Research - International Journal of Medical Research & Health Sciences ( 2024) Volume 13, Issue 3
Asymmetrical Septal Hypertrophy: A rare case of respiratory distress in an Infant of a Diabetic Mother
Syed Adnan Ali*, C.V.S. Lakshmi and U. Narayan ReddySyed Adnan Ali, Department of Pediatrics, Deccan College of Medical Sciences (DCMS)-Princess Esra Hospital, Hyderabad, India, Email: syedadnan25@gmail.com
Received: 08-Jan-2022, Manuscript No. ijmrhs-22-51808 (M); Accepted Date: Jan 24, 2022 ; Editor assigned: 10-Jan-2022, Pre QC No. ijmrhs-22-51808 (P); Reviewed: 16-Jan-2022, QC No. ijmrhs-22-51808 (Q); Revised: 23-Mar-2022, Manuscript No. ijmrhs-22-51808 (R); Published: 29-Jan-2022
Abstract
Introduction: Cardiomyopathy is a disease that affects the myocardium and causes mechanical or electric dysfunction. Hypertrophic cardiomyopathy comprises of various cardiac components such as thickening of ventricular walls, hypertrophy of inter-ventricular septum thereby resulting in sub-aortic stenosis, systolic and/or diastolic dysfunction. This cardiac complication is a known but rare entity in infants of diabetic mothers wherein the clinical presentation ranges from being asymptomatic to respiratory distress to congestive cardiac failure. Incidence of Congenital Heart Disease in infants of Diabetic Mothers is 5% and the percentage of symptomatic HOCM babies is 12%. Case Report: We report a term neonate, born to a G2P2L2 mother with Gestational Diabetes Mellitus with poor glycemic control, presenting with respiratory distress manifesting as silent tachypnea at 24 hours of life, diagnosed as Asymmetrical Septal Hypertrophy on 2D-Echo, treated successfully with Propranolol and showed resolution of hypertrophy in follow-up echocardiography. Conclusion: The Fetal Hyperinsulinemia is responsible for increase in synthesis and deposition of fat and glycogen in the myocardial cells which explains the cardiac hypertrophy. Due to increase in the thickness of the Interventricular Septum, there is Left Ventricular Hypertrophy and during systole, the systolic anterior motion of the anterior leaflet (SAM) of the aortic valve is elongated. Therefore, due to this obstruction of the orifice by the Aortic Valve, there is reversal of blood flow clinically manifesting as Silent Tachypnea. Symptomatic babies are treated with Oral Propranolol which act by improving left ventricular outflow obstruction.
Keywords
Aortic valve, Blood flow, Tachypnea
Abbreviations
GDM: Gestational Diabetes Mellitus, TTNB: Transient Tachypnea of New Born, RDS: Respiratory Distress Syndrome, HOCM: Hypertrophic Obstructive Cardiomyopathy, ASD: Atrial Septal Defect, VSD: Ventricular Septal Defect, TGA: Transposition of Great Arteries, PDA: Patent Ductus Arteriosus, LVOT: Left Ventricular Outflow Tract, IDM: Infants of Diabetic Mothers, LSCS: Lower Segment Caesarean Section, PROM: Premature Rupture Of Membranes, NICU: Neonatal Intensive Care Unit, CBP: Complete Blood Picture, CRP: C-Reactive Protein, CXR: Chest X-Ray, SAM: Systolic Anterior Motion, CHD: Congenital Heart Disease
Introduction
Cardiomyopathy is a disease that affects the myocardium and causes mechanical or electric dysfunction.
Hypertrophic cardiomyopathy comprises various cardiac components such as thickening of ventricular walls, hypertrophy of interventricular septum thereby resulting in sub-aortic stenosis, systolic and/or diastolic dysfunction.
We report a neonate that was diagnosed as a case of asymmetrical septal hypertrophy born to a mother with Gestational Diabetes Mellitus (GDM) with poor glycemic control, presenting with respiratory distress, treated successfully with oral Propranolol and showed resolution of hypertrophy in follow-up transthoracic 2-D echocardiography.
GDM is a frequent complication seen in pregnancy with the incidence in the increasing trend recorded in developing countries. Diabetes in pregnancy results in an increased risk of fetal, neonatal, and long-term complications in the new born (listed below):
• Congenital-Neural tube defects, Intestinal anomalies, Cleft palate, Skeletal Malformations, Flexion Contractures
• Respiratory-Organogenesis, Transient Tachypnea of New Born (TTNB), Respiratory Distress Syndrome (RDS), Pneumothorax
• Cardiac-Organogenesis, Hypertrophic Obstructive Cardiomyopathy (HOCM), Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD), Transposition of Great Arteries (TGA), Patent Ductus Arteriosus (PDA)
• Metabolic-Hypoglycemia, Hypocalcemia, Hypomagnesaemia
• Others- Hyperbilirubinemia, Polycythemia, Macrosomia, Prematurity [1,2]
The incidence of congenital heart disease in normal new borns is 0.8% whereas, in Infants of Diabetic Mothers (IDM), it is as high as 5%. The incidence of Asymptomatic HOCM is 36% while the percentage of symptomatic babies is 12% [3].
When routinely searched for with an echocardiographic scan, HOCM is found in 30% of IDM, while symptomatic HOCM occurs in 12.1% [4]. The left ventricular mass and contractility are increased and there is Left Ventricular Outflow Tract (LVOT) obstruction with apposition of the anterior leaflet of the mitral valve to the inter-ventricular septum during systole. Cardiac output is significantly reduced, secondary to reduced stroke volume, and is directly related to the degree of septal hypertrophy [5].
This asymmetric septal enlargement, with a disproportionally hypertrophic septum, is an anabolic result of fetal hyperinsulinemia triggered by maternal hyperglycemia during the third trimester. Cardiac septum hypertrophy correlates with maternal glycosylated hemoglobin levels and high levels of fetal insulin better than with macrosomia.
The severity of IDM cardiomyopathy can vary from an incidental finding on echocardiography (30% of cases) to an infant with severe symptoms of congestive heart failure (12% of cases) [6].
Case Description
A term (39-weeks period of gestation) male baby, with a birth weight of 3.97 kg was born to a 26-year-old G2P2L2 mother via. Lower Segment Caesarean Section (LSCS) given Premature Rupture of Membranes (PROM). The baby had a successful transition from intrauterine to extrauterine life with APGAR scores of 8/9 at 1/5 minutes respectively. The mother was diagnosed with GDM in the 28th week, was on subcutaneous Insulin treatment but maintaining poor glycemic control. There was no other significant antenatal history with all routine scans revealing no abnormalities. The baby was monitored for sugars and respiratory distress and in the normalcy of both, was shifted to the mother’s side after 2 hours of observation in the Neonatal Intensive Care Unit (NICU).
Physical examination of the baby showed a macrosomic infant (weight>90% percentile for age), thick skin folds, broad shoulders, and a plethoric look. No other obvious malformations were noted.
At 24 hours of life, the baby was brought to the NICU with complaints of poor feeding, and an increased work of breathing. On examination, there was only tachypnea with a respiratory rate of 82/min and no other significant findings. Provisionals of TTNB, Aspiration Pneumonia, Sepsis, and Congenital Heart Disease were kept in mind and the baby started on oxygen support via. nasal prongs at 1 L/min thereafter maintaining saturations >93%.
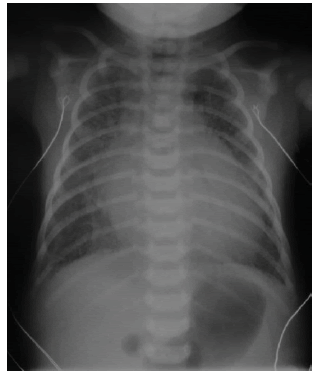
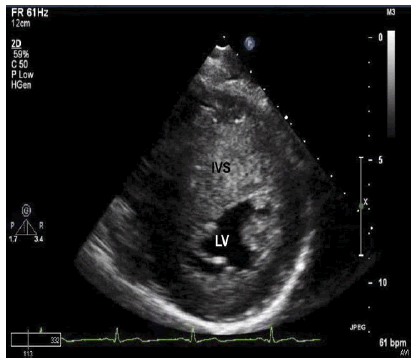
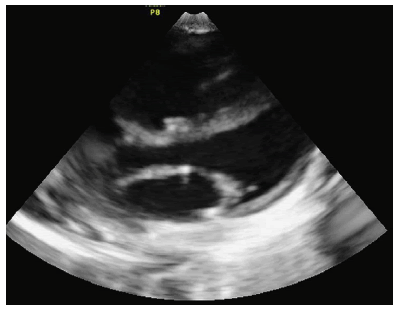
The baby was investigated with a sepsis screen of Complete Blood Picture (CBP), C-Reactive Protein (CRP) and Blood Culture/Sensitivity, Chest X-Ray (CXR), and Serum Calcium, which was in the favour of sepsis (CRP=29.53, White Blood Cells=25,000), Hypocalcemia (7.2 mg%), CXR was done which showed cardiomegaly (cardiothoracic ratio of 0.8) and plethoric lung fields. The baby was started on antibiotics for sepsis control, calcium supplementation initiated, and 2-Dimensional Transthoracic Cardiac Echocardiography was scheduled to investigate the cause of cardiomegaly. The echocardiography was suggestive of marked Inter Ventricular Septal Hypertrophy with a significant reduction in the volume of the ventricular cavity i.e., features pointing towards Asymmetrical Septal Hypertrophy under HOCM (Figures 1-3).
The baby was started on Oral Propranolol at 2 mg/kg/day 12th hourly with regular monitoring of sugar, heart rate, and blood pressure. Distress gradually subsided over the next 24 hours-36 hours. Over the next 2 days, the baby was weaned off oxygen support, oral feeds initiated and monitored for 2 more days, and discharged on Oral Propranolol. Follow-up was scheduled at 2 weeks of age at the time of which tapering of the dose was started and eventually stopped at 4 weeks of age.
The repeat transthoracic echocardiography done at 6 months of age showed resolution of hypertrophy.
Discussion
The diagnosis of sepsis would explain the distress but not the cardiomegaly. There were no associated signs of rales, cyanosis, and hepatomegaly to give Congenital Heart Disease (CHD) as the diagnosis leaving the only significant symptom the baby presented with, the silent tachypnea, wherein the level of tachypnea does not match the severity of the retractions which in this baby’s case, was completely absent.
Gestational Diabetes Mellitus is defined as carbohydrate intolerance of variable severity first diagnosed in pregnancy. Complications of late-onset GDM include Somatohypertrophy, Metabolic, Hyperbilirubinemia, Polycythemia, Macrosomia, and Birth Trauma [1].
The mechanism of Fetal Hypoglycemia is explained by the Pederson Maternal Hyperglycemia-Fetal Hyperinsulinemia Hypothesis which states: Maternal Hyperglycemia leads to Fetal Hyperglycemia which in turn causes Fetal Hyperinsulinemia resulting in Fetal Hypoglycemia. Fetal Hyperinsulinemia is responsible for an increase in synthesis and deposition of fat and glycogen in the myocardial cells which explains cardiac hypertrophy [7,8].
Due to an increase in the thickness of the Interventricular Septum, (>1.3 times the normal thickness is significant) there is Left Ventricular Hypertrophy and during systole, the Systolic Anterior Motion of the anterior leaflet (SAM) of the Aortic Valve is elongated. Therefore, due to this obstruction of the orifice by the Aortic Valve, there is a reversal of blood flow clinically manifesting as silent tachypnea [9,10].
Inotropic agents like dopamine and dobutamine are contraindicated as they end up reducing the ventricular size and thereby contribute to obstruction of cardiac outflow. Beta-Blockers cause a reduction in maximal contraction velocity leading to change in Systolic Anterior Motion and thereby improving left ventricular outflow obstruction [11].
Studies similar to ours, Codazzi, AC, et al., observed similar results with the use of Propranolol in two babies born to diabetic mothers and so did the study of Sharma D, et al., who also documented resolution of septal hypertrophy by 6 months with the use of Propranolol [12,13].
Conclusion
Uncontrolled diabetes mellitus in mothers has proven to have detrimental side effects for the newborn making them a high-risk infant. Smooth, uneventful transition to extra-uterine life, close monitoring in the immediate post-natal period, early diagnosis of underlying abnormality, and periodic screening and follow-ups for associated congenital anomalies ensure that these babies are well taken care of. Beta-Blockers must be started for symptomatic babies like this one but strictly monitored for side effects like bradycardia and hypoglycemia. Septal Hypertrophy is one of the rarest manifestations of HOCM with Incidence of Congenital Heart Disease in normal newborns at 0.8% whereas in Infants of Diabetic Mothers, it is as high as 5%, marked Inter Ventricular Septal Hypertrophy with a significant reduction in the volume of the ventricular cavity. The baby was started on Oral Propranolol at 2 mg/kg/day 12th hourly with regular monitoring of sugar, heart rate, and blood pressure. Distress gradually subsided over the next 24-36 hours. Follow-up was scheduled at 2 weeks of age at the time of which tapering of the dose was started and eventually stopped at 4 weeks of age. The repeat Echo done at 6 months of age showed resolution of hypertrophy.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Buchanan, MD, Thomas A., and John L. Kitzmiller, MD. "Metabolic interactions of diabetes and pregnancy." Annual Review of Medicine, Vol. 45, No. 1, 1994, pp. 245-60.
- Russell, Noirin E., et al. "Cardiomyopathy and cardiomegaly in stillborn infants of diabetic mothers." Pediatric and Developmental Pathology, Vol. 11, No. 1, 2008, pp. 10-14.
- Correa, Adolfo, et al. "Diabetes mellitus and birth defects." American Journal of Obstetrics and Gynecology, Vol. 199, No. 3, 2008, pp. 237e1-e9.
- Vural, M., et al. "Should an echocardiographic scan be done routinely for infants of diabetic mothers?" The Turkish Journal of Pediatrics, Vol. 37, No. 4, 1995, pp. 351-56.
Google Scholar Crossref
- Walther, Frans J., et al. "Cardiac output in infants of insulin-dependent diabetic mothers." The Journal of Pediatrics, Vol. 107, No. 1, 1985, pp. 109-14.
- Reller, Mark D., and Samuel Kaplan. "Hypertrophic cardiomyopathy in infants of diabetic mothers: An update." American Journal of Perinatology, Vol. 5, No. 04, 1988, pp. 353-58.
- Mace, Sharon, et al. "Echocardiographic abnormalities in infants of diabetic mothers." The Journal of Pediatrics, Vol. 95, No. 6, 1979, pp, 1013-19.
- Colucci, Wilson S., and E. Braunwald. "Heart disease. A textbook of cardiovascular medicine." WB Saunders Company, Philadelphia, 1997, pp. 394-420.
Google Scholar Crossref
- Ullmo, Sandra, et al. "Pathologic ventricular hypertrophy in the offspring of diabetic mothers: A retrospective study." European Heart Journal, Vol. 28, No. 11, 2007, pp. 1319-25.
- Akcoral, A. D. N. A. N., et al. "Transient right sided hypertrophic cardiomyopathy in an infant born to a diabetic mother." The Indian Journal of Pediatrics, Vol. 63, No. 5, 1996, pp. 700-03.
- Denfield, S. W., R. J. Gajarski, and J. A. Towbin. "Cardiomyopathies." The science and practice of pediatric cardiology. Second edition. Baltimore: Williams and Wilkins, 1998, pp. 1851-84.
Google Scholar Crossref
- Codazzi, Alessia Claudia, et al. "Hypertrophic cardiomyopathy in infant newborns of diabetic mother: A heterogeneous condition, the importance of anamnesis, physical examination and follow-up." Italian Journal of Pediatrics, Vol. 47, No. 1, 2021, pp. 1-6.
- Sharma, Deepak, et al. "Asymmetrical septal hypertrophy and hypertrophic cardiomyopathy in infant of diabetic mother: A reversible cardiomyopathy." Medical Journal of Dr. DY Patil University, Vol. 9, No. 2, 2016, pp. 257-60.