Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
Clinico-Pathological Study of Abnormal Uterine Bleeding-A Two Year Study at Tertiary Care Center
Megha S. Kinake1, Shweta Watane1* and Shubha Deshpande22Department of Pathology, Dr. Shankarrao Chavan, Government Medical College, Nanded, Maharashtra, India
Shweta Watane, Department of Pathology, Grant Government Medical College, Mumbai, Maharashtra, India, Tel: 022 2373 5555, Email: sswetawatane@gmail.com
Received: 13-May-2021 Accepted Date: Jun 22, 2021 ; Published: 30-Jun-2021
Abstract
Background: Histopathological assessment of endometrial samples plays a crucial role in the diagnosis of Abnormal Uterine Bleeding (AUB). The present study was conducted to assess the histopathology of the endometrium with AUB. Methods: It is a prospective study conducted in the Department of Pathology, Dr. Shankararo Chavan, Government Medical College, Nanded, Maharashtra, India. All cases attending Gynaecology OPD with AUB were included in the study. The sample received was Dilatation and Curettage (D and C) samples, endometrial biopsy, polypectomy, and hysterectomy specimen. Specimens were routinely processed and stained with hematoxylin and eosin stains and microscopic morphological evaluation was done and data recorded and analyzed. Results: We studied 680 cases. Out of which 661 cases showed significant findings and 19 were reported unsatisfactory samples for evaluation. The commonest histomorphological pattern in these patients was proliferative endometrium 248 (36.47%), leiomyoma 100 (14.70%), adenomyosis 90 (13.23%), endometrial hyperplasia 72 (10.58%), secretory endometrium 47 (6.91%), atrophic endometrium 40 (6.91%), endometritis 11 (1.61%), endometrial polyp 27 (3.97%), adenomyosis with leiomyoma were seen in 23 cases (3.66%) and least number cases were of endometrial carcinoma forming 3 (0.44%) of the total cases taken in the study. Conclusions: The outcomes of the present study provide important information about the prevalence of Abnormal uterine bleeding is common in the peri-menopausal period in the fourth and fifth decades of life. The most common clinical presentation is menorrhagia. The commonest histopathological pattern is proliferative endometrium suggesting anovulation. Histopathological examination of endometrium inpatient of AUB shows a wide spectrum of changes ranging from normal endometrium to malignancy. Accurate analysis of endometrial sampling is important in the management of AUB.
Keywords
AUB, Endometrium, Leiomyoma, Menorrhagia
Introduction
Abnormal Uterine Bleeding (AUB) is defined as changes in the frequency of menstruation, duration of flow, or amount of blood loss [1].
AUB interferes significantly with the quality of life in otherwise healthy women with various distressing symptoms like menorrhagia, polymenorrhea, and metrorrhagia [2-4].
The cause of AUB varies according to age, endometrial response to hormones and their variations, and other structural lesions [5].
AUB can be due to functional disturbances referred to as dysfunctional uterine bleeding and organic pathologic conditions, such as chronic endometritis, endometrial polyps, endometrial hyperplasia, submucosal leiomyoma, or endometrial neoplasm [6].
Currently, the most commonly used technologies for outpatient evaluation of the endometrium are biopsy, hysteroscopy, and Trans Vaginal Ultrasound (TVS). Endometrial biopsy by Dilatation and Curettage or office endometrial biopsy is considered the gold standard in AUB [7].
Hysterectomy is one of the most common surgical procedures in gynecology worldwide. It is one of the major methods of surgical management of abnormal uterine bleeding [8].
Below the age of 20 years, the disturbance is most likely to be a functional one. Inactive reproductive life, an organic cause for bleeding is more likely, pregnancy-related conditions being the most common [9].
Histopathological diagnosis of endometrium samples varies according to the age with increased risk of endometrial hyperplasia and endometrial carcinoma is in peri-menopausal and post-menopausal women, so early evaluation of the peri-menopausal and postmenopausal women is essential to confirm the exact nature of the lesion and to rule out malignancy [10].
The key to successful clinical management is to recognize or identify the causative factors responsible. This study was done to evaluate the endometrial causes of AUB and to determine the specific pathology in different age groups.
Methods
The present study “Clinico-pathological study of abnormal uterine bleeding” was undertaken in the Department of Pathology, Dr. Shankararo Chavan, Government Medical College, Nanded, Maharashtra, India.
Study Design
Prospective study.
Duration of Study
January 2011-December 2012
Approval from the institutional ethical committee and Maharashtra University of Health Sciences (MUHS), Nashik was taken before commencing study. The present study included histopathological examination of surgical specimens like endometrial biopsies, D and C samples, hysterectomy specimens, and polypectomy specimens at the department of pathology in our institute.
The detailed clinical history was taken from the case records which included the following parameters age, and parity, a dominant clinical pattern of abnormal bleeding, radiological findings, operative findings, and clinical diagnosis.
Following inclusion and exclusion criteria were adopted in our study
Inclusion criteria: All the patients who were diagnosed clinically with Abnormal Uterine Bleeding (AUB) cases were included in the study.
Exclusion criteria: Women with pregnancy-related complications like (threatened/incomplete/missed miscarriage and ectopic pregnancy), gestational trophoblastic diseases, vaginal, cervical pathology, functional ovarian tumors, thyroid disorders, and hemostatic disorders were excluded from the study.
The surgical specimen and biopsies were fixed in 10% neutral buffer formalin, gross examination of the specimen was done, for assessing the appearance and extent of the lesion. In the case of endometrial biopsies, D and C samples whole tissue was submitted, and in hysterectomy specimen, the sections were taken in following orders i.e. Endometrium, myometrium, cervix, and associated lesion. Sections were processed according to standard protocol and stained with H and E stains and special stains were done whenever necessary. The clinical and histopathological data obtained were analyzed using the statistical package for social science (SPSS, Version 21) for windows.
Results
In this study spanning from January 2011-December 2012, 680 cases of abnormal uterine bleeding were collected from Gynaecology OPD and ward. The distributions of nature of sample are shown in Table 1. Out of 680 cases, 661 were endometrial lesions and in 19 cases no diagnosis was given because of an inadequate sample of D and C material, hence excluded from the study.
Table 1: Distribution of nature of sample (n=680)
| Nature of sample | No of Specimen | Percentage |
|---|---|---|
| Endometrial biopsy, D and C sample | 367 | 53.97% |
| Hysterectomy | 286 | 42.05% |
| Polypectomy | 27 | 3.97% |
| Inadequate sample | 19 | 2.79% |
| Total | 680 | 100% |
Among the 680 cases, the majority of cases were in the age group 41-50 years i.e. 271 cases (40.90%), followed by 193 cases (27.98%) belonging to 31-40 years of age (Table 2).
Table 2: Distribution of cases according to age group (n=661)
| Age Group | No. of cases | Percentage (%) |
|---|---|---|
| 21-30 | 80 | 12.10% |
| 31-40 | 193 | 27.98% |
| 41-50 | 271 | 40.90% |
| 51-60 | 81 | 12.25% |
| 61-70 | 33 | 4.99% |
| 71-80 | 3 | 0.45% |
| Total | 661 | 100 |
The incidence of AUB was high in grand multipara 319 (39.88%) cases and parity III 264 (33%) cases. This indicates that the incidence of AUB increases as parity increases.
In the present study, predominant pattern of AUB were reported as menorrhagia in 338 cases (51.13%), followed by intermenstrual bleeding in 115 cases (17.39%), polymenorrhagia in 79 cases (11.95%), while metrorrhagia was seen in 73 cases (11.04%) (Table 3).
Table 3: Distribution of bleeding pattern according to age group
| Age Group | Menorrhagia | Metrorrhagia | Polymenorrhagia | Menorrmetrorrhagia | Intermenstrual Bleeding | Total |
|---|---|---|---|---|---|---|
| 21-30 | 26 | 10 | 17 | 13 | 14 | 80 |
| 31-40 | 94 | 28 | 20 | 14 | 37 | 193 |
| 41-50 | 162 | 18 | 28 | 21 | 42 | 271 |
| 51-60 | 33 | 13 | 13 | 7 | 15 | 81 |
| 61-70 | 22 | 4 | 1 | 1 | 5 | 33 |
| 71-80 | 1 | 0 | 0 | 0 | 2 | 3 |
| Total | 338 (51.13%) | 73 (11.04%) | 79 (11.95%) | 56 (8.47%) | 115 (17.39%) | 661 |
Spectrum of endometrial findings, found in present study were proliferative endometrium was the most frequent finding 248 (36.47%), leiomyoma comprised of 100 cases (14.70%), adenomyosis 90 cases (13.23%), endometrial hyperplasia 72 cases (10.58%), secretory endometrium 47 cases (6.91%), atrophic endometrium 40 cases (5.88%), endometrial polyp 27 cases (3.97), endometritis 11 cases (1.61%), endometrial carcinoma 3 cases (0.44%) (Table 4).
Table 4: Age wise distribution of endometr ial lesions
| Age Group | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | 71-80 | Total |
|---|---|---|---|---|---|---|---|
| Proliferative endometrium | 40 | 76 | 92 | 33 | 7 | 0 | 248 (36.47%) |
| Secretory endometrium | 8 | 14 | 22 | 3 | 0 | 0 | 47 (6.91%) |
| Atrophic endometrium | 0 | 8 | 5 | 13 | 11 | 3 | 40 (5.88%) |
| Endometritis | 3 | 3 | 5 | 0 | 0 | 0 | 11 (1.61%) |
| Endometrial hyperplasia | 8 | 20 | 28 | 11 | 5 | 0 | 72 (10.58%) |
| Adenomyosis | 4 | 26 | 41 | 13 | 6 | 0 | 90 (13.23%) |
| Adenomyosis with leiomyoma | 2 | 6 | 14 | 1 | 0 | 0 | 23 (3.38%) |
| Leiomyoma | 14 | 30 | 51 | 3 | 2 | 0 | 100 (14.70%) |
| Endometrial polyp | 1 | 10 | 13 | 3 | 0 | 0 | 27 (3.97%) |
| Carcinoma of endometrium | 0 | 0 | 0 | 1 | 2 | 0 | 3 (0.44%) |
| Inadequate sample | 5 | 4 | 3 | 3 | 4 | 0 | 19 (2.79%) |
| Total | 80 | 193 | 271 | 81 | 33 | 3 | 680 (100%) |
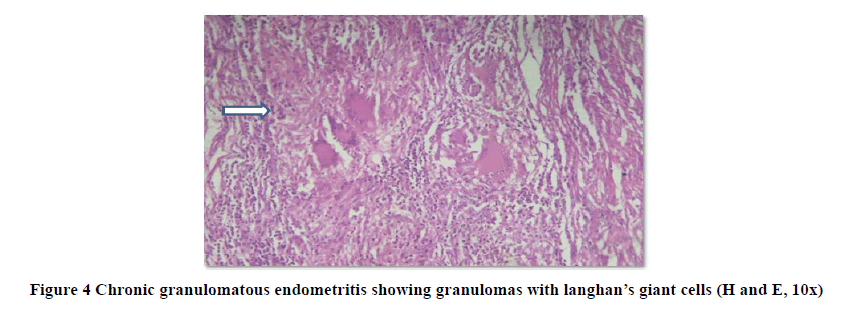
Out of 11 cases of endometritis, 10 cases (90.90%) were of chronic endometritis and 1 case (9.09%) of tubercular endometritis.
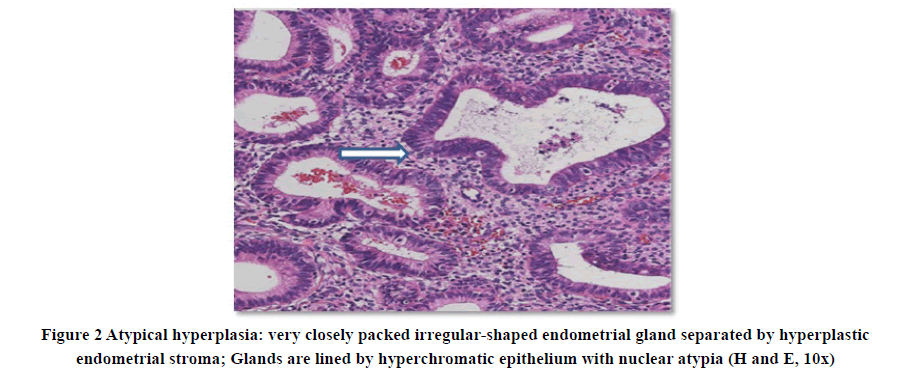
A total of 661 cases, 72 cases were endometrial hyperplasia. Out of 72 cases, hyperplasia without atypia constitutes 59 (81.94%) and atypical hyperplasia constitutes 13 cases (18.05%).
Discussion
AUB accounts for almost 25% of gynecological operations and 20% of outpatient visits [3].
Total 661 cases of AUB were studied to establish various causes of AUB and to analyze the distribution of histopathological findings with various age groups. Detail clinical data were noted from case records, which included age, parity, presenting complaints, associated complaints, operative findings, and diagnosis.
In the present clinicopathological study, AUB was commonly seen among 40-50 years of age group i.e. 271 cases (40.90%), the similar occurrence was reported by Bhatta S, et al., Sandeepa S, et al., Mahapatra M, et al., Rajagopal I, et al., Sharma R, et al. which shows a maximum number of cases were in similar age range comprised of 48 cases (39.34%), 122 (76.72%), 53 (38%) 81 (48.5%), 87 (47.5%) respectively (Table 5) [1,6,11-13].
Table 5: Comparison of age range with different studies
| Studies | Age range | No. of cases |
|---|---|---|
| [1] | 41-50 | 48 (39.34%) |
| [6] | 41-50 | 122 (76.72%) |
| [11] | 41-50 | 53 (38%) |
| [12] | 41-50 | 81 (48.5%) |
| [13] | 41-50 | 87 (47.5%) |
| Present study | 41-50 | 271 (40.90%) |
The most common bleeding pattern encountered in the present study was menorrhagia 338 (51.13%) which is comparable with the study by Mahapatra M, et al, and Rajagopal I, et al. [11,12].
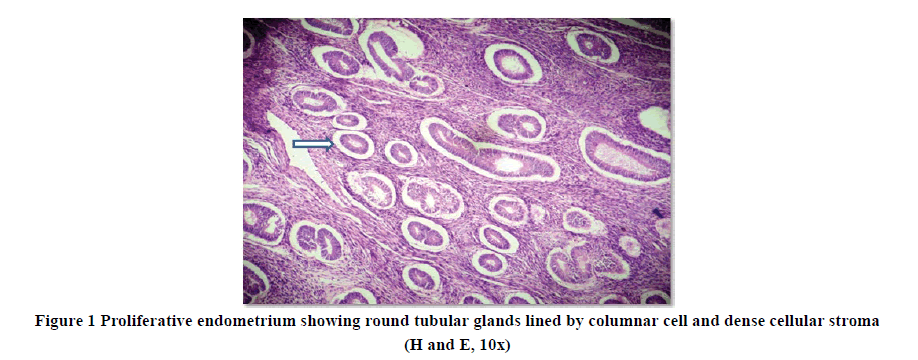
Table 6 represents the summary of various endometrial lesions and patterns of endometrium in AUB. The most common cyclic endometrial pattern seen in the present study was proliferative endometrium 248 cases (36.47%) (Figure 1), which was comparable with studies done by Sharma R, et al. 71 cases (38.8%), Sandeepa S, et al. 62 cases (38.99%) and Mahapatra M, et al. 64 cases (45.70%) however Rajagopal I, et al. had a lower incidence of proliferative pattern endometrium 15 cases (8.9%) [6,11-13]. This is followed by leiomyoma 100 (14.70%) cases with a maximum no. of patients falling in the age group of 31-40 years which is comparable with a study done by Ramachandran T, et al. 56 cases (22.9%) [14]. However study done by V. R SR, et al. had a higher incidence of (54%) [15].
The third commonest lesion was endometrial hyperplasia (Figure 2) observed in 72 (10.58%) cases with its maximum number of patients falling in the age group of 31 to 40 years which is comparable with the study done by Sharma R, et al. 22 (12.0%) and is in discordance with the studies done by Sandeepa S, et al. 59 (37.10%), Rajagopal I, et al. 38 (22.6%), who observed a high incidence of endometrial hyperplasia [6,12,13]. Identification of endometrial hyperplasia is important because they are thought to be precursors of endometrial carcinoma [3].
Table 6: Comparison of endometrial lesions with different studies
| Endometrial Patterns | Present study | Sharma R, et al. [13] | Sandeepa S, et al. [6] | Rajagopal I, et al. [12] | Mahapatra M, et al. [11] |
|---|---|---|---|---|---|
| Proliferative endometrium | 248 (36.47%) | 71 (38.8%) | 62 (38.99%) | 15 (8.9%) | 64 (45.70%) |
| Secretory endometrium | 47 (6.91%) | 30 (16.3%) | 20 (12.57%) | 40 (23.9%) | 42 (30%) |
| Atrophic endometrium | 40 (5.88%) | 08 (4.4%) | 6 (3.77%) | 19 (11.3%) | 7 (5.00%) |
| Endometritis | 11 (1.61%) | 06 (3.3%) | 3 (1.88%) | - | |
| Endometrial hyperplasia | 72 (10.58%) | 22 (12.0%) | 59 (37.10 %) | 38 (22.6%) | 17 (12.10%) |
| Adenomyosis | 90 (13.23%) | - | - | - | - |
| Adenomyosis with leiomyoma | 23 (3.38%) | - | - | - | |
| Leiomyoma | 100 (14.70%) | - | - | - | |
| Endometrial polyp | 27 (3.97%) | 04 (2.2%) | - | 05 (3.60%) | |
| Carcinoma of endometrium | 3 (0.44%) | 02 (1.1%) | 5 (3.14%) | 3 (1.7%) | 01 (0.70%) |
| Inadequate sample | 19 (2.79%) | 11 (6.0%) | - | ||
| Total | 680 (100%) |
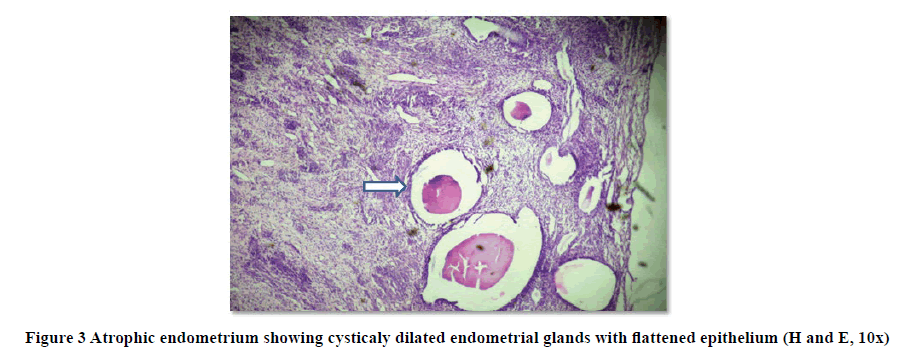
Postmenopausal bleeding is frequently associated with an atrophic endometrium.
The number of cases with atrophic endometrium (Figure 3) constitutes 40 cases (5.88%) in the present study which is in concordance with the study done by Sharma R, et al., Sandeepa S, et al., Mahapatra M, et al. [6,11,13].
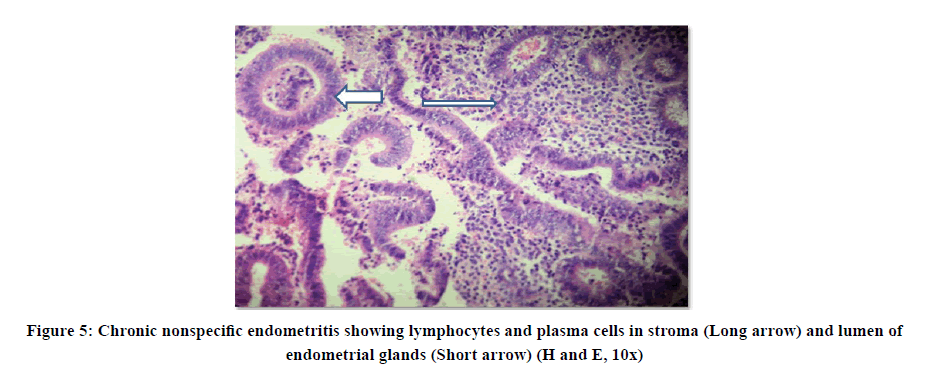
Endometritis was seen in 11 cases (1.61%), out of which 1 case showed necrotizing granulomatous endometritis i.e. caseating granulomas, Langhans type of giant cells, areas of necrosis (Figure 4), and the remaining 10 cases showed chronic endometritis (Figure 5).
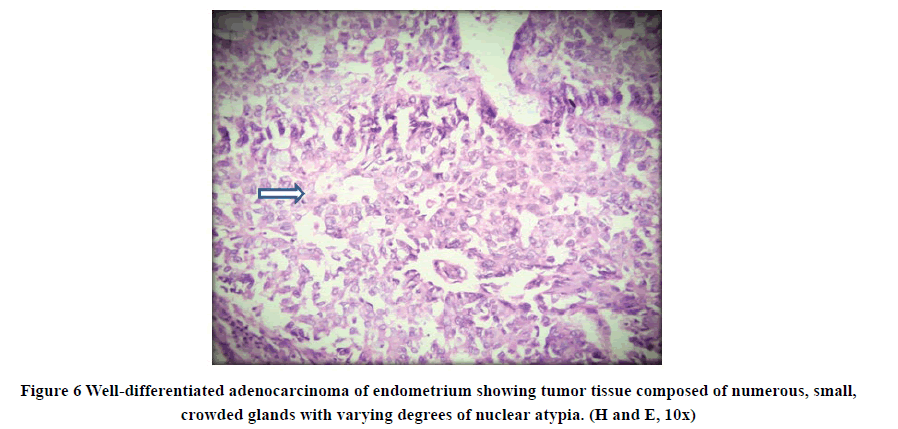
In this study endometrial carcinoma (Figure 6) constituted only 3 (0.44%) of cases. A similar incident was reported by Mahapatra M, et al. 01 (0.70%) [11].
The concomitant lesion was seen in 23 (3.66%) which constitute adenomyosis with leiomyoma.
Conclusion
In the present study, there is a high prevalence of heavy menstrual bleeding in peri-menopausal age with the highest prevalence between the ages of 40-50 years. The information presented in this study adds to our understanding of the common causes of abnormal uterine bleeding. Histopathological examination of the endometrium revealed that proliferative endometrium is the most common pattern. Among the organic pathological causes, leiomyoma is the commonest cause followed by adenomyosis. Endometrial sampling is a simple cost-effective and appropriate method that provides an accurate diagnostic step in abnormal uterine bleeding. Histopathological examination of endometrium in patients of AUB shows a wide spectrum of changes ranging from normal endometrium in various hormonal cycles to malignancy. AUB needs thorough and prompt evaluation as it could be the only clinical manifestation of endometrial malignancy.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
This article could not have been compiled without the able guidance of Dr. Shubha Deshpande, Professor, and Head of Department of Pathology, Dr. Shankarrao Chavan, Government Medical College, Nanded, Maharashtra, India.
References
- Bhatta, S., and A. K. Sinha. "Histopathological study of endometrium in abnormal uterine bleeding." Journal of Pathology of Nepal, Vol. 2, No. 4, 2012, pp. 297-300.
- Devi, Junu, and N. Aziz. "Study of histopathological pattern of endometrium in abnormal uterine bleeding in the age group 40-60 years. A study of 500 cases." International Journal of Medical Science and Clinical Inventions, Vol. 1, No. 10, 2014, pp. 579-85.
- Sajitha, K., et al. "Study of histopathological patterns of endometrium in abnormal uterine bleeding." Chrismed Journal of Health and Research, Vol. 1, No. 2, 2014, pp. 76-81.
- Mirza, Talat, et al. "Histopathological pattern of abnormal uterine bleeding in endometrial biopsies." Journal of Basic and Applied Sciences, Vol. 8, No. 1, 2012, pp. 114-17.
- B. S. Vani, R. Vani, and Jijiya Bai P. "Histopathological evaluation of endometrial biopsies and curetting’s in abnormal uterine bleeding." Tropical Journal of Pathology and Microbiology, Vol. 5, No. 4, 2019, pp. 190-97.
- Sandeepa, Supriya, H. T. Jayaprakash, and M. C. Ashwini. "Abnormal uterine bleeding: Histopathological patterns of endometrium in elderly." Indian Journal of Pathology and Oncology, Vol. 3, No. 4, 2016, pp. 662-64.
- Desai, Kairavi, Kiran P. Patole, and Manasi Kathaley. "Endometrial evaluation by histopathology in abnormal uterine bleeding in perimenopausal and postmenopausal patients." MVP Journal of Medical Science, Vol. 1, No. 2, 2014, pp. 75-79.
- Neena, Yogesh, and Bhaskar Honey. "Clinico-pathological correlation of hysterectomy specimens for abnormal uterine bleeding in rural area." Journal of Evolution of Medical and Dental Sciences, Vol. 2, No. 39, 2013, pp. 7506-12.
- Kumar, Pratap, Sir Norman Jeffcoate, and Narendra Malhotra. "Jeffcoate's principles of gynaecology." Butterworths, 2008.
- Sharma, Kavita, and Akta Rasania. "Clinicopathological spectrum of endometrial biopsies in a tertiary care center." Internatinal Journal of Scientific Research, Vol. 8, No. 11, 2019, pp. 4-7
- Mahapatra, Mitali, and Pratima Mishra. "Clinicopathological evaluation of abnormal uterine bleeding." Journal of Health Research and Reviews, Vol. 2, No. 2, 2015, pp. 45-49.
- Rajagopal, Indu, Beena Mary Thomas, and Vidyadhar N.K. Rama Rao. "Endometrial pathology in abnormal uterine bleeding." International Journal of Research in Medical Sciences, Vol. 7, No. 10, 2019, pp. 3762-66
- Sharma, Ritu, et al. “Histomorphological spectrum of endometrial lesion in women presenting with abnormal uterine bleeding: A 3-year study at a tertiary care center”. Tropical Journal of Pathology and Microbiology, Vol. 4, No. 7, 2018, pp. 525-31.
- Ramachandran, Thamilselvi, and Pammy Sinha. "Subramanium. Correlation between clinico-pathological and ultrasonographical findings in hysterectomy." Journal of Clinical Diagnosis and Research, Vol. 5, No. 4, 2011, pp. 737-40.
- Rani, VR Sreeja, and Sindha Thomas. "Leiomyoma, a major cause of abnormal uterine bleeding." Journal of Evolution of Medical and Dental Sciences, Vol. 2, No. 16, 2013, pp, 2626-31.