Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 7
Clinical Validation of Novel Smartphone-Based Spirometer for Measurement of Obstructive Diseases
Shardul Joshi* and Gajanan SakhareShardul Joshi, Division of Respiratory Health, Department of Research and Development, BRIOTA Technologies Private Limited, Pune, Maharashtra, India, Email: shardul@briota.com
Received: 02-Jun-2021 Accepted Date: Jul 23, 2021 ; Published: 30-Jul-2021
Abstract
Introduction: Spirometry, despite being the gold-standard diagnostic test for obstructive airway diseases, is underutilized in clinical practice. It is widely used to assess lung function and provide objective data for lung disease diagnosis and monitoring. Real-life conditions are less ideal because of comorbidities, age of the subjects, and a variety of airflow limitations. BRIOTA Technologies Private Limited has developed a portable and point-of-care diagnostic tool for Asthma and obstructive diseases. Objective: This descriptive and cross-sectional prospective study was carried out in the respiratory ward of a Semi-Government hospital located in Pune, Maharashtra, India. In this study, 126 patients with Chronic Obstructive Pulmonary Disease (COPD) and asthma were enrolled, with only a handful of them being healthy. SpiroPROTM is a turbine-based electronic measuring device integrated with an intuitive mobile application to perform spirometry analysis and generate a spirometry report. Furthermore, the apparatus allows us to incorporate a vital parameter representing Forced Expiratory Volume (FVC), Forced Expiratory Volume in the first second (FEV1) into the final diagnosis. Methods: We compared volumetric parameters as well as inhalation parameters using an Easy-ware air Spirometer device, a conventional spirometer to a house-developed SpiroPROTM device, and analyze the ability of this new portable device to detect obstructions and restrictions. Results: The concordance and relation of the FEV1 and FVC parameters were optimal. We used the absolute values as well as the percentages to make this comparison. The greatest difference in the measurement was in the FVC, which was 77.95 ml (95% CI: 38 to 117). Conclusion: This SpiroPROTM Spirometer device is a simple, easy-to-use, and highly accurate technology that may be used to screen and diagnose chronic respiratory disorders.
Keywords
Spirometry, SpiroPROTM, FVC, Chronic obstructive pulmonary diseases, Asthma
Introduction
Millions of people around the world suffer from Chronic Obstructive Pulmonary Disease (COPD) and asthma, the two most common respiratory diseases that can have serious health consequences and even lead to death [1]. Patients with asthma and COPD should measure static and dynamic respiratory functions daily to keep a record of their pulmonary health and avoid complications [2]. The most common machines for such tests are spirometers [3]. They evaluate lung function and provide a first-level diagnostic test for pulmonary diseases and disease progression by measuring the volume and speed of air inhaled and exhaled [4]. Spirometry is the gold-standard, guideline-recommended test for Obstructive Airway Diseases (OADs), such as asthma and Chronic Obstructive Pulmonary Disease (COPD) [5]. It also aids in the differentiation of the two diseases as well as delivers a better index of severity and prognosis and helps in the selection of suitable pharmacotherapy [6,7]. Spirometry is a physiological test that determines the maximum amount of air a person can inhale and exhale while exerting maximum effort. In spirometry, the primary signal is either volume or flow as a function of time. The FVC, which is the volume delivered during a forceful and complete expiration beginning with full inspiration, and the FEV1, which is the expiratory volume in the first second of an FVC maneuver, are the two most significant measurements discussed in this document.
Spirometers are divided into two categories-laboratory and portable [8]. Spirometers in laboratories are either desktop devices or cabinet-size machines that are typically found in hospitals and are operated by trained technicians [9]. Even though they can provide precise spirometry measurements and conduct systematic tests on flow volume, tidal spirometry, and maximum voluntary ventilation, patients find it inconvenient and costly to visit the hospital every day for the test. The use of laboratory spirometers by primary care providers is limited due to their high cost. Spirometers for general practice and home use are usually compact desktop units or handheld devices [9,10]. They are compact and consume little power. Low cost is another important feature of these spirometers, making them more accessible to a larger user base.
In India, the number of people with COPD increased from 281 million in 1990 million to 553 million in 2016, with a prevalence rate of 33% to 42%. In 2016, the less developed state group had the highest age-standardized COPD prevalence and DALY (Disability Adjusted Lives Yearly) rates. In 2016, India had 379 million asthma cases, with similar prevalence across different state groups. Population-based studies in children, adults, and the elderly suggest that 20 percent to 70 percent of people with asthma in the community are undiagnosed and thus untreated [11].
This has resulted in the development and commercialization of several portable devices that allow for the rapid collection of Spirometric parameters, making them particularly useful in the screening of respiratory diseases in nonspecialized care areas [12].
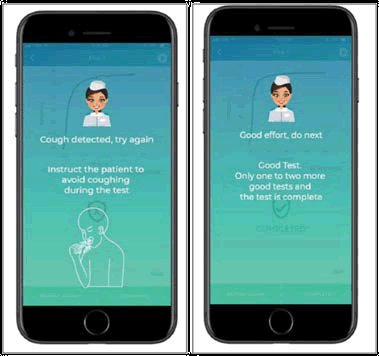
BRIOTA Technologies Private Limited has developed a portable and point-of-care diagnostic tool for the assessment of asthma, COPD, and other respiratory ailments. SpiroPROTM is a turbine-based electronic measuring device integrated with an intuitive mobile application to perform spirometry analysis and generate a spirometry report. This SpiroPROTM spirometer is very easy to use because of its simple design, audio-visual guidance for correct positioning of the device, and test progression indicator during spirometry maneuver the fact that mobile app provides real-time feedback about acceptable spirometry, and the cardboard mouthpieces are disposable and one-time use.
Material and Methods
Design
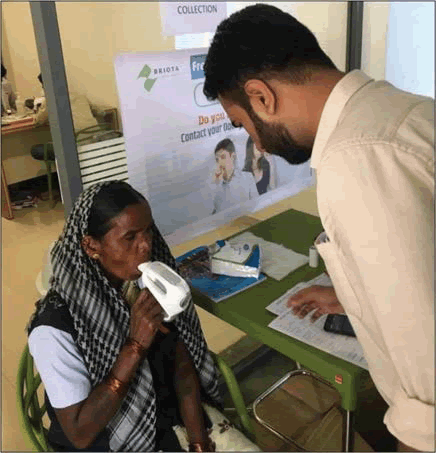
SpiroPROTM, a device developed by BRIOTA technologies using turbine transducer technology, has been validated by comparing spirometry values with those of conventional gold standard devices such ndd EasyOne Air Spirometer as shown in figure 1. This SpiroPROTM requires a disposable mouthpiece and filter, which are easily available in the market.
The study was carried out at a single center with great potential and was considered a descriptive and cross-sectional study. As a part of an example shown in figure 2, we included 126 patients from the Semi-Government Hospital’s chest ward who were suffering from COPD and asthma, as well as some who were healthy.
Validation was done on all spirometry parameters, including volumetric ones like FVC, FEV1, FEV1/FVC, flow rate parameters like PEF, MEF 25, MEF 50, MEF 75, MEF 25-75, and inhalation parameters like FIVC and PIF.
Subjects
A total of 126 patients with Chronic Obstructive Pulmonary Disease (COPD) and asthma were involved in this study, with only a few of them being healthy. Each participant was informed about the study and gave their consent orally. The study excluded patients with hemodynamic instability, pulmonary embolism, recent pneumothorax, acute hemoptysis, active respiratory infections, and myocardial infarction. Special cases, such as pregnancy, obesity, and bedridden people, were also excluded from the study.
All patients were subject to the classical EasyOne Air Spirometer and the SpiroPROTM Spirometer, to obtain satisfactory and reproducible criteria following SEPAR requirements [13].
Spirometry performed by the patients was considered acceptable if it commenced quickly and without hesitation. During this spirometry process, the expiratory maneuver should be continuous, and the end of the maneuver should not show any early or abrupt interruptions without artifacts or evidence of coughing in the first second.
The two best acceptable VC, IC, FVC, and FEV1 values should have a difference of less than 0.15.
Trial Design
The EasyOne Air device was used to perform traditional spirometry with an ultrasonic transducer. This sensor calculates flow using the proportional time of flight concept and airflow interference. The calibration for the sensor is done on daily basis with a 3-liter syringe and further subjected to temperature, humidity, and altitude adjustment. Along with this daily calibration, a weekly calibration of flow linearity is also carried out using a 1-liter syringe. For spirometry reference values of Asian ethnic people, this Easy-ware Air employs NHANEES III.
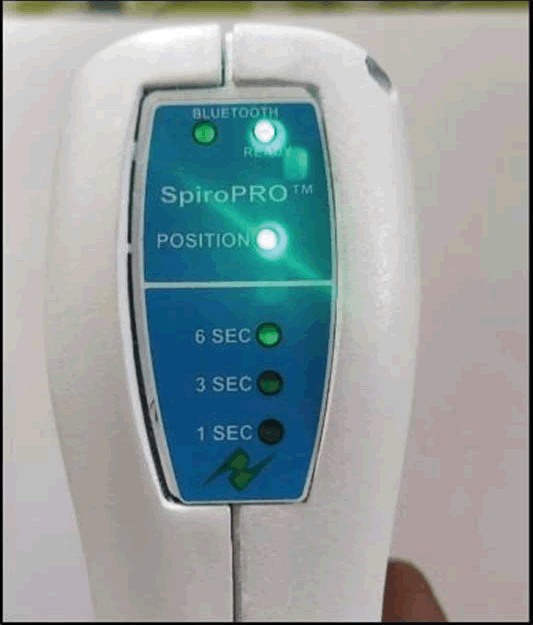
The SpiroPROTM spirometer is a small portable device that communicates with the digital interface. Bluetooth. It measures 79 × 56 × 20 mm and weighs 50 grams. It comes with a 500 mAh 3.7 v lithium polymer rechargeable battery with a 2-year half-life. It uses a turbine mechanism (like Flow Mir) to take measurements inside single-use disposable mouthpieces. There is no calibration required for the equipment, however, age, sex, and height information must be entered before spirometry takes place.
Once the user switches on the device, the buzzer will turn on with red led and the user will be guided to hold the device in a horizontal position for accurate spirometry maneuverer. Once the device is in the correct position, the buzzer and red led will go off and the green led will light up indicating test readiness. The user exhales into the turbine pipe to perform spirometry. This air turns a turbine, and the device keeps track of how many times the turbine fan rotates. Further, the data is recorded in time, and the data is transferred to the software application on the smartphone. An LED pattern is activated when the patient initiates exhalation and white LED lights up after completion of 1st second, 3rd second, and then 6th-second indicating minimum exhalation of 6 seconds is achieved in maneuverer after 6 seconds of exhalation as shown in Figure 3. Once spirometry maneuverer is complete and data is shared to a mobile app through Bluetooth as communication media, a message will be seen on the device if acceptable spirometry is achieved or not. To calculate the percentages of FEV1 and FVC, the SpiroPROTM system uses reference values validated in the NHANES III study [14,15].
To record the observation and choose the one with the highest sum of FEV1 and FVC, a minimum of three Spirometric maneuvers (triplicates) were performed as per ATS/ERS guidelines [16].
Statistical Analysis
All statistical analyses were performed by using the Statistical Package for Social Sciences (SPSS for Windows version 17.0, SPSS Inc., Chicago, US) and Medcalc for Windows MedCalc for Windows, version 12.5 (MedCalc Software, Ostend, Belgium).
The qualitative variables were reported as absolute values and percentages, whereas the quantitative data were represented as means and standard deviations.
The variations between the parameters studied were presented using the mean of the difference at a 95% confidence interval. The comparison of the quantitative variables was carried out by applying the student’s t-test for paired samples, and a p-value equal to or less than 0.05 was considered statistically significant. The kappa index was used to evaluate the concordance between the two devices for the detection of obstruction (FEV1/FVC ratio<70%) as a qualitative variable.
The agreement and relation between the values of FEV1 and FVC in absolute value and the FEV1/ FVC ratio measured by both devices were analyzed by calculating the Intra Class Correlation Coefficient (ICC) and the Pearson correlation coefficient (r) respectively and were plotted using Bland and Altman graphics and correlation plots.
Results
A total of 126 patients with respiratory ailments have undergone spirometry with both conventional and newly developed SpiroPROTM. Tests were conducted at a semi-government chest OPD hospital in Pune, Maharashtra with a mean age of 45 years, out of which 72 were male and 52 were female subjects.
The validity and safety of the SpiroPROTM Spirometer in the detection of obstruction were determined using the usual equations, and the sensitivity, specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), and Positive/Negative Likelihood Ratios (LR+, LR-) were calculated.
The sample size was based on the experience of the group invalidation of other devices, estimating that the Air Smart Spirometer could present sensitivity of 90% and a specificity of 80% in the detection of obstruction, a prevalence of the same of 40%, and an alpha error of 5% [12,15]. This study followed the STARD recommendations for the evaluation of diagnostic tests [6].
The absolute and percentage values of the different parameters measured with the conventional spirometer and the Air Smart Spirometer are shown in Table 1. The mean of the differences and the 95% confidence level are also included. The values obtained with the Easy-ware Spirometer were significantly higher for the absolute value of FEV1 (p=0.012) and FVC (p=0.027). There was no significant difference in FEV1/FVC ratio (p=0.205) as indicated in Table 1. The concordance and correlation between the parameters of the two devices were FEV1-(SpiroPROTM spirometry) vs. FEV1 (EasyOne Air Spirometer) ICC=0.90 (p<0.001), r=0.89 (p<0.001).
| Parameters | Spiro (Mean ± Std. Deviation) | Easy (Mean ± Std. Deviation) | Significance (p) |
|---|---|---|---|
| FEV1 | 1.610 ± 0.891 | 1.888 ± 0.949 | 0.012 |
| FVC | 2.440 ± 1.091 | 2.547 ± 1.053 | 0.027 |
| FEV1/FVC | 0.662 ± 0.272 | 0.716 ± 0.146 | 0.293 |
The concordance and relation of the FEV1 and FVC parameters were optimal. We used the absolute values as well as the percentages to make this comparison. The greatest difference in the measurement was in the FVC, which was 77.95 ml (95% CI: 38 to 117). The kappa index was 0.31, sensitivity (81.6%), specificity (53.2%), PPV (52.6%), NPV (82.0%), positive likelihood ratio (1.75%), and negative likelihood ratio (0.34), using an FEV1/FVC ratio lower than 0.7 to detect obstruction with the Easy Spirometer. The ICC between FEV1 and FVC measured by the Easy Spirometer and the conventional spirometer were all higher than 0.90.
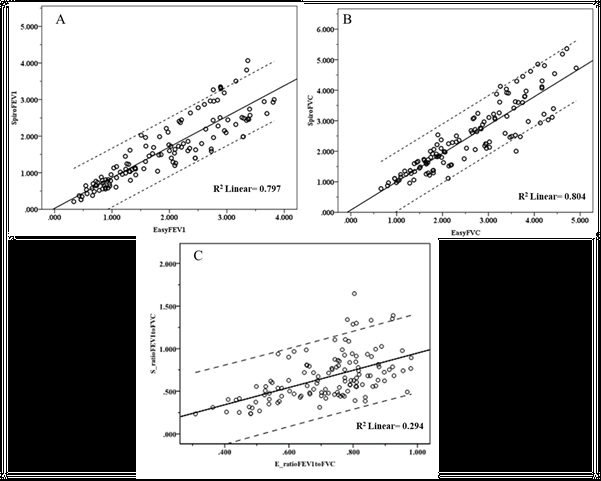
The concordance and correlation between the parameters of the two devices were FEV1 (SpiroPROTM Spirometer) vs. FEV1 (Easy-ware Spirometer) ICC=0.94 (p<0.001), r=0.89 (p<0.001), FVC (SpiroPROTM Spirometer) vs. FVC (Easy-ware Spirometer) ICC=0.94 (p<0.001), r=0.89 (p<0.001), FEV1/FVC (SpiroPROTM Spirometer) vs. FEV1/FVC (Easy-ware Spirometer) ICC=0.62 (p<0.001), r=0.54 (p<0.001) as shown in Table 2.
| Parameters | ICC | R |
|---|---|---|
| FEV1 | 0.94 (p<0.001) | r=0.89 (p<0.001) |
| FVC | 0.94 (p<0.001) | r=0.89 (p<0.001) |
| FEV1/FVC | 0.62 (p<0.001) | r=0.54 (p<0.001) |
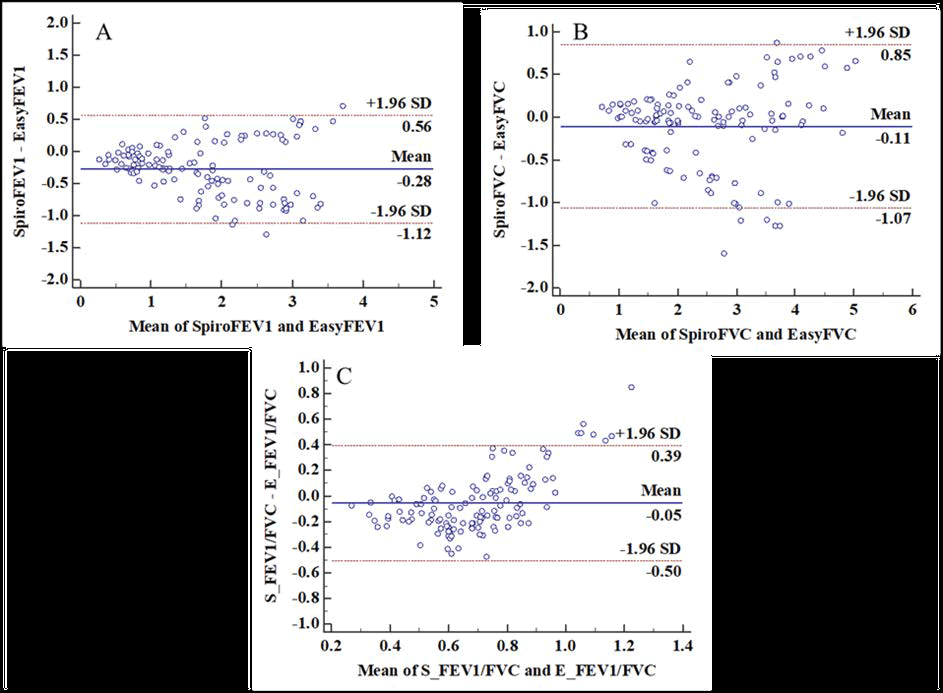
The graphs presented in Figure 4 are Bland and Altman graphs in which a homogeneous distribution can be observed. As shown in Figure 4A Bland-Altman’s analysis showed that the standard deviation of the difference between FEV1 measured by two methods was 0.35 g/dL and the limits of agreement between the two methods were -1.12 to 0.56. A similar analysis was carried out for FVC and FEV1/FVC as shown in Figure 4B and Figure 4C, respectively.
The linear least-squares regression analysis (Figure 5) showed a significant correlation between the FEV1 and FVC values obtained from both methods. However, we did not find a significant correlation between FEV1/FVC values.
Table 3 shows a contingency table for patients diagnosed with airway obstruction with conventional spirometry and Easy Smart Spirometer. Airway obstruction is defined in both cases as FEV1/FVC ratio lower than 0.7.
| SpiroPROTM Spirometer | Easy-ware Spirometer | |||
|---|---|---|---|---|
| No Obstruction | Obstruction | No Obstruction | Obstruction | |
| Count | 76 | 50 | 78 | 48 |
| Total | 126 | 126 | ||
Discussion
This article summarizes the findings of an independent investigation conducted with a handheld SpiroPROTM spirometer. Most of the observations gave excellent results. In this investigation, the SpiroPROTM satisfied criteria for repeatability and validity for the FEV1 and FVC. SpiroPROTM spirometer performance was shown to be on par with EasyOne Air spirometer performance SpiroPROTM, on the other hand, proved to be more user-friendly than the EasyOne Air spirometer.
Spirometry is the gold standard and approved diagnostic test for Obstructive Airway Diseases (OADs), including Asthma and CPD (COPD) [5]. It helps to differentiate between both diseases, offers a useful gravity and prognostic index, and guides suitable pharmacotherapy [6,7].
Despite being the highly recommended diagnostic test for obstructive airway diseases, spirometry is underutilized in clinical practice [17,18]. Chronic respiratory diseases are likely underdiagnosed because of these factors [18]. The use of high-quality spirometry is also required in this line of work.
To date, several portable spirometers have been validated, including the MIR spirometer, a similar small device that uses the expiratory flow in 6 seconds (FEV6) to replace FVC in obstruction detection. Using an FEV1/FEV6 ratio of 0.8, the Vitalograph COPD-6 device was validated and demonstrated to be a useful tool for screening for obstructive respiratory diseases in a non-specialized area [15].
Most validated portable devices do not allow users to display flow/volume or volume/time loops, making it difficult to assess potential bias in the technique. Others, like the Easy-ware Spirometer, use ultrasounds to assess flow rates. This allows the volume/flow loop to be displayed, but the device is quite costly, and the results of a volunteer test have shown correlations in FVC, but not in FEV1 [18].
In the light of current technological progress, the increase in COPD and the aging of the population for the next few years require a rapid and accurate diagnosis. Computing and medicine are a current example of scientific discipline integration and a nexus between science, technology, and society.
The SpiroPROTM Spirometer is very accessible because of its design, which allows for easy handling, audio-visual guidance for correct positioning of device and test progression indicator during spirometry maneuver and the fact that mobile app provides real-time feedback about acceptable spirometry, and the cardboard mouthpieces are disposable and one-time use.It can be linked to any enabled interfaces of Bluetooth that can be used after “NEHA” mobile app installation (google play store) as depicted in Figure 6. This allows, unlike other portable devices, a Spirometric loop visualization, enhancing the results and allowing a critical evaluation of the maneuvers. The pathologies of the upper airway may even be diagnosed by the loop’s morphology [13].
We are the first to analyze the validity and safety of the SpiroPROTM Spirometer and conclude that it is of excellent validity when compared to the gold standard for the diagnosis of obstruction (conventional spirometry). FEV1 and FVC parameters were optimally aligned and correlated. For this comparison, we used the absolute values and the percentages. The largest measuring difference was 77.95 ml in the FVC (95 percent CI: 38 to 117). This may be associated with the Spirometric or ultrasound sensing techniques, as this is the known parameter for more discord in the comparison of studies conducted. Nevertheless, the limits included in the trust interval meet the criteria for reproductivity
Figure 4 and Figure 5 shows Bland-Altman plots of the difference between measures from the two spirometers compared to the mean value from two spirometers for FVC and FEV1. The plot for FVC and FEV1 suggested that the difference between measures from the spirometers was proportional to mean FVC, and linear regression confirmed that the slope of the line on the Bland-Altman plot was statistically significantly different. The plot for FEV1/FVC showed less proportionality that was not statistically significant. Additionally, as shown in Table 1, there was no significant difference in the FEV1/FVC ratio obtained by these two devices indicating the accuracy of the SpiroPROTM.
The concordant measurements are useful in the early detection of chronic respiratory illnesses and can be more valued as normal values exclude aerial obstruction with acceptable safeguarding in the field of non-specialized care. It can be used for rapid assessments in spirometry screenings because of its easy use and aesthetic look. Users can save data and view or retrieve records from the database directly via. the software.
The current study has several limitations. First, the study was conducted by hospital technicians and may limit the external validity in other areas with less experienced professionals.
To assess their validity at this level, further studies are required in other areas such as remote care, bed care, and emergencies. On the contrary, the interrupting point used to detect an airflow obstruction was FEV1/FVC<0.7, because of its potential in current, especially at age levels this index is controversial (both young and old).
At present, most authors support the idea that under-diagnosis and overdiagnosis in older adults are prevented with the lower limit of regularity [19]. However, the FEV1/FVC ratio<0.7 was considered more suitable in this respect to facilitating diagnoses to validate new device measures.
Conclusion
This article proposes a smart SpiroPROTM Spirometer device with multiple objectives. The developed model is portable, with a user-friendly interface configured over consistent and reliable hardware. Bluetooth is communication technology, and it contains all data required by patients and doctors. With real-time feedback through mobile apps and audio-visual guidance on the device for acceptable spirometry, it becomes easier to adhere to the right practices as provided by ATS (American Thoracic Society). The results using this portable device were found to be accurate, chronologically recorded, and simple to interpret to make the best possible decisions regarding medication, treatment stages, and hospitalization. This SpiroPROTM Spirometer device is simple, manageable, and very precise as it comprises analysis of the Forced Vital Capacity for better diagnosis. As compared to conventional spirometry, our study is the first to examine the validity and safety of the SpiroPROTM Spirometer gadget, and we conclude that it has outstanding legitimacy for the diagnosis of obstruction and possible restriction. Using this device, the FEV1 and FVC values were found to be in optimum concordance which proves the aesthetic value of the device. Because of its ease of use and attractive appearance, it could be used to perform rapid assessments in spirometry screenings. Users can save the results and view or retrieve the records directly from the database using the software.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgment
This article could not have been compiled without the guidance and support of BRIOTA technologies private limited.
References
- Chronic respiratory diseases: Asthma. World Health Organization. 2020. https://www.who.int/news-room/q-a-detail/chronic-respiratory-diseases-asthma
- Brunelli, Alessandro, et al. "Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer: American College of chest physicians evidence-based clinical practice guidelines." Chest, Vol. 143, No. 5, 2013, pp. e166S-90S.
- Binu, E. M. N. S., and N. S. Varsha. "Real time monitoring of respiratory parameters using a wireless portable system." International Journal of Engineering Development and Research, Vol. 3, No. 1, 2014, pp. 283-87.
- Hankinson, J. L., et al. "Method to produce American Thoracic Society flow-time waveforms using a mechanical pump." European Respiratory Journal, Vol. 10, No. 3, 1997, pp. 690-94.
- Pierce, Rob. "Spirometry: An essential clinical measurement." Australian Family Physician, Vol. 34, No. 7, 2005, pp. 535-39.
- Yawn, Barbara P., et al. "Spirometry can be done in family physicians' offices and alters clinical decisions in management of asthma and COPD." Chest, Vol. 132, No. 4, 2007, pp. 1162-68.
- O’donnell, Denis E., et al. "Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease-2003." Canadian Respiratory Journal, Vol. 10, No. Suppl A, 2003, pp. 11A-33A.
- Hudson, Jessica L., et al. "Office-based spirometry: A new model of care in preoperative assessment for low-risk lung resections." The Annals of Thoracic Surgery, Vol. 105, No. 1, 2018, pp. 279-86.
- Maree, D. M., et al. "Comparison of a new desktop spirometer (Diagnosa®) with a laboratory spirometer." Respiration, Vol. 68, No. 4, 2001, pp. 400-04.
- Dieffenderfer, James P., et al. "Wearable wireless sensors for chronic respiratory disease monitoring." 2015 IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), IEEE, 2015.
- Aaron, Shawn D., et al. "Underdiagnosis and overdiagnosis of asthma." American Journal of Respiratory and Critical Care Medicine, Vol. 198, No. 8, 2018, pp. 1012-20.
- Represas-Represas, Cristina, et al. "Screening for chronic obstructive pulmonary disease: Validity and reliability of a portable device in non-specialized healthcare settings." PLoS One, Vol. 11, No. 1, 2016, pp. 1-11.
- Ramos Hernández, Cristina, et al. "Validation of the portable air-smart spirometer." PLoS One, Vol. 13, No. 2, 2018, pp. 1-11.
- Chhabra, S. K., et al. "Prediction equations for spirometry in adults from northern India." Indian Journal of Chest Diseases & Allied Sciences, Vol. 56, No. 4, 2014, pp. 221-29.
- Represas, Cristina Represas, et al. "Assessment of the portable COPD-6 device for detecting obstructive airway diseases." Archives of Bronconeumology, Vol. 46, No. 8, 2010, pp. 426-32.
- Graham, Brian L., et al. "Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement." American Journal of Respiratory and Critical Care Medicine, Vol. 200, No. 8, 2019, pp. e70-e88.
- Vanjare, Nitin, et al. "Use of spirometry among chest physicians and primary care physicians in India." NPJ Primary Care Respiratory Medicine, Vol. 26, No. 1, 2016, pp. 1-5.
- Barr, R. Graham, et al. "Reproducibility and validity of a handheld spirometer." Respiratory Care, Vol. 53, No. 4, 2008, pp. 433-41.
- Quanjer, P. H., et al. "The need to change the method for defining mild airway obstruction." European Respiratory Journal, Vol. 37, No. 3, 2011, pp. 720-22.