Case Report - International Journal of Medical Research & Health Sciences ( 2021) Volume 0, Issue 0
Basal Ganglia infarct following minor head trauma in a child: Case report and review of literature
Nisreenbader* and NuhaAlzaabiNisreenbader, Department of Radiology & Fujairah hospital, Emirates health services, Ministery of health and prevention, UAE, Email: dr.nanone@hotmail.com
Received: 07-Aug-2021 Accepted Date: Aug 13, 2021 ; Published: 28-Aug-2021
Abstract
Background: Basal ganglia infarct as a consequence of minor head trauma is rare in children, however clinical history of such lesions is been favourable . Here we report a 5-year-old girl who presented with left side hemiparesis and sensory loss after a fall. Diffusion weighted magnetic resonance imaging showed an acute infarct in the right basal ganglia region. Genetic, metabolic, cardiac and haematological causes of stroke were ruled out.A conservative therapeutic approach of such cases is considered most effect up to date, although the best regimen is not defined yet.
Mild head trauma is an independent risk factor leading to ischemic stroke with unclear pathophysiology. Presence of genetic, metabolic and haematological causes must be excluded. In the following report we discuss the incidence, risk factors and possible mechanisms leading to such cases.
Keywords
Hemiparesis, Basal ganglia infarct, Head trauma, Stroke
Introduction
Blunt Head traumas are common events reported in the pediatric age group; often not associated with long term neurological sequelae. Nevertheless, pediatric ischemic strokes (with incidence of 1.9%) as a complication, are been reported and hence it’s important to identify such cases. Although the exact pathogenesis remains unclear, however basal ganglia infarcts in infants and young children are believed to be due to vasospasm or thrombosis of lenticulostriate arteries- originating from the middle cerebral artery [1]. Focal dissection of such has also been hypothesized. Although the best treatment regimen is still not well defined,however; conservative approach remains the most effective up to this date.
Here we report a case presenting with neurological deficit following a minor head injury probably due to ischemia of small vessel territories at the basal ganglia.
Case Description
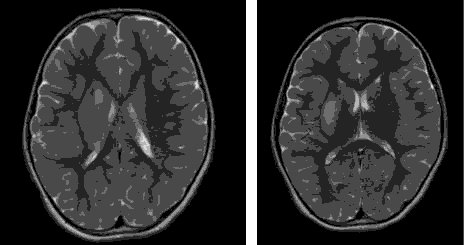
A 5-year-old girl, not known to have any medical problems, with history of minor head trauma after a fall from bed. Patient cried immediately and there was no loss of consciousness. On the following day, she was noted by parents not using her left arm and left leg. Clinical examination confirmed left sided hemiparesis with impairment of sensation on the same side. MRI of the braindone three days later, reported acute infarction involving the right globuspallidus, putamen and part of posterior limb of internal capsule. Normal MRV\MRA studies of the cerebral vessels. To rule out the possibility of an embolic heart disease, doppler ultrasound of the carotids and echocardiography was done. Lab investigations including coagulation profile (PT, PTT and INR) and thrombophilia workup (protein C and S, factor V Leiden) within normal limits. Serum amino acid analysis, carnitine levels and urine organic acid screen reported normal. She was treated by Aspirin and underwent physical therapy sessions. She showed gradual improvement in her upper and lower limb weakness over several weeks.
Discussion
Stroke is defined by the WHO as a clinical syndrome of rapidly developing neurological deficit related to the perfusion territory of the affected cerebral artery and an evidence of an ischemic lesion on neuro radiological imaging [2]. In children older than 28 days of life; the estimated incidence of ischemic stroke is variable.However,it occurs at an average of 13 per 100,000 for all strokes; of which 7.9/100,000 are of ischemic ones, whereas 5.1/100,000 forhaemorrhagic strokes. 50% of children with ischemic strokes survive with a neurological sequela, hemiparesis being the most common; and about 20% of them die after an ischemic stroke. Recurrence rate has been reported to be 15% at 1 year, possibly reaching up to 41% after 5 years.
It is exceedingly rare, for a pediatric minor head trauma to be complicated by an ischemic stroke, thus exclusion of other systemic causes in such cases is often required. Our case mentioned above, presented with neurological deficit on the subsequent day after a fall from bed [3]. observed a latency of 15 min–16 days for the evolution of basal ganglia lesion following minor head injury.Since there is no supporting clinical or radiological evidence of non-accidentalinjury, it was ruled out [4,5].
In humans, motor learning is controlled by a group of subcortical nuclei termed the basal ganglia; as well as other roles such as executive functions, behaviors, and emotions. Classical lacunar infarcts often lead to pure motor stroke [6]. Damage to the posterior limb of the internal capsule which carriers both sensory and motor nerves can lead to contralateral sensory and motor loss as the case presented in this report.
The basal ganglia and internal capsule are supplied by the lenticulostriate arteries, originating at an acute angle from the larger middle cerebral artery. Having mentioned this, children are more liable to have basal ganglia infarcts then adults provided that these end arteries exhibit more acute angle then former. Therefore, even simple motion of the brain inside the child’s skull could cause disruption of theend arteries, subsequently leading to thrombosis or spasm. Similar concerns are assumed by Kieslich et al. With regards to the pathophysiologymany hypotheses have been proposed; one which states that an injury to the middle cerebral artery andthe associated reduction in partial pressure of carbon dioxide due to crying results in narrowing of the blood vessel, thereby decreasing the blood supply and increasing the chances of thrombosis.Focal dissection of such artery is also being said [7].
In our case, MRI of the brain showed an acute infarct involving the right globuspallidus, putamen and part of posterior limb of internal capsule. This explains the clinical features that are seen (Figure 1).
Increasingly emphasized, is the association between viral infections and stroke. For example, varicella zoster infection, could it be possible that this viral infection leads to an increase in the brittleness of the lenticulostriate arteries, which are more likely to cause basal ganglia infarction in the presence of external force. Cytomegalovirus has also been implicated, as it could cause damage to vascular endothelial cells thereby increasing the risk of development of thrombosis or spasm.However, there was no history of recent infection in the case presented.
Hematological causes could also be one of the secondary causes of ischemic stroke in such cases, for example protein C and S deficiency [8]. Protein C deficiency has also been reported in children taking valproate. Not to forget to mention, that iron deficiency anaemia per say have been reported in children with ischemic stroke with no other apparent etiology.Hemoglobin, protein C and S and factor V Leiden yielded normal results in our case. Other causes include sickle cell disease, which is a very common cause of pediatric stroke, occurring in 285 cases per 100,000 affected children [9].
The vulnerability to adverse neurological sequelae after basal ganglia infarcts may be genetically determined, as has been demonstrated in children having mutations in the calcium voltage-gated channel subunit α1 A gene. Basal ganglia mineralization is also a major risk factor for cerebral infarction identified after minor head injury in children [10]. They allow the lenticulostriate arteries to become more vulnerable to develop vasospasm or thrombosis. Further research is needed however to explore the cause of mineralization [11].
In childhood, ischemic stroke is multifactorial.Commonly, emboli due to congenital or acquired heart disease, arterial dissections, meningitis, hemolytic uremic syndrome, homocystinuria, and syndromes like Down’s syndrome and Williams syndrome, all of which have been implicated as possible reasons.
In our case scenario, the child has no dysmorphic features clinically to suggest any underlying syndrome. There were no features of anaemianor investigations suggestive of any organ involvement. Doppler US of the carotids and ECHO were unremarkable. This helped in narrowing the possibility of the cause of infarction, to be traumatic etiology.
The child was managed conservatively, and showed gradual improvement in the neurological symptoms over several weeks; highlighting a good prognosis of such cases.
Many authors mentioned such cases in the literature like Rana et al. who presented 7 cases of ischemic stroke in minor head injury in children [12,13].
Conclusion
Basal ganglia ischemic lesions following minor head trauma is rare in children. After exclusion of other causes with the available lab and radiological workup, one could suggest a confederation among ischemic stroke and head injuries by the above-mentionedmechanisms.Such cases have a good prognosis with complete remission in few weeks to months.
Consent
Verbal informed consent was taken from the parents about writing this case report and publishing it.
References
- Bodensteiner, J. B."Clinical features of vascular thrombosis following varicella." Archives of Pediatrics& Adolescent Medicine 146.1(1992):100.
- Ganesan, V., et al. "Clinical and radiological recurrence after childhood arterial ischemic stroke." Circulation 114. 20 (2006): 2170-2177.
- Kieslich, M. "Minor head injury as cause and Co-factor in the aetiology of stroke in childhood: A report of eight cases." J Neurol Neurosurg Psychiatry 73. 1 (2002):13-16.
- Ganesan, V., et al. "Clinical and radiological recurrence after childhood arterial ischemic stroke." Circulation 114. 20 (2006): 2170-2177.
- Hunter, J. V. New radiographic techniques to evaluate cerebrovascular disorders in children. Semin Pediatr Neurol 7.4 (2000):261-277.
- Giroud, M., et al. (1995). "Cerebrovascular disease in children under 16 years of age in the city of Dijon, France: A study of incidence and clinical features from 1985 to 1993." J Clin Epidemiol 48.11(1995):1343-1348.
- Kirkham, F. J., et al. (2000). "Risk factors for arterial ischemic stroke in children." J. Child Neurol 15.5 (2000):299-307.
- Gruppo, R., et al. "Protein C deficiency related to valproic acid therapy: A possible association with childhood stroke." J Pediatr 137. 5 (2000): 714-718.
- Earley, C. J., et al. "Stroke in children and sickle-cell disease: Baltimore-Washington cooperative young stroke study." Neurology 51.1 (1998): 169-176.
- Kors, E. E., et al. "Delayed cerebral edema and fatal coma after minor head trauma: Role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine." Ann Neurol 49. 6 (2001): 753-760.
- Lingappa, L., et al. "Mineralizing angiopathy with infantile basal ganglia stroke after minor trauma units." Dev Med Child Neurol, 56. 1 (2013): 78-84.
- Shaffer, L. (2003). "Can mild head injury cause ischaemic stroke?" Arch Dis Child 88. 3 (2003): 267-269.
- Stoodley, N. "RCPCH clinical guideline, stroke in childhood: An evidence-based guideline for diagnosis, management, and rehabilitation." The Lavenham Press (2004).