70.9) | 42/80 (52.5) | |||
| Moderate adherence, n (%) Score 6-7 | 20/79 (21.5) | 30/80 (36.3) | |||
| Low adherence, n (%) Score 0-5 | 3/79 (7.6) | 8/80 (11.3) | |||
| *Chi-square test; a: Mann-Whitney U test; MMAS: Morisky Medication Adherence Scale; n: Number of patients | |||||
Compliance and Adverse Events
The most common adverse events among the patients of both groups were dysgeusia, observed in 45.9% patients in group OD and 54% patients in group BD (Table 4). The overall adverse events occurrence rates were similar in the once-daily group and twice-daily group. All the adverse events were of mild intensity and no patient withdrew from the study due to adverse events.
| Adverse Events | Group I | Group II | p-value* |
|---|---|---|---|
| Dizziness | 5 | 5 | 1.000 |
| Nausea/Vomiting | 3 | 6 | 0.495 |
| Headache | 7 | 2 | 0.098 |
| Rashes | 4 | 4 | 1.000 |
| Dysguesia | 30 | 30 | 0.951 |
| Dry mouth | 0 | 4 | 0.120 |
| *Chi-square test or Fischer’s exact test | |||
Compliance was assessed directly by counting pills at the end of the therapy. Patients who reportedly consumed 80% or more medications were considered to be having “good compliance”. 85% of patients in group OD and 69% of patients in group BD showed good compliance as determined by personal interviews at the end of the therapy. Additionally, as assessed by using the MMAS-8 questionnaire the patients in the OD group showed significantly greater compliance than BD (Table 4).
Symptom Assessment
Significant improvement in all the symptoms in both groups was found at the end of the treatment. Between the groups, reduction in heartburn and shortness of breath was more pronounced in group OD (83.3% and 80%, respectively) than group BD (63.6% and 75%, respectively) (Table 5).
| Symptoms | Group I % Change | p-value* | Group II % Change | p-value* | p-valuea Between groups |
|---|---|---|---|---|---|
| Heartburn | -83.33% | <0.001 | -63.64% | <0.001 | 0.002 |
| Belching | -76.09% | <0.001 | -72.73% | <0.001 | 0.067 |
| Bloating | -75.51% | <0.001 | -73.33% | <0.001 | 0.063 |
| Fatty food intolerance | -90.00% | <0.004 | -75.00% | <0.004 | 0.677 |
| Nausea | -78.95% | 0.001 | -50.00% | 0.210 | 0.336 |
| Abdominal Cramps | -83.33% | <0.001 | -75.61% | <0.001 | 0.381 |
| Lethargy | -79.49% | <0.001 | -84.91% | <0.001 | 0.196 |
| SOB | -80.00% | <0.001 | -75.00% | <0.001 | 0.046 |
| * McNemar's test for comparison of before and after symptoms (Symptom assessment was done with actual number of patients); a: Chi-square or Fischer exact test between groups; SOB: Shortness of Breath | |||||
Discussion
About half of the world’s population is infected with H. pylori with varying amounts of prevalence across regions [2]. According to the latest reports of consensus published by the Indian Society of Gastroenterology (ISG) in 2021, there is an increased disease burden and high reoccurrence rate of H. pylori across India over the last decade [9]. Furthermore, a fair link between the reduction in gastric cancer-related mortality with an overall improvement in proper eradication rates in East-Asian countries has been established [10].
The mechanisms by which H. pylori has adapted to stay in the stomach have made it immune to several H. pylori eradication medications. Hence, multidrug regimens consisting of two antibiotics and a PPI are chosen for variable time durations, strengths, and doses to treat it [11].
Eradication rate depends on several patient factors with its relation being inversely associated with the presence of gastric ulcers and lack of medication compliance [12]. Poor adherence always leads to subtherapeutic levels or suboptimal doses resulting in poor clinical outcomes thereby resulting in a reduced eradication rate. In addition to patient and environmental factors, the most important factor which affects the cure rates is the antibiotic resistance of H. pylori strains, which is progressively increasing every year [13,14].
According to a recent study evaluating the antimicrobial resistance to H. pylori, it was found that in India 81.4% of the total H. pylori strains were resistant to metronidazole, 54.9% were resistant to levofloxacin, 20.4% were resistant to Clarithromycin [15]. Moreover, multidrug resistance was found in 59.3% of total isolated strains among which 86.6% were resistant to at least both metronidazole and levofloxacin indicating high primary resistance to metronidazole and levofloxacin and modest resistance to Clarithromycin reducing their usefulness as a first-line treatment [15].
In this study, a once-daily anti- H. pylori regimen was compared and evaluated against the conventional, twice-daily H. pylori regimen.
To find antibiotics for a once-daily regimen, characteristics of several antibiotics such as half-life and tissue concentration were taken into account. Previous studies conducted in other countries included levofloxacin in their once-daily regimen which we avoided considering the resistance rate of the antibiotic in India.
In our study, we employed Tinidazole, a drug from the nitroimidazole class. Nitroimidazoles reach a very high concentration in gastric lumen (up to 1000 mg/l) with their oral bioavailability estimated to be more than 90% compared with intravenous administration [16]. The use of nitroimidazoles for H. pylori eradication is limited by the increasing resistance of H. pylori. Tinidazole has a half-life of 12 hours-13 hours and has shown good results in previous studies. The activity of Tinidazole is independent of pH. Moreover, the drug has better tolerability and favourable pharmacokinetics in comparison to metronidazole.
Azithromycin, which is a new generation macrolide, readily accumulates in the human gastric mucosa which then redistributes to the mucus layer from the mucosal tissue and finally reaches the gastric tissue where its tissue concentration persists above its MIC90 over 5 days. This in addition to the high pharmacological affinity of Azithromycin makes it a useful alternative for H. pylori treatment [17].
In our study, the combination of Azithromycin and Tinidazole along with a PPI were employed for the once-daily regimen. There was an improvement in the eradication rate in both groups when a sub-analysis of patients with good compliance in both groups was performed. However, the difference in the eradication rate between the groups was not statistically significant (Table 3).
In terms of compliance, the rate was significantly better in the OD group compared to the BD group (Table 3). The number of pills that were required to be taken in the OD group was much lesser compared to the other group, possibly contributing to an improvement in patient medication adherence and thereby influencing treatment success.
Many factors influenced drug compliance among patients including the duration of treatment, number of drugs, and side effects of medications.
We acknowledge that this study has limitations. The eradication with either regimen did not achieve the desirable eradication rate of 90% for first-line therapy. Within the settings in which the study was performed, it was impossible to impose blinding. Self-reported adherence and adverse events evaluation interviews have drawbacks like social desirability bias and a tendency to overestimate adherence. Although measures such as the pill count method were used, it can sometimes misrepresent adherence, since it fails to measure whether the medication was taken on scheduled time.
Within our study, it was not possible to utilize a symptom assessment scale and therefore, actual patient numbers were used. For statistical analysis of symptom assessment, we needed to dichotomize patients into “symptom found” and “symptom not found” groups; however, this led to simplification and loss of information regarding the severity of symptoms.
Conclusion
The once-daily regimen did not yield a statistically significant eradication rate when compared with their twice-daily regimen counterpart. However, a once-daily regimen resulted in better medication compliance than the conventional regimen. The once-daily therapy can be considered safe and satisfactory, and they appear to be a well-tolerated alternative to the conventional triple therapy, especially for non-compliant patient groups. Further studies should be performed to confirm the results.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Source of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Approval
This study was approved by the Institutional Review Boards of the Deccan College of Medical Sciences and Allied Hospitals with the protocol number 2019/29/003 on November 27, 2019
References
- Robinson, Karen, Darren P. Letley, and Kazuyo Kaneko. "The human stomach in health and disease: Infection strategies by Helicobacter pylori." Molecular Pathogenesis and Signal Transduction by Helicobacter pylori, 2017, pp. 1-26.
- Hooi, James KY, et al. "Global prevalence of Helicobacter pylori infection: Systematic review and meta-analysis." Gastroenterology, Vol. 153, No. 2, 2017, pp. 420-29.
- Venerito, Marino, et al. "Helicobacter pylori and gastrointestinal malignancies." Helicobacter, Vol. 20, 2015, pp. 36-39.
- O’Connor, Anthony, et al. "Treatment of Helicobacter pylori infection 2010." Helicobacter, Vol. 15, 2010, pp. 46-52.
- Zou, Yunzhi, et al. "The effect of antibiotic resistance on Helicobacter pylori eradication efficacy: A systematic review and meta‐analysis." Helicobacter, Vol. 25, No. 4, 2020, p. e12714.
- Savoldi, Alessia, et al. "Prevalence of antibiotic resistance in Helicobacter pylori: A systematic review and meta-analysis in World Health Organization regions." Gastroenterology, Vol. 155, No. 5, 2018, pp. 1372-82.
- Lee, Marianne, et al. "A randomized controlled trial of an enhanced patient compliance program for Helicobacter pylori therapy." Archives of Internal Medicine, Vol. 159, No. 19, 1999, pp. 2312-16.
- Olofsson, Sara K., and Otto Cars. "Optimizing drug exposure to minimize selection of antibiotic resistance." Clinical Infectious Diseases, Vol. 45, No. Supplement 2, 2007, pp. S129-36.
- Singh, Shivaram Prasad, et al. "Management of Helicobacter pylori infection: The Bhubaneswar consensus report of the Indian Society of Gastroenterology." Indian Journal of Gastroenterology, 2021, pp. 1-25.
- Ford, Alexander Charles, Yuhong Yuan, and Paul Moayyedi. "Helicobacter pylori eradication therapy to prevent gastric cancer: Systematic review and meta-analysis." Gut, Vol. 69, No. 12, 2020, pp. 2113-21.
- Jenks, Peter J. "Causes of failure of eradication of Helicobacter pylori: Antibiotic resistance is the major cause, and susceptibility testing may help." BMJ, 2002, pp. 3-4.
- Cutler, Alan F., and Timothy T. Schubert. "Patient factors affecting Helicobacter pylori eradication with triple therapy." American Journal of Gastroenterology (Springer Nature), Vol. 88, No. 4, 1993, pp. 505-09.
- Uotani, Takahiro, Muhammad Miftahussurur, and Yoshio Yamaoka. "Effect of bacterial and host factors on Helicobacter pylori eradication therapy." Expert Opinion on Therapeutic Targets, Vol. 19, No. 12, 2015, pp. 1637-50.
- Rizvanov, Albert A., et al. "Helicobacter pylori and its antibiotic heteroresistance: A neglected issue in published guidelines." Frontiers in Microbiology, Vol. 10, 2019, p. 1796.
- Shetty, Vignesh, et al. "High primary resistance to metronidazole and levofloxacin, and a moderate resistance to clarithromycin in Helicobacter pylori isolated from Karnataka patients." Gut Pathogens, Vol. 11, No. 1, 2019, pp. 1-8.
- Manes, Gianpiero, and Antonio Balzano. "Tinidazole: From protozoa to Helicobacter pylori-the past, present and future of a nitroimidazole with peculiarities." Expert Review of Anti-Infective Therapy, Vol. 2, No. 5, 2004, pp. 695-705.
- Dong, Jie, Xiao-Feng Yu, and Jian Zou. "Azithromycin-containing versus standard triple therapy for Helicobacter pylori eradication: A meta-analysis." World Journal of Gastroenterology: WJG, Vol. 15, No. 48, 2009, pp. 6102-110.