Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
Association of Indices of Glucose Metabolism with Diabetic Foot Ulcers Nothing Sweet about This: Observations from a Hospital-Based Cross- Sectional Study
Rachita Nanda*, Seema Shah, Suprava Patel and Eli MohapatraRachita Nanda, Department of Biochemistry, AIIMS Raipur, India, Email: dr.rachitananda@gmail.com
Received: 30-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Background and Aims: With a lifetime incidence of diabetic foot ulcers as high a 25% for diabetics, early detection of these ulcers is utmost to reduce the morbidity, mortality, and economic burden associated with it. Although the role of glycaemic control in wound healing has been studied, there is limited information on indices of glucose metabolism in predisposing diabetics towards foot ulcers. This study aimed to evaluate the association of Fasting Plasma Glucose (FPG), Postprandial Plasma Glucose (PPPG), HbA1C, and Body Mass Index (BMI) with diabetic foot ulcers. Methods: This is a hospital-based observational study where patients with diabetic foot ulcers were recruited. The diabetic ulcers gradation was according to Wagner’s classification, followed by the collection of detailed demographic, clinical and biochemical. Data were presented as frequency and percentage, mean ± SD, median and interquartile range. Comparison between different ulcer grades was performed with ANOVA and posthoc tests. Results: A total of 93 patients were recruited, with 76% males in the age group of 55.6 ± 9.44. With a median duration of diabetes being eight years, most ulcers (>90%) were in grades 2, 3, and 4. The FPG and PPPG were higher than that recommended by Diabetes standards of care. Although mean BMI was normal, HbA1C was significantly associated with the ulcer grade (p=0.01). Conclusions: HbA1C is a better indicator of the severity of ulcers than FPG, PPPG, and BMI. Regular monitoring of glycaemic status through HbA1C would give a better idea of glycaemic control and regulate the development of microvascular complications.
Keywords
BMI, Fasting plasma glucose, HbA1C, Microvascular complications, Postprandial plasma glucose
Introduction
The prevalence of Diabetic Foot Ulcers (DFU) in India is varied, ranging from 5.3% in central India to 13.6% in Northern India [1]. To contain the considerable cost and challenge, detection and effective management of foot ulcers at early stages are essential.
The mechanism and management of wound healing in DFU are still not satisfactory [2]. An association with wound healing and the lower limb’s amputation has been observed, considering that hyperglycemia impairs wound healing through various mechanisms [3,4]. Hyperglycaemia impairs growth factor signaling and recruitment of fibroblasts to the wound site and delays the healing of the wound [5,6]. The role of glycaemic control in preventing the development of DFU is not clear. Therefore, we hypothesize that blood glucose management is also one of the criteria for developing ulcers.
In this study, we chose to evaluate the clinical profile of DFU and the association of various indices of glucose metabolism like Body Mass Index (BMI), Fasting Plasma Glucose (FPG), Postprandial Plasma Glucose (PPPG), and glycosylated hemoglobin (HbA1C) with the grade of DFU.
Materials and Methods
This observational study was conducted at a tertiary care teaching hospital where 93 patients with diabetic foot ulcers were recruited consecutively over 18 months. Institutional ethics committee approval was obtained before the initiation of the project. Written informed consent was obtained from all participants enrolled in the study. Diabetic foot ulcer was defined as ulceration, infection, or destruction of deep tissues located in the lower limb below the ankle [7]. The severity of the foot ulcers was categorized according to Wagner’s Classification system [8]. Patients with bilateral feet ulcers have not been included in the study.
Demographic and other clinical data like duration of diabetes, insulin and oral hypoglycaemic drug therapy, smoking history, and family history of diabetes were recorded. Weight and height were used to calculate the BMI (Kg/m2). Using the laboratory information system, all biochemical parameters like FPG, PPPG, HbA1C, renal function tests, and lipid profile were collected. Glucose estimation was done by glucose oxidase peroxidase method, HbA1C by HPLC (High-Performance Liquid Chromatography), urea by urease UV, and creatinine by modified Jaffe’s method. The total cholesterol, triglycerides, and High-Density Lipoprotein (HDL) were estimated by the cholesterol oxidase peroxidase method, glycerol phosphate oxidase, and direct estimation, respectively. Friedwald’s equation calculated Low-Density Lipoprotein (LDL).
Statistical Analysis
Data were analyzed using IBM SPSS 20.0 Version. Qualitative data were presented as n (%), quantitative data normally distributed and not normally distributed were as mean ± SD and median (interquartile range) respectively. Analysis of Variance (ANOVA) has been used for testing the difference between more than two means. A p-value of 0.05 was considered to be significant.
Results
Table 1 shows the mean age of the participants was 55.6 ± 9.44 years, with 56.9% of subjects above the age group more than 50 years. There was a male predominance (76.3%) of patients who visited the hospital. Unskilled workers accounted for 31.1% of the study population, retired 23.6%, skilled 18.2 and homemakers, and currently unemployed at 18.2% and 15%. The 93 participants having foot ulcers had a median duration of diabetes of 8 years (IQR 4, 14), with five having a time of diabetes more than 20 years. Almost half (45.1%) of the participants had a family history of diabetes mellitus. Around 42% were on insulin therapy, with 71 participants on oral hypoglycaemic agents combined with or without insulin therapy. Only 18.2% were smokers in the past, with 31.1% continuing smoking even after developing an ulcer. The mean BMI was normal, with systolic blood pressure in the higher range than diastolic blood pressure.
| Characteristics | Value |
|---|---|
| Median age | 55.6 ± 9.44 |
| Gender(M/F) | 71/22 (76.3, 23.7) |
| Occupation | |
| Skilled | 17 (18.2) |
| Unskilled | 29 (31.1) |
| Unemployed | 11 (11.8) |
| Retired | 22 (23.6) |
| Housewife | 14 (15.0) |
| Mean duration of diabetes (years)* | 8.0 (4,14) |
| Family history of diabetes | 42 (45.1) |
| On insulin therapy, n (%) | 39 (41.9) |
| Active smoking, n (%) | 29 (31.1) |
| Past smokers | 17 (18.2) |
| BMI (Kg/m2) | 23.23 ± 3.63 |
| Systolic Blood Pressure (mmHg) | 130.96 ± 13.39 |
| Diastolic Blood Pressure (mmHg) | 81.37 ± 9.6 |
| Data expressed in mean ± SD, n (%), *median (IQR) | |
As depicted in Table 2, the most predominant co-morbidity was neuropathy (43%), followed by a similar prevalence of dyslipidemia and retinopathy (35.4% and 32.2%). Hypertension was observed in 29% of participants, with none having nephropathy. According to Wagners classification of ulcer grading, grade 4 was the most common ulcer (43%), followed by grade 3 (30.1%) and grade 2 (20.4%). Both grade 1 and grade 5 were three each in number. The sole (47.3%) was the most typical site, followed by toes and then the heel (37.6% and 15%, respectively).
| Variables | N (%) |
|---|---|
| Hypertension | 27 (29) |
| Dyslipidaemia | 33 (35.4) |
| Neuropathy | 40 (43) |
| Nephropathy | 0 (0) |
| Retinopathy | 30 (32.2) |
| Ulcer grade | |
| 0 | 0 (0) |
| 1 | 3 (3.2) |
| 2 | 19 (20.4) |
| 3 | 28 (30.1) |
| 4 | 40 (43.0) |
| 5 | 3 (3.2) |
| Location of ulcer | |
| Sole | 44 (47.3) |
| Toes | 35 (37.6) |
| Heel | 14 (15.0) |
The glycemic profile of diabetic foot ulcers patients is much higher than that recommended as per glycemic targets: Standards of medical care in diabetes- 2020 by the American Diabetes Association [9]. The FPG, PPPG, HbA1C were 187.74 ± 61.3 mg/dL, 263.75 ± 77.12 mg/dL and 10.1 ± 2.0% respectively (Table 3).
| Lab Parameters | Mean ± SD |
|---|---|
| Fasting plasma glucose (mg/dL) | 187.74 ± 61.3 |
| Post prandial plasma glucose (mg/dL) | 263.75 ± 77.12 |
| HbA1C (%) | 10.1 ± 2.01 |
The glycemic indices of the three standard grades of ulcers were matched to identify which was associated with diabetic foot (Table 4). In comparison, it is revealed that there was a significant change in HbA1C level (p=0.01), with the difference being significant between grade 2 and grade 4 diabetic foot ulcer patients (p=0.023). However, the FPG, PPPG, and BMI were comparable in the three ulcer grades.
| Ulcer grade | FPG (mg/dL) | p-value | PPPG (mg/dL) | p-value | HbA1C (%) | p-value | BMI (Kg/m2) | p-value |
|---|---|---|---|---|---|---|---|---|
| Grade 2 (n=19) | 191.36 ± 43.48 | 0.86 | 267.47 ± 49.62 | 0.99 | 9.27 ± 1.84 | 0.01 | 23.07 ± 3.96 | 0.06 |
| Grade3 (n=28) | 189.5 ± 69.02 | 264.67 ± 75.87 | 9.73 ± 2.06 | 21.9 ± 3.66 | ||||
| Grade 4 (n=40) | 182.92 ± 63.1 | 264.8 ± 93.16 | 10.79 ± 1.99 | 24.12 ± 3.59 | ||||
| *ANOVA and (Bonferroni test) HbA1C; Grade2 vs. Grade 4 ; p=0.023 | ||||||||
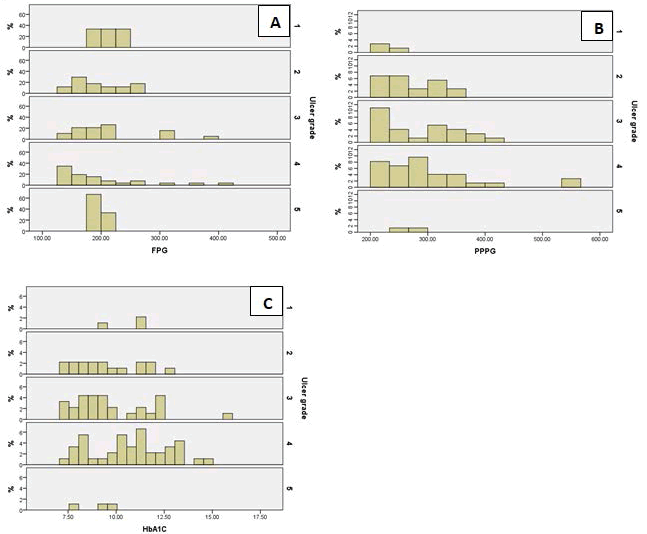
Figure 1 depicts the histogram plots of participants with FPG ≥ 126 mg/dL, PPPG ≥ 200 mg/dL, HbA1C ≥ 7%. The majority of the ulcers were when FPG was within 150 mg/dL-250 mg/dL, PPPG within 200 mg/dL-400 mg/dL, and HbA1c from just below 7.5 to just above 12.5.
Discussion
A diabetic foot ulcer complications one out of four people with diabetes will develop in their lifetime [4]. Furthermore, non-healing ulcers are an important cause of amputation of the lower limb. A variety of risk factors associated with delayed ulcer healing is dysglycemia and other pathological states due to the metabolic disorder.
Our study revealed that many patients who come to the hospital were beyond the middle age group and were males. A similarity was to the work was found by other researchers as middle age is the stage people were more likely to have worse lifestyle and poor glucose control resulting in microangiopathy as a complication [10,11]. In middle age, these patients have been exposed to diabetes for a mean period of at least eight years. Long-term exposure to high glucose levels impairs each phase of wound healing, like hemostasis, inflammation, proliferation, and remodeling phase. such exposure is also associated with the poor formation of granulation tissue and decline in tensile strength of the wound [12]. A similar percentage of individuals were unskilled or retired individuals or were smokers who have not managed the development of ulcers. Also, smoking has extensive effects on the onset and healing of diabetic ulcers by weakening immune-mediated healing responses and augmenting microvascular damage [13]. Since around 41% were on insulin therapy, it indicates that these individuals had diabetes for a pretty long time as insulin is generally the later mode of treatment after failure of oral hypoglycaemic drugs.
The mean BMI was normal in these patients, although there has been a disagreement between BMI and foot ulceration risk in people with diabetes. Vibha, et al. have mentioned no association between BMI and foot ulceration, whereas Sohn, et al. have suggested a significant J-shaped association between BMI and diabetic foot [10,14]. Almost one-third of patients had hypertension, dyslipidemia, and retinopathy, whereas 43% as neuropathy, with no case of nephropathy.
The FPG, PPPG, and HbA1C in these patients are not, as per ADA, glycemic targets in the standards of medical care in diabetes, with the mean value of all the three parameters being elevated. The target preprandial capillary plasma glucose is 80 mg/dL-130 mg/dL, peak postprandial capillary plasma glucose <180 mg/dL, and HbA1C maintained at <7.0% [9]. Comparison of glycaemic indices (FPG, PPPG, HbA1C, and BMI) across the three standard grades of ulcers revealed only HbA1C to be significantly associated. The HbA1C values between grade 2 and grade 4 ulcers were quite different (p=0.023).
Evidence of HbA1C as a biomarker in predicting wound healing has been suggested by some researchers while in specific other papers, there is no association [15-17]. HbA1C testing reflects glycemia over three months. Although HbA1C is affected by different factors like anemia or advanced kidney disease, none existed in our patient population. Hence the association of HbA1c with the grade of ulcer must be taken into consideration. A plasma glucose level of an individual has a very high variance than HbA1C. Although postprandial glucose level has more contribution than preprandial glucose level towards HbA1C level at the cut-off grade of 7%, studies have shown HbA1C to be a predictor of complications of diabetes [9]. As evident in the histogram plots, the range of FPG and PPPG is quite broad, to dangerously high levels even beyond 400 mg/dL. These peaks were identified at postprandial and preprandial states, but the peak value attained by glucose must have been far higher. The measurement of HbA1C can only monitor these high values. The authors also suggest that all people with diabetes should be monitored for an average HbA1C, given that the individuals who develop diabetic foot ulcers have a longer duration of diabetes.
Although HbA1C is an indirect measure of average glycemia, with certain limitations like unavailability of testing facility and variability in test measurement, clinicians should exercise judgment of glycaemic control solely on HbA1C, especially if the result is close to the threshold. Achieving the HbA1C target goal of <7% early in the course of the disease would reduce microvascular complications like diabetic foot ulcers and prevent the most dreaded lower limb amputation.
Although observational with small sample size, this study can provide the guide for prospective longitudinal studies before developing ulcers through diabetes registries, which can keep track of all various parameters to observe the role of glycemic indices on ulcer development and outcome.
Conclusion
Hyperglycaemia in people with diabetes is the culprit of poor healing of wounds in those with ulcers. Long-term high blood glucose identified by HbA1C, if made to achieve a target goal of around 7%, may reduce complications like diabetic foot ulcers. Hence reasonable control of blood glucose early at the onset of diabetes is the goal for improved healing rate.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Seth, Abhinav, et al. "Clinical profile and outcome in patients of diabetic foot infection." International Journal of Applied and Basic Medical Research, Vol. 9, No. 1, 2019, pp. 14-19.
- Xiang, Jiali, et al. "Reasonable glycemic control would help wound healing during the treatment of diabetic foot ulcers." Diabetes Therapy, Vol. 10, No. 1, 2019, pp. 95-105.
- Baltzis, Dimitrios, Ioanna Eleftheriadou, and Aristidis Veves. "Pathogenesis and treatment of impaired wound healing in diabetes mellitus: New insights." Advances in Therapy, Vol. 31, No. 8, 2014, pp. 817-36.
- Hingorani, Anil, et al. "The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine." Journal of Vascular Surgery, Vol. 63, No. 2, 2016, pp. 3S-21S.
- Peppa, Melpomeni, Panagiotis Stavroulakis, and Sotirios A. Raptis. "Advanced glycoxidation products and impaired diabetic wound healing." Wound Repair and Regeneration, Vol. 17, No. 4, 2009, pp. 461-72.
- Falanga, Vincent. "Wound healing and its impairment in the diabetic foot." The Lancet, Vol. 366, No. 9498, 2005, pp. 1736-43.
- IWGDF Guidelines. "IWGDF definitions and criteria." 2019. https://iwgdfguidelines.org/wp-content/uploads/2019/05/definitions-and-criteria-final.pdf
- Oyibo, Samson O., et al. "A comparison of two diabetic foot ulcer classification systems: The Wagner and the University of Texas wound classification systems." Diabetes Care, Vol. 24, No. 1, 2001, pp. 84-88.
- American Diabetes Association. "6. Glycemic targets: Standards of medical care in diabetes-2020." Diabetes Care, Vol. 43, No. Supplement 1, 2020, pp. S66-S76.
- Vibha, S. P., et al. "Community based study to assess the prevalence of diabetic foot syndrome and associated risk factors among people with diabetes mellitus." BMC Endocrine Disorders, Vol. 18, No. 1, 2018, pp. 1-9.
- Tong, Tao, et al. "Phenotypes and outcomes in middle-aged patients with diabetic foot ulcers: A retrospective cohort study." Journal of Foot and Ankle Research, Vol. 13, 2020, pp. 1-8.
- Patel, Satish, et al. "Mechanistic insight into diabetic wounds: Pathogenesis, molecular targets and treatment strategies to pace wound healing." Biomedicine & Pharmacotherapy, Vol. 112, 2019, p. 108615.
- Xia, Nan, et al. "Review of the role of cigarette smoking in diabetic foot." Journal of Diabetes Investigation, Vol. 10, No. 2, 2019, pp. 202-15.
- Sohn, Min‐Woong, et al. "Significant J‐shaped association between Body Mass Index (BMI) and diabetic foot ulcers." Diabetes/Metabolism Research and Reviews, Vol. 27, No. 4, 2011, pp. 402-09.
- Christman, Andrea L., et al. "Hemoglobin A1c predicts healing rate in diabetic wounds." Journal of Investigative Dermatology, Vol. 131, No. 10, 2011, pp. 2121-27.
- Kumar, Brajkishor, et al. "Prospective study to correlate the level of glycosylated haemoglobin with wound healing, vasculopathy and neuropathy in diabetic foot patients." International Surgery Journal, Vol. 3, No. 4, 2016, pp. 2087-91.
- Fesseha, Betiel K., et al. "Association of hemoglobin A1c and wound healing in diabetic foot ulcers." Diabetes Care, Vol. 41, No. 7, 2018, pp. 1478-85.