Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 6
Assessment of Outcome and Feasibility of Bladder Preservation Therapy in Muscle Invasive Bladder Carcinoma: A Prospective Observational Study with Meta-analysis
Ishwar Ram Dhayal, Department of Urology and Renal Transplant, Dr RMLIMS, Lucknow, India, Email: ish23456@gmail.com
Received: 03-Jun-2022, Manuscript No. ijmrhs-22-65840 ; Editor assigned: 06-Jun-2022, Pre QC No. ijmrhs-22-65840 (PQ); Reviewed: 22-Jun-2022, QC No. ijmrhs-22-65840 (Q); Revised: 22-Jun-2022, Manuscript No. ijmrhs-22-65840 (R); Published: 30-Jun-2022
Abstract
Background: Radical Cystectomy (RC) is the standard of care for the management of Muscle Invasive Bladder Cancer (MIBC). Considering perioperative complications coupled with a classically older patient population with multiple comorbidities has led patients and clinicians to seek alternatives to cystectomy like organ-preserving therapies in the management of bladder cancer over the past several decades. Objectives: The primary objectives were to assess the outcome (overall survival, recurrence-free survival) of bladder preservation therapy in patients with muscle invasive bladder carcinoma and to compare the outcome of bladder preservation therapy with the outcome of radical cystectomy in patients with muscle invasive bladder carcinoma. Methods: In a prospective observational setting patients with clinical stage T2-T4aN0M0 (after initial cystoscopic biopsy) carcinoma of the urinary bladder were given a choice between bladder preservation therapy (Only maximal TURBT/Partial cystectomy/Hemicystectomy/ Primary chemotherapy/Primary Radiotherapy/Concurrent Chemo-radiation) and radical cystectomy. The decision to pursue bladder preservation therapy was based on the patient’s choice after a multidisciplinary discussion of treatment options. Primary endpoints were overall survival, recurrence-free survival, disease-specific survival, bladder intact survival, and secondary endpoints considered were-tumor response, treatment compliance, and rate of salvage radical cystectomy, toxicity, and patient-reported quality of life. Results: Out of 116 patients with MIBC enrolled in the study, 31 (26.7%) opted for Radical Cystectomy (RC) while the rest 85 patients (73.3%) opted/considered bladder preservation therapy. The majority (70%) of patients with muscle invasive bladder carcinoma chose or was suitable to undergo bladder preservation therapy and the rest (30%) chose or were suitable to undergo radical cystectomy. In the bladder preservation therapy group, the majority (82.2%) of patients underwent chemo-radiation after TUR biopsy, 4.1% of patients underwent partial cystectomy and 13.7% of patients underwent maximal (radical) TURBT followed by chemo-radiation. Overall survival, recurrence-free survival, disease-specific survival, and bladder intact survival in the bladder preservation therapy group at 22 months follow-up (Median follow-up period-11.97 months) were 80.8%, 56.2%, 84.9%, and 75.3% respectively. Conclusions: Survival of bladder preservation therapy patients was non-inferior to the survival of radical cystectomy patients at 22 months follow-up. Mortality and morbidity of bladder preservation therapy were acceptable.
Keywords
Muscle Invasive Bladder Cancer (MIBC), Bladder preservation therapy, Radical Cystectomy (RC), Combined-Modality Therapy (CMT), Radiation Therapy (RT), Transurethral Resection of Bladder Tumor (TURBT)
Introduction
Radical Cystectomy (RC) has long been the standard of care for the management of Muscle Invasive Bladder Cancer (MIBC). Modern RC series have demonstrated 5-year Overall Survival (OS) rates of 56%-66% [1-4].
The morbidity and mortality of RC are well documented [5]. The high incidence of perioperative complications, coupled with a classically older patient population with multiple medical comorbidities, has led patients and clinicians to seek alternatives to cystectomy. There has been an increasing trend of utilizing organ-preserving therapies in the management of multiple cancers over the past several decades.
“Bladder preservation” as a treatment paradigm includes a range of therapies: partial cystectomy, radical transurethral resection, chemotherapy, and radiation therapy. Combined-Modality Therapy (CMT) incorporating maximal TURBT followed by Radiation Therapy (RT) with concurrent radio-sensitizing chemotherapy can be a comparably effective regimen to preserve a functioning bladder in well-selected patients who are either poor candidates for radical cystectomy or patients who are motivated to maintain their native bladder. This combined-modality approach utilizing TURBT followed by RT with concurrent chemotherapy is often referred to as tri-modality therapy. Modern oncologic therapies are increasingly driven towards organ preservation and maximizing functional outcomes while maintaining treatment efficacy. Emerging data suggest that an approach using a combination of these therapies results in the best oncologic outcomes. In highly selected patients, metastasisâ??free and cancerâ??specific survivals appear to be similar to RC [6,7].
Historical series have demonstrated inferior results with single modality therapy (radical TUR, chemotherapy alone, or radiation alone) compared to that of radical cystectomy. With this in mind, successful bladder preservation should be viewed as a multimodal therapy involving aggressive TUR, systemic chemotherapy, and radiation therapy. Appropriate patient selection is also extremely important to optimize response to bladder-sparing protocols. Each patient should be thoroughly evaluated regarding perioperative risk before undergoing radical cystectomy. Patients who are medically unfit for surgery or who refuse surgery can be considered for bladder preservation. Patients who are deemed “medically fit” to undergo cystectomy should be offered cystectomy as the standard of care; however, bladder preservation is a reasonable option for those who are highly selected and counseled appropriately.
Patients with hydronephrosis, obvious T3 disease on imaging, presence of CIS, multifocal tumors, and/or incomplete macroscopic tumor resection are suboptimal candidates for bladder preservation.
Bladder preservation methods can be either single modality or Multimodal therapy. Single modality treatments can be either radical transurethral resection (maximal TURBT) Partial Cystectomy or chemo-radiation therapy or primary chemotherapy or radiation monotherapy.
Multimodal therapy or tri-modal therapy is the growing concept for bladder preservation protocol. Two basic strategies for tri-modal bladder preservation exist split course and continuous-course therapy. Split-course therapy is based on the premise of mid-treatment restaging. Patients are administered induction chemo-radiation therapy to approximately 40 Gy, which is followed by restaging with cross-sectional imaging and endoscopic evaluation. If the persistent invasive disease is noted, radical cystectomy is recommended. Those without persistent invasive disease undergo consolidative chemo-radiotherapy to approximately 64 Gy.
As the name implies, continuous-course treatment involves a full course of chemo-radiation therapy followed by an endoscopic restaging examination 6 months after therapy to allow time for an adequate response to therapy. Regardless of the approach, maximal tumor debulking before tri-modal therapy is critical to optimize therapeutic results. Following tri-modal therapy, although there is no universally accepted follow-up regimen, close surveillance with cross-sectional imaging and cystoscopy are necessary.
There is no randomized controlled trial evidence directly comparing surgery with bladder preservation. A UK-based multi-center feasibility pilot study, Selective bladder Preservation against Radical Excision (SPARE), attempted to randomize patients with the complete response at cystoscopy following neoadjuvant chemotherapy, between surgery and radiotherapy [8]. However, the trial was closed due to poor accrual. This reminds us of the inherent difficulties in testing surgical versus non-surgical options for the definitive treatment of cancer. Patients often find it hard to accept being randomized between two radically different treatment approaches. The treatment pathway becomes very complex when multiple teams are involved in delivering different components of treatment causing further difficulties in recruiting patients. The closure of this trial suggests that we might never have high-quality evidence directly comparing chemoradiotherapy and radical cystectomy for MIBC. National and international guidelines for bladder cancer management have included bladder preservation as an effective alternative treatment for MIBC. Recently published National Institute of Clinical Excellence (NICE) Guidelines in the UK recommend that patients with MIBC suitable for radical treatment should be offered a choice between radical cystectomy and radio -therapy with a radiosensitizer [9].
No completed randomized studies are comparing RC and bladder preservation therapy, but multiple series have suggested that bladder preservation therapy can yield favorable results in well-selected patients [10-21]. The available data demonstrate long-term outcomes for TMT similar to RC and continue to support and establish the role of bladderpreserving TMT as an appropriate alternative to RC for well-selected patients with MIBC who are motivated to preserve their native bladder. Engaging patients in shared decision-making through multidisciplinary clinics are key to more widespread utilization of this treatment strategy, and it would be reasonable to offer it routinely, as an alternative to RC, to appropriate candidates. Prospective trials are needed to compare the efficacy of bladder preservation therapy to that of radical cystectomy; however, it is worth noting that reported outcomes from bladder preservation therapy series are comparable to those of surgical series.
Objectives
Primary objectives:
• To assess the outcome (overall survival, recurrence-free survival) of bladder preservation therapy in patients with muscle invasive bladder carcinoma.
• To compare the outcome of bladder preservation therapy with the outcome of radical cystectomy in patients with muscle invasive bladder carcinoma.
Secondary objectives:
• To assess side effects and compliance of bladder preservation therapy in patients with muscle invasive bladder carcinoma.
• To assess factors affecting bladder preservation therapy.
Methods
This prospective observational study was carried out from 1st March 2019 to December 2019 after obtaining informed consent from all the patients explaining the nature of the study.
Inclusion Criteria
• Patients with clinical stage T2-T4aN0M0 urothelial carcinoma of urinary bladder-who were also candidates for radical cystectomy.
• Patients who were ideal candidates for partial cystectomy (solitary lesion <5 cm in a region that can be excised with adequate 2 cm margins) or hemicystectomy (in whom at least 50% of the urinary bladder is free of tumor).
• Patients not fit or who refused to undergo radical cystectomy.
Exclusion Criteria
• Patients who refused Bladder preservation protocol and opted for radical cystectomy
• Clinical stage >T4a or >N0 or >M0
• Widespread carcinoma in situ
• Simultaneous upper tract, urethral or prostatic urethral TCC or presence of hydronephrosis-they were counseled for radical cystectomy-they were kept in the bladder preservation group if they did not give consent.
• Moribund patients (ECOG>2)
Methodology
• Patient eligibility and selection: Patients with clinical stage T2-T4aN0M0 (after initial cystoscopic biopsy) carcinoma of the urinary bladder were given a choice between bladder preservation therapy (Only maximal TURBT/Partial cystectomy/Hemicystectomy/Primary chemotherapy/Primary Radiotherapy/ Concurrent Chemoradiation) and radical cystectomy. Chemotherapy was Cisplatin-based (most common was Gemcitabine+Cisplatin). The decision to pursue bladder preservation therapy was based on the patient’s choice after a multidisciplinary discussion of treatment options. Depending upon the patient’s tolerance, compliance, and medical condition, we used bladder preservation therapy in a customized and tailored manner (using single/ multimodality treatment) based on the evidence available in current literature.
• Patients underwent a maximally safe TURBT and then received induction (neoadjuvant) concurrent chemotherapy (except for those who were poor candidates for chemotherapy in whom we did maximum TURBT or partial cystectomy followed by radiotherapy) and radiation therapy (split course of continuous course) or partial cystectomy (ideal candidates are those patients with a solitary lesion (<5 cm) in a region that can be excised with adequate, 2 cm margins) or hemicystectomy (in whom >50% of bladder is free of tumor). Patients undergoing partial cystectomy or hemicystectomy also underwent extensive lymphadenectomy in case of positive lymph nodes followed by any additional treatment if required. In the case of Ureterovesical Junction (UVJ) involvement, crossed ureterostomy or ureteric re-implantation was planned.
• After completion of induction therapy/bladder preservation surgery, patients underwent a treatment response evaluation with a repeat cystoscopy, tumor site rebiopsy/re TURBT, CT scan/MRI scan, and urine cytology. Patients with a Complete Response (CR) to induction therapy were asked to undergo consolidation chemoradiation, whereas those with the residual invasive disease were recommended to undergo immediate salvage radical cystectomy. Patients who took 2 or fewer cycles of chemo-radiation were considered to be lost to follow-up and were excluded and only patients who underwent more than 2 cycles were included in the study.
• Criteria for complete response and follow-up: Complete Response (CR) to chemo-radiation is defined as no visible tumor on cystoscopy or imaging and a negative tumor site re-biopsy. Patients with conserved bladders were followed closely with serial cystoscopy, tumor site re-biopsy, bi-manual Examination Under Anaesthesia (EUA), urine cytology, and imaging of the chest, abdomen, and pelvis (CT/MRI/FDG PET) every 3 monthly. Intravesical therapy will be the preferred treatment for appropriate non-invasive recurrences, while invasive recurrence will be recommended to undergo salvage radical cystectomy.
• Outcome endpoints:
• Primary endpoint:
a. Overall survival
b. Recurrence-free survival
c. Disease specific survival
d. Bladder intact survival
• Secondary endpoints:
a. Tumour response
b. Treatment compliance
c. Rate of salvage radical cystectomy
d. Toxicity
e. Patient-reported quality of life
Statistical Analysis
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 21.0 statistical analysis software. Continuous variables were expressed in Mean ± SD. Categorical variables were expressed as frequency and percentage. Nominal categorical data were compared using the Chi square test or Fischer’s exact test as appropriate. Multivariate analysis was used when multiple factors affected an outcome. Quantitative data were compared using paired t-test. For all statistical purposes, the confidence interval was set at 95% and a p-value<0.05 was considered significant.
Time-to-event endpoints were assessed using Kaplan-Meier methods. Comparisons were made using the log-rank test. Univariate Cox proportional hazard regression analysis was used to evaluate the effect of individual variables on the described survival endpoint. Multivariate cox proportional hazard regression analysis was performed using continuous variables or categorical variable cut points. The covariates considered were: age (continuous variable), sex (male vs. female), clinical T stage (T2 vs. T3/4a), TURBT (complete vs. incomplete), hydronephrosis (absence vs. presence), response to chemoradiation (complete vs. incomplete), concurrent chemotherapy regimen, neoadjuvant chemotherapy (yes vs. no), year of diagnosis (continuous variable), and cystectomy (time-varying covariate; any vs. none; immediate vs. delayed). Unadjusted and adjusted hazard ratios were calculated for each covariate using a stepwise Cox proportional hazards regression analysis.
The values were represented in Number (%) and Mean ± SD.
Results
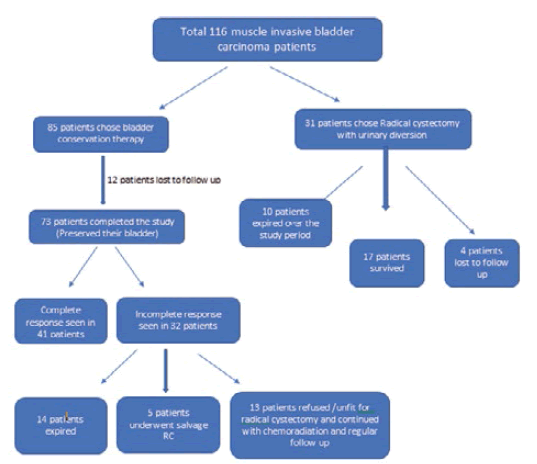
A total of 116 consecutive patients with Muscle Invasive Bladder Carcinoma (MIBC) who came to our center were enrolled in the study according to the inclusion criteria. Out of 116 patients with MIBC enrolled in the study, 31 (26.7%) opted for Radical Cystectomy (RC) while the rest 85 patients (73.3%) opted/considered bladder preservation therapy (Figure 1).
The profile of these 73 patients of MIBC who opted for bladder preservation therapy is given in following Table 1.
| SN | Characteristics | No. | % |
|---|---|---|---|
| 1 | Mean Age ± SD (Range) | 56.08 ± 12.49 (18-78) | |
| 2 | Gender | ||
| Male | 59 | 80.8 | |
| Female | 14 | 19.2 | |
| 3 | Coexisting Disease | ||
| Absent | 54 | 74 | |
| Present | 19 | 26 | |
| 4 | Mean Tumor size ± SD (Range) | 3.91 ± 0.98 (2.5-6.5) | |
| 5 | Clinical T Stage | ||
| T2 | 23 | 31.5 | |
| T3a | 10 | 13.7 | |
| T3b | 24 | 32.9 | |
| T4a | 16 | 21.9 | |
| 6 | Neoadjuvant chemotherapy | ||
| Yes | 4 | 5.5 | |
| No | 69 | 94.5 | |
| 7 | Hydronephrosis | ||
| Absent | 51 | 69.9 | |
| Present (Unilateral) | 14 | 19.2 | |
| Present (Bilateral) | 8 | 11 | |
| 8 | TURBT | ||
| Not done | 2 | 2.7 | |
| Incomplete | 33 | 45.2 | |
| Complete | 38 | 52.1 | |
| 9 | Response to chemo-radiation | ||
| Not given | 3 | 4.1 | |
| Incomplete | 27 | 37 | |
| Complete | 43 | 58.9 | |
| 10 | ECOG Score | ||
| 0 | 23 | 31.5 | |
| 1 | 39 | 53.4 | |
| 2 | 11 | 15.1 | |
| 11 | Median follow up duration ± SD (Range) | 13.21 ± 9.79 (3-64) | |
| 12 | Histopathological Findings | ||
| TCC | 70 | 95.9 | |
| Adenocarcinoma | 2 | 2.7 | |
| Leiomyosarcoma | 1 | 1.4 | |
| 13 | Intervention | ||
| TUR biopsy followed by chemoradiation | 60 | 82.2 | |
| Partial cystectomya | 3 | 4.1 | |
| Maximal TURBT followed by chemoradiation | 10 | 13.7 | |
| 14 | Response to Intervention | ||
| Complete | 41 | 56.2 | |
| Incomplete | 32 | 43.8 | |
| (a) Chemoradiation continued | 13 | 17.8 | |
| (b) Salvage radical cystectomy | 5 | 6.8 | |
| (c) Expired | 14 | 19.2 | |
| 15 | Follow up modality | ||
| Check cystoscopy | 32 | 43.8 | |
| CECT KUB | 5 | 6.8 | |
| Check cystoscopy and CECT KUB | 31 | 42.5 | |
| Check cystoscopy and MRI KUB | 2 | 2.7 | |
| Not followed | 3 | 4.1 | |
| 16 | Post op MMC Instillation | 17 | 23.3 |
| 17 | Post op BCG Instillation | 6 | 8.2 |
| 18 | Survival | ||
| Expired | 14 | 19.2 | |
| Surviving | 59 | 80.8 | |
| 19 | Expired (n=14) | ||
| Expired due to cancer | 11 | 78.50% | |
| Expired due to other reasons | 3 | 11.50% | |
| 20 | Final Outcome (at 22 months) | ||
| Overall survival | 59 | 80.8 | |
| Disease specific survival | 62 | 84.9 | |
| Recurrence-free survival | 41 | 56.2 | |
| Survival with recurrence | 18 | 24.7 | |
| Bladder intact survival | 54 | 73.9 | |
| a: Partial cystectomy was done in 4 patients but in one patient, salvage radical cystectomy had to be done due to recurrence | |||
Age of patients enrolled in the study ranged from 18 to 78 years, mean age of patients was 56.08 ± 12.49 years.
The minimum tumor size was 2.5 cm while the maximum tumor size was 6.5 cm, and the average size of the tumor was 3.91 ± 0.98 cm.
We included patients with clinical stage T2-T4a out of which the most common stage was T3b (32.9%) followed by T2 (31.5%), T4a (21.9%), and T3a (13.7%).
Neoadjuvant chemotherapy was given in 5.5% of patients and pre-treatment hydronephrosis was present in 30.2% of patients. Unilateral hydronephrosis was present in 19.2% and bilateral in 11.0% cases.
TURBT was done in all but 2 (2.7%) cases as both patients were treated with partial cystectomy based on cold cup biopsy and radiological evidence of muscle infiltration and both showed deep muscle invasion in the postâ??operative histopathology of the specimen. In the majority of the cases TURBT was complete (52.1%).
All but three (4.1%) cases were subject to chemo-radiation-two because they had undergone only partial cystectomy as the modality of choice for bladder preservation and one. After all, the histology of the tumor was adenocarcinoma in which chemo-radiation was not indicated.
A complete response to chemo-radiation i.e. complete disappearance of tumor on follow-up cystoscopy, imaging, and scar biopsy was observed in 58.9% of cases.
Out of the 73 cases of bladder preservation therapy patients, 5 (6.85%) required salvage radical cystectomy followed by chemotherapy. Out of these 5 patients, one patient expired after 5 months of salvage radical cystectomy due to metastases.
Patients were followed up for 3 to 22 months; the average follow-up duration was 13.21 ± 9.79 months.
Histopathologically, 70 (95.9%) cases were transitional cell carcinoma, 2 (2.7%) cases were adenocarcinoma and 1 (1.4%) case was leiomyosarcoma.
Out of 32 cases with the incomplete response, chemo-radiation therapy was continued in 13 cases, 5 patients opted for salvage radical cystectomy, and the rest 14 patients expired before any further intervention.
Fourteen patients (19.1%) died out of which 3 (4.1%) patients died because of reasons other than cancer and the rest 11 (15%) patients died because of cancer itself (metastases were the most common reason).
Overall Survival (OS), Recurrence Free Survival (RFS), and Diseaseâ??Specific Survival (DSS) at 22 months of followâ?? up were 80.8%, 56.2%, and 84.9% respectively.
The number of females was higher among deaths (28.6% vs. 16.9%) but this difference too was not found to be significant statistically (p-value=0.321).
The average tumor size of cases who died (4.32 ± 0.83 cm) was found to be higher as compared to that of surviving patients (3.81 ± 1.00 cm) but this difference was not found to be significant statistically (p-value=0.082).
It was observed that as the stage of the disease increased, survival decreased and the number of deaths increased and this difference was found to be significant statistically (p=0.018) (Table 2).
| Clinical Stage | Deaths (n=14) | Survived (n=59) | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| T2 | 1 | 7.1 | 22 | 37.3 | 10.082 | 0.018 |
| T3a | 1 | 7.1 | 9 | 15.3 | ||
| T3b | 5 | 35.7 | 19 | 32.2 | ||
| T4a | 7 | 50 | 9 | 15.3 | ||
Among patients who died, the majority of the cases had incomplete TURBT (78.6%) while among surviving cases, the majority of cases had complete TURBT (61.4%). This difference was found to be significant statistically (p=0.007) (Table 3).
| TURBT Status | Deaths (n=14) | Survived (n=57)* | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| Incomplete | 11 | 78.6 | 22 | 38.6 | 7.22 | 0.007 |
| Complete | 3 | 21.4 | 35 | 61.4 | ||
Out of 73 cases that underwent bladder preservation therapy, chemo-radiation was not offered in 3 cases, because in them, the modality of treatment was partial cystectomy only and one patient’s histology turned out to be adenocarcinoma in which chemo-radiation was not indicated.
Among expired cases, the majority had an incomplete response to chemo-radiation (85.7%) while among survived cases majority had a complete response to chemo-radiation (70.7%). This difference was found to be significant statistically (p<0.001) (Table 4).
| Chemoradiation | Expired (n=14) | Survived (n=56)* | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| Incomplete | 12 | 85.7 | 16 | 28.5 | 14.916 | <0.001 |
| Complete | 2 | 14.3 | 40 | 71.4 | ||
| *Chemoradiation not offered in 3 cases | ||||||
It was observed that as the performance status of patients declined (ECOG score increased), survival decreased (p<0.001) (Table 5).
| ECOG* Score | Expired (n=14) | Survived (n=59) | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| 0 | 1 | 7.1 | 22 | 37.3 | 17.653 | <0.001 |
| 1 | 6 | 42.9 | 33 | 55.9 | ||
| 2 | 7 | 50 | 4 | 6.8 | ||
| *ECOG: Eastern Co-Operative Oncology Group | ||||||
The size of tumors in cases with incomplete TURBT was found to be significantly higher (4.59 ± 0.93 vs. 3.37 ± 0.61) as compared to those with complete TURBT (p<0.001) (Table 6).
| Parameter | Visibly incomplete TURBT (n=33) | Visibly complete TURBT (n=38) | Statistical significance |
|---|---|---|---|
| Mean tumor size ± SD (in cm) | 4.59 ± 0.93 | 3.37 ± 0.61 | ‘t’=6.619; p<0.001 |
| *TURBT not done in 2 cases | |||
It was observed that cases in which visibly complete TURBT was achievable had lower clinical T stages and in higher clinical T stages, TURBT was visibly incomplete (p=0.016) (Table 7).
| Parameter | Visibly incomplete TURBT (n=33) | Visibly complete TURBT (n=38) | Statistical significance | |||
|---|---|---|---|---|---|---|
| Clinical Stage | No. | % | No. | % | χ2 | ‘p’ |
| T2 | 5 | 15.2 | 17 | 44.7 | 0.228 | 0.016 |
| T3a | 5 | 15.2 | 5 | 13.2 | ||
| T3b | 11 | 33.3 | 12 | 31.6 | ||
| T4a | 12 | 36.4 | 4 | 10.5 | ||
| *TURBT not done in 2 cases | ||||||
The majority of the cases with incomplete TURBT had an incomplete chemo-radiation response (60.6%) while the majority of cases with complete TURBT had a complete chemoradiation response (78.3%), this difference was found to be statistically significant (p=0.001) (Table 8).
| Parameter | Visibly incomplete TURBT (n=33) | Visibly complete TURBT (n=37) | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| Chemoradiation response | ||||||
| Incomplete | 20 | 60.6 | 8 | 21.7 | 11.569 | 0.001 |
| Complete | 13 | 39.4 | 29 | 78.3 | ||
| *chemoradiation not offered in 3 cases | ||||||
Mean tumor size of cases with incomplete response to chemoâ??radiation (4.29 ± 0.89 cm) was found to be significantly higher as compared to cases with complete response to chemoradiation (3.67 ± 0.98 cm) and this difference was found to be statistically significant (p=0.008) (Table 9).
| Parameter | Incomplete response to chemoradiation (n=28) | Complete response to chemoradiation (n=42) | Statistical significance |
|---|---|---|---|
| Mean tumor size ± SD (in cm) | 4.29 ± 0.89 | 3.67 ± 0.98 | ‘t’=2.731; p=0.008 |
| *chemoradiation not offered in 3 cases | |||
More patients with incomplete responses to chemo-radiation were found to have hydronephrosis on pre-treatment imaging (p=0.015). It was also observed that bilateral hydronephrosis was more common in patients with incomplete responses to chemoradiation (Table 10).
| Parameter | Incomplete response to chemo-radiation (n=28) | Complete response to chemo-radiation (n=42) | Statistical significance | |||
|---|---|---|---|---|---|---|
| No | % | No | % | χ2 | ‘p’ | |
| Hydronephrosis | ||||||
| Absent | 17 | 60.7 | 32 | 76.2 | 8.357 | 0.015 |
| Unilateral | 5 | 17.8 | 9 | 21.42 | ||
| Bilateral | 6 | 21.42 | 1 | 2.3 | ||
Patients with incomplete response to chemo-radiation were observed to have a higher clinical stage of disease and the difference was found to be significant statistically (p=0.002) (Table 11).
| Parameter | Incomplete response to chemoradiation (n=28) | Complete response to chemoradiation (n=42) | Statistical significance | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | ‘p’ | |
| Clinical Stage | ||||||
| T2 | 3 | 10.7 | 18 | 42.85 | 14.502 | 0.002 |
| T3a | 2 | 7.1 | 8 | 19.04 | ||
| T3b | 11 | 39.2 | 12 | 28.57 | ||
| T4a | 12 | 42.8 | 4 | 9.5 | ||
| *chemoradiation not offered in 3 cases | ||||||
In our study, the major intervention done was TUR biopsy followed by chemo-radiation irrespective of the clinical stage (65.2% of patients with T2 stage, 91.2% of patients with T3 stage, and 87.5% of patients with T4 stage).
Partial cystectomy was done in 4 cases out of which 2 were T2 stage, and one each in were T3 and T4 stages. Out of the 4 cases, recurrence was found in 2 cases-one who underwent salvage radical cystectomy that is doing well and is on regular follow up and one patient expired due to metastases. The other 2 cases had a complete response and are on regular follow-up.
In ten patients, the modality opted for was maximal TURBT followed by chemoradiation out of which 6, 2 and 2 patients had T2, T3, and T4 stages respectively.
So out of 73 patients, 60 (82.2%) patients underwent TUR biopsy followed by chemo-radiation, and 13 (17.8%) patients underwent surgery (Partial cystectomy or Maximal TURBT).
At the end of 22 months, out of 73 patients who completed bladder preservation therapy, 14 (19.2%) patients died. Three patients died because of reasons other than cancer. Overall survival was 80.8% and diseaseâ??specific survival was 84.9 %. Forty-one (56.2%) patients are surviving without recurrence i.e. patients who have achieved a complete response to bladder preservation therapy and 18 (24.7%) patients are surviving with recurrent disease in the bladder. Of the 73 patients, 14 (80.8%) patients died and 5 patients underwent salvage radical cystectomy (of which one patient died). The 14 patients who died include this one patient. So patients surviving with an intact bladder at end of the study period were 55 (75.3%) (Table 12).
| Final Outcome (at 22 months) | No. | % |
|---|---|---|
| Overall survival | 59 | 80.8 |
| Disease specific survival | 62 | 84.9 |
| Recurrence-free survival | 41 | 56.2 |
| Survival with recurrence | 18 | 24.7 |
| Bladder intact survival | 55 | 75.3 |
On univariate analysis, only higher clinical T stage, incomplete TURBT, incomplete response to chemoradiation, and poor performance status (higher ECOG score) were associated with decreased survival (Table 13).
| S. No. | Parameter | Deaths (n=14) | Survived (n=59) | p-value |
|---|---|---|---|---|
| 1 | Mean age (Years) | 58.36 ± 12.7 | 55.5 ± 12.49 | 0.452 |
| 2 | Gender | |||
| Female | 4 (28.6%) | 10 (16.9%) | 0.321 | |
| Male | 10 (71.4%) | 49 (83.1%) | ||
| 3 | Co-existing disease | |||
| No | 10 (71.4%) | 44 (74.6%) | 0.809 | |
| Yes | 4 (28.6%) | 15 (25.4%) | ||
| 4 | Mean tumor size | 4.32 ± 0.83 cm | 3.81 ±1.00 cm | 0.082 |
| 5 | Clinical T stage | |||
| T2 | 1 (7.1%) | 22 (37.3%) | 0.018 | |
| T3a | 1 (7.1%) | 9 (15.3%) | ||
| T3b | 5 (35.7%) | 19 (32.2 %) | ||
| T4a | 7 (50.0%) | 9 (15.3 %) | ||
| 6 | TURBT status | |||
| Incomplete | 11 (78.57%) | 22 (38.59%) | 0.007 | |
| Complete | 3 (21.43% | 35 (61.40%) | ||
| 7 | Response to chemo-radiation | |||
| Incomplete | 12 (85.71%) | 17 (29.82%) | <0.001 | |
| Complete | 2 (14.29%) | 41 (71.18%) | ||
| 8 | ECOG score | |||
| 0 | 1 (7.1%) | 22 (37.3%) | <0.001 | |
| 1 | 6 (42.9%) | 33 (55.9%) | ||
| 2 | 7 (50.0%) | 4 (6.8%) | ||
On multivariate analysis, none of the parameters was found to be significantly associated with survival (Table 14).
| B | S.E. | Wald | df | p-value | |
|---|---|---|---|---|---|
| Age | 0.034 | 0.1 | 0.117 | 1 | 0.732 |
| Sex | 5.534 | 4.571 | 1.465 | 1 | 0.226 |
| Coexisting disease | 6.093 | 5.362 | 1.291 | 1 | 0.256 |
| UVJ involvement | -4.507 | 10746.39 | 0.000 | 1 | 1 |
| Clinical T Stage | -14.483 | 13.78 | 1.105 | 1 | 0.293 |
| Tumour size | 11.382 | 7.927 | 2.062 | 1 | 0.151 |
| Hydronephrosis | 2.002 | 10746.39 | 0.000 | 1 | 1 |
| TURBT status | 20.034 | 14.894 | 1.809 | 1 | 0.179 |
| Mode of intervention | -9.28 | 6.012 | 2.383 | 1 | 0.123 |
| Performance status (ECOG score) | -13.241 | 8.935 | 2.196 | 1 | 0.138 |
| Neoadjuvant chemotherapy | -1.559 | 2.053 | 0.577 | 1 | 0.448 |
| Chemoradiation Response | -14.884 | 12.927 | 1.326 | 1 | 0.25 |
| Follow up duration | 0.693 | 0.4 | 2.996 | 1 | 0.083 |
| Intervention Response | -46.969 | 4623.129 | 0.000 | 1 | 0.992 |
| Constant | 95.466 | 9246.43 | 0.000 | 1 | 0.992 |
Survival Analyses (Kaplan Meier Curves)
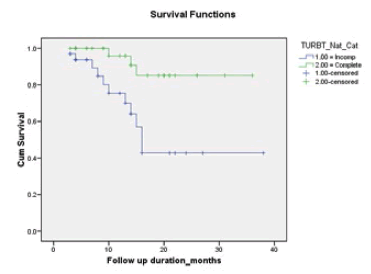
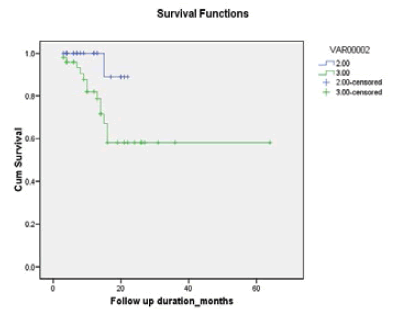
Survival of patients with complete TURBT was found to be superior to patients with incomplete TURBT (p=0.003) (Table 15, and Figure 2).
| TURBT Status | Total | No. of deaths (%) | Mean follow up duration (months) | S.E. | 95% CI |
|---|---|---|---|---|---|
| Incomplete | 33 | 11 (33.3%) | 13.48 | 1.38 | 10.78-16.18 |
| Complete | 38 | 3 (7.9%) | 13.68 | 1.15 | 11.42-15.94 |
| Log Rank (Mantel-Cox): χ2=8.890; p=0.003 *TURBT not done in 2 cases |
|||||
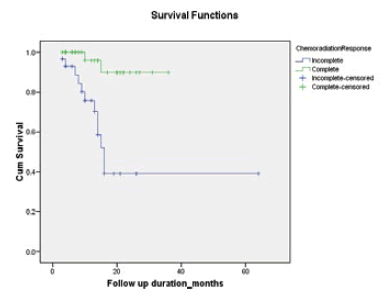
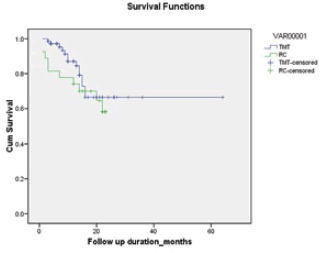
Survival of patients with complete response to chemoradiation was found to be superior to patients with incomplete response to chemo-radiation (p ≤ 0.001) (Table 16, and Figure 3).
| Chemo-radiation Response | Total | No. of deaths (%) | Mean follow up duration (months) | S.E. | 95% CI |
|---|---|---|---|---|---|
| Incomplete | 27 | 12 (41.4%) | 32.12 | 6.08 | 20.20-44.03 |
| Complete | 43 | 2 (4.7%) | 33.66 | 1.58 | 30.56-36.76 |
| Log Rank (Mantel-Cox): χ2=12.676; p<0.001 *Chemotherapy not offered in 3 cases |
|||||
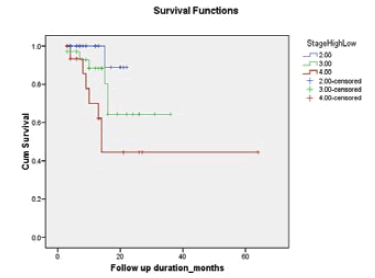
Survival was seen in the clinical T stage. We found that survival of T2 was better than the survival of T3 which in turn was better than the survival of T4 patients and T3 cases (p=0.024). In a head-to-head comparison, only the association between T2 and T4 was found to be significant (p=0.002) (Table 17, and Figure 4).
| Clinical Stage | Total | No. of deaths (%) | Mean follow up duration (months) | S.E. | 95% CI |
|---|---|---|---|---|---|
| T2 | 23 | 1 (4.3%) | 21.22 | 0.73 | 19.79-22.66 |
| T3a-3b | 34 | 6 (17.6%) | 27.75 | 2.83 | 22.20-33.30 |
| T4a | 16 | 7 (43.7%) | 34.31 | 7.62 | 19.37-49.25 |
| Log Rank (Mantel-Cox): χ2=7.427; p=0.024 | |||||
It was found that survival in patients with the T2 stage was better when compared with T3 and T4 combined (p=0.049) (Table 18, and Figure 5).
| Clinical Stage | Total | No. of expiry (%) | Mean follow up duration(months) | S.E. | 95% CI |
|---|---|---|---|---|---|
| T2 | 23 | 1 (4.3%) | 21.22 | 0.73 | 19.79-22.66 |
| T3a-3b+T4a | 50 | 13 (26.0%) | 42.13 | 4.86 | 32.60-51.66 |
| Log Rank (Mantel-Cox): χ2=3.861; p=0.049 | |||||
It was found that survival of patients with T2 and T3 stages combined was better when compared with T3 stage (p=0.013) (Table 19, and Figure 6).
| Clinical Stage | Total | No. of expiry (%) | Mean follow up duration(months) | S.E. | 95% CI |
|---|---|---|---|---|---|
| T2+ T3a-3b | 57 | 7 (12.3%) | 30.13 | 1.97 | 26.27-33.99 |
| T4a | 16 | 7 (43.7%) | 34.31 | 7.62 | 19.37-49.25 |
| Log Rank (Mantel-Cox): χ2=6.114; p=0.013 | |||||
To compare the outcome of bladder preservation therapy with radical cystectomy, which is the standard treatment for muscle invasive bladder cancer, we also retrospectively reviewed patients diagnosed with muscle invasive bladder carcinoma who underwent radical cystectomy in our study period. There were 31 such patients (Table 20). Four (12.9%) patients were lost to follow-up (they didn’t come to follow-up and are non-traceable).
| SN | Outcome | No. of cases | Percentage |
|---|---|---|---|
| 1 | Followed up | 27 | 87.1 |
| 2 | Lost to follow up | 4 | 12.9 |
| Total | 31 | 100.0 |
In the majority of cases (59.2%), the urinary diversion of choice was orthotopic neobladder followed by ileal conduit (33.3%) with the least common being cutaneous ureterostomy (7.4%) (Table 21).
| SN | Type of diversion | No. of cases | Percentage |
|---|---|---|---|
| 1 | Ileal conduit | 9 | 33.3 |
| 2 | Orthotopic neobladder | 16 | 59.2 |
| 3 | Cutaneous ureterostomy | 2 | 7.4 |
Overall survival among radical cystectomy cases was 63.0% at a median follow-up of 17.52 months (Table 22). The following table shows the outcome of 27 MIBC cases that underwent radical cystectomy.
| SN | Outcome | No. of cases | Percentage |
|---|---|---|---|
| 1 | Deaths | 10 | 37.0 |
| 2 | Alive | 17 | 63.0 |
| Total | 27 | 100.0 |
Out of the 10 patients who died after radical cystectomy, 4 each had ileal conduit and orthotopic neobladder and 2 patients had cutaneous ureterostomy type of urinary diversion. Incidentally, all 2 patients (100%) in whom cutaneous ureterostomy was made, died (Table 23).
| SN | Type of urinary diversion | No. of cases | Percentage |
|---|---|---|---|
| 1 | Ileal conduit | 4 | 40 |
| 2 | Orthotopic neobladder | 4 | 40 |
| 3 | Cutaneous ureterostomy | 2 | 20 |
| Total | 10 | 100.0 |
Out of the 10 patients who died, 3 died in the perioperative period (within 30 days of surgery).
Survival of the bladder preservation therapy group was non-inferior to the survival of the radical cystectomy group (p=0.364) (Figure 7).
Discussion
Organ preserving approaches have been successfully accepted and adopted for various cancers like anal, breast, head and neck, renal, larynx, limb, esophagus, and prostate. As far as bladder cancer is concerned, the bladder conservation approach for Muscle Invasive Bladder Cancer (MIBC) has met with resistance.
Radical cystectomy with lymph node dissection remains widely accepted as the standard treatment for MIBC with 5-year Overall Survival (OS) ranging from 45% to 66% [3]. Nevertheless, removal of the bladder leads to significant morbidity and affects patients’ quality of life. Bladder preservation treatment strategies have evolved over the past 20 years with continued refinements in Radiation Therapy (RT), chemotherapy for radiation sensitization, and patient selection that can provide selected patients with an excellent chance for long-term survival with an intact, functioning bladder. Several bladder preservation options exist [13,20,22-24]. The hallmarks of modern bladder-preserving therapy include Combined-Modality Therapy (CMT) with maximal Transurethral Resection of Bladder Tumor (TURBT), RT, and concurrent chemotherapy. An early assessment of treatment response is performed by cystoscopy, CT or MRI, urine cytology, and scar biopsy. Patients achieving clinical complete response continue with consolidative chemo-radiotherapy. Incomplete responders are advised to undergo immediate cystectomy (known as salvage radical cystectomy). Those with conserved bladders are followed by close cystoscopic surveillance, with prompt salvage cystectomy at the first sign of invasive recurrence.
A multimodality therapy approach, including visually complete Transurethral Resection of Bladder Tumor (TURBT) followed by chemotherapy and radiotherapy, is the most studied bladder-sparing strategy. Long-term follow-ups from several institutions have shown that this multimodality treatment leads to an excellent chance for long-term survival ranging from 50% to 60% with the preserved bladder [18,19,25-28].
Unfortunately, there are no completed randomized comparisons available, nor will there likely be given the failure of the Selective Bladder Preservation against Radical Excision trial to accrue patients [8]. Any direct comparison between TMT and RC series is naturally confounded by selection biases and discordance between clinical and pathologic staging [29]. Those limitations aside, the 5-yr and 10-yr OS and DSS rates in contemporary RC series, whether in combination with neoadjuvant chemotherapy or not, are comparable to those seen in various bladder preservation therapy series [1-4,19-21,26]. An additional barrier to the wider use of bladder preservation therapy relates to concerns regarding the efficacy and feasibility of salvage cystectomy. Reassuringly, among those patients with an incomplete response to chemoradiation or an invasive relapse identified on follow-up cystoscopy, salvage RC could still be performed with curative intent, with 5-yr and 10-yr DSS rates of 58% and 44%, respectively. Furthermore, salvage RC can be performed with acceptable morbidity with no evidence of increased 30-day or 60-day mortality in patients undergoing salvage RC after pelvic radiation therapy relative to non-irradiated patients [30,31].
In our prospective study of MIBC patients, our primary aim was to see the outcome of bladder preservation therapy and the secondary aim was to compare it with the outcome of radical cystectomy over the study period. Throughout the study period, 116 patients were diagnosed with MIBC. Thirty-one patients underwent radical cystectomy and the rest of the patients i.e. 85 patients underwent bladder preservation therapy. Out of the 85 patients, 12 patients were lost to follow-up due to several reasons. Seventy-three patients completed the bladder preservation therapy. We performed maximally safe TURBT for the patients and waited for the biopsy results. Non-muscle invasive cancers were treated and followed up as per protocol.
Muscle invasive bladder cancer patients were given a choice between radical cystectomy and bladder preservation therapy. The disease was staged with computed tomography and only patients with clinical stages T2 to T4a were included.
We demonstrate the overall survival of patients who underwent bladder preservation therapy to be 80.8%, with disease-specific survival of 62% at 22 months (median follow-up of 11.9 months) which matches the world literature. We also reviewed patients who underwent radical cystectomy and found their overall survival to be 63% at 22 months (median follow-up of 17.5 months).
In RTOG pooled analysis of long-term outcomes of selective bladder preservation therapy in the multi-institutional setting, it was found that this modality results in low rates of invasive tumor recurrence (5 and 10-year DSS, 71% and 65% respectively) and OS (5 and 10 years OS, 57% and 36% respectively), with 80% of patients retaining intact bladder at 5 years. This study provided a unique insight into the outcomes of the bladder preservation therapy approach over two decades in the multi-institutional setting with one of the largest cohorts of patients to date [19].
Efstathiou, et al., studied long-term outcomes of selective bladder preservation by combined modality therapy for muscle invasive bladder cancer at Massachusetts general hospital [18]. In their study, Seventy-two percent of patients (78% with stage T2) had CR to induction therapy. 5, 10, and 15 year DSS rates were 64%, 59%, and 57% (T2=74%, 67%, and 63%; T3-4=53%, 49%, and 49%), respectively. 5, 10, and 15 year OS rates were 52%, 35%, and 22% (T2: 61%, 43%, and 28%; T3-4=41%, 27%, and 16%), respectively. Among patients showing CR, 10-yr rates of noninvasive, invasive, pelvic, and distant recurrences were 29%, 16%, 11%, and 32%, respectively. Among patients undergoing visibly complete TURBT, only 22% required cystectomy (vs. 42% with incomplete TURBT; log-rank p<0.001). In multivariate analyses, clinical T-stage and CR were significantly associated with improved DSS and OS. The use of neo-adjuvant chemotherapy did not improve outcomes.
Chiang, et al. reported 5 years overall, progression-free, and bladder preservation-specific survival rates of 76.3%, 62.9%, and 71.5% respectively [32]. They had enrolled 60 patients in their study with a median follow-up of 86.7 months. Three patients underwent salvage cystectomies for invasive recurrences. Of 45 surviving patients, 42 patients (93.3%) retained functioning bladders. In our study, out of the out of 59 surviving patients, 55 (91.52%) patients retained functioning bladders.
In our study, we confirm the favorable outcome of bladder preservation therapy in patients with muscle invasive bladder cancer. We also confirm non-inferior survival of bladder preservation therapy over radical cystectomy (p=0.32). Though the limitation of our study is that our follow-up is short (11.97 ± 6.56 months) but we are hopeful that with a longer follow-up, we would get a similar outcome.
In our study, on the univariate analysis we found that poor overall survival was significantly associated with increasing T stage of disease (p=0.018), incomplete TURBT (p=0.007), and incomplete response to chemo-radiation (p<0.001), and poorer performance status (ECOG) (p<0.001). But on multivariate analysis, none of the parameters (mean age, gender, mean tumor size, clinical T stage, visibly complete/incomplete TURBT, response to chemo-radiation, performance score) was found to be significantly associated with survival.
In a study by Chiang, et al. on univariate analysis, patients with younger age (<60 years) had higher overall survival (p=0.03) and DMFS (p=0.02) [32]. Patients with unfavorable factors had significantly lower OS (61.4% vs. 80.2%, p=0.007) and DMFS (53% vs. 78.9%, p=0.002) on univariate analysis, and the unfavorable factor was the only independent factor in multivariate analysis (hazard ratio, 4.4; 95% confidence interval,1.6e12; p=0.03). Giacalone, et al. on multivariate analysis, found increasing age at diagnosis, clinical T2 disease, complete response to chemoradiation, presence of hydronephrosis, and presence of tumor-associated CIS to be significant predictors for overall survival [33].
We found in our study that increased tumor size (p<0.001), and higher clinical T stage (p=0.016) were associated with visibly incomplete TURBT. This is relatable because as tumor size increases, its probability of being completely resectable goes down. Similarly as tumor size increases, its T stage increases. Out of 70 patients who received chemoradiation, 28 patients (40%) had an incomplete response, and the rest 42 patients (60%) had a complete response. The probability of incomplete response increased with visibly incomplete TURBT (p=0.001), larger tumor size (p=0.008), higher clinical T stage (p=0.002), and presence of pre-intervention hydronephrosis (p=0.015). Giacolone, et al. found both response to chemoradiation and clinical T stage as significant predictors for both OS and DSS [33]. Interestingly, they also showed that both hydronephrosis and tumor-associated CIS were associated with OS, whereas only the latter was significantly associated with DSS. Regarding CR to chemoradiation, they showed that their ability to achieve a CR is itself associated with the clinical T stage and the completeness of the initial TURBT. Notably, however, even in patients with an incomplete TURBT or more advanced T stage (i.e. cT3-4a); over 50% can still achieve a CR to induction therapy. An exploratory analysis of their patients showed a marked improvement in the rates of CR and DSS over time. The improvements in CR have in turn resulted in a marked reduction in the need for salvage RC. These improvements are likely explained in several ways. In part, it is likely due to evolving criteria for patient selection. For example, patients with hydronephrosis were excluded from protocol treatment beginning with RTOG 9506, due to prior data suggesting that hydronephrosis was associated with reduced rates of CR to chemoradiation. Hydronephrosis also increases the likelihood of decreased renal function, thereby affecting the ability to receive platinum-based chemotherapy. It is also plausible that improvements in the TURBT technique and the completeness of resection, advances in radiation therapy (e.g., computed tomography planning, three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, and the introduction of image-guided radiotherapy), optimized concurrent chemotherapeutic regimens, and improved supportive care may have contributed to improvements in CR rates and survival.
The modality of bladder preservation therapy in our study was TUR biopsy followed by chemoradiation (60 patient-82.2%), maximally safe TURBT followed by chemoradiation (10 patients-13.8%), and partial cystectomy (3 patients-4%) (p=0.035). Total 4 patients had undergone partial cystectomy as the primary modality of treatment out of which 2 were T2 stage and one each in were T3 and T4 stages. Out of the 4 cases, recurrence was found in 2 casesone who underwent salvage radical cystectomy that is doing well and is on regular follow up and one patient died due to metastases. The other 2 patients had a complete response and are on regular follow-up. Compared with radical cystectomy, removal of a portion of the bladder may result in better retention of sexual function. Optimal candidates for partial (segmental) cystectomy are those who have solitary lesions with focal muscularis propria involvement located either anteriorly or on the bladder dome where a 1- to 2-cm resection margin is possible [34]. Patients should also have an absence of carcinoma in situ secondary to an increased risk of recurrence [35]. In addition, Smaldone, et al. demonstrated that, in 25 highly selected patients who underwent partial cystectomy for solitary tumors, tumor size was significantly associated with local recurrence [36]. In appropriately selected patients, partial cystectomy can result in long-term, bladder-intact survival rates ranging from 50% to 75% [10-13]. However, only 5% to 10% of patients with cT1N0 to cT2N0 disease are candidates for this treatment.
Bilateral pelvic lymphadenectomy should be performed and minimally include common, internal, and external iliac, and obturator nodes. For well-selected patients, outcomes appear to be reasonable for partial cystectomy. In an analysis of population data, Capitanio, et al. found that 5â??year overall survival and cancerâ??specific survival for partial cystectomy matched those for RC (57.2% and 70.3% compared to 54.6% and 69.2%) in patients matched for age, race, TNM stage, grade, and several removed lymph nodes [7]. As summarized in Table 7, overall 5-year survival for patients undergoing partial cystectomy for MIBC is between 50% and 70%, with up to 81% of patients retaining their native bladder at 10 years [6,7,35-40]. In addition, the question of whether or not to utilize neoadjuvant chemotherapy before partial cystectomy has also been addressed in a small, nonrandomized series.
Bazzi, et al. reported on their contemporary experience with the use of partial cystectomy post neoadjuvant chemotherapy as a bladder-sparing modality in 36 highly selected patients [38]. They found that at the last follow-up, 19 (53%) patients had a recurrence, 15 (42%) had advanced recurrences (defined as a recurrence that could not be addressed with intravesical therapy or RC), 10 (28%) died of disease, and 1 died of another cause [38]. Five-year recurrence-free survival and overall survivals were 28% and 63%, respectively. Furthermore, 56% of patients had no evidence of disease after a median follow-up of 17 months, and 22 (61%) had an intact bladder [38]. The authors concluded that these results were consistent with similar previous small series of oncologic outcomes in patients receiving neoadjuvant chemotherapy followed by partial cystectomy and established this modality as a viable alternative to neoadjuvant chemotherapy and RC in carefully selected patients [38-41]. Because the bladder remains a source of recurrence, patients counseled for partial cystectomy must understand that postoperative surveillance is mandatory. In addition to imaging of the chest, upper tracts, abdomen, and pelvis, NCCN guidelines recommend cystoscopy and urine cytology, ± mapping biopsies, in addition to laboratory testing every 3-6 months for 2 years and then increasing intervals as appropriate [42]. Recurrence rates (noninvasive+invasive) have been as high as 38%-49% with 7%-30% of partial cystectomy patients ultimately undergoing RC 5-year recurrence-free survival is similar at 56% and 66%, respectively [43]. These findings underscore the great importance of appropriate patient selection and patient compliance with follow-up in implementing partial cystectomy for MIBC.
On Kaplan Meier curve analyses of different parameters for survival, we found that survival of patients decreased with TURBT being incomplete (p=0.003), with incomplete response to chemoradiation (p<0.001), and with increasing clinical T stage (p=0.024).
According to various studies, bladder preservation yields a 5-year OS rate of approximately 50%. Contemporary bladder preserving approaches in patients with clinically staged MIBC can achieve complete response rates of 60%- 70% and bladder intact survival rates of 40%-45% [25,26]. Importantly, the bladder is retained in the majority of the surviving patients. Several large surgical series that report outcomes after radical cystectomy has been recently published. Modern radical cystectomy series have demonstrated 5-year overall survival rates of 56%-66% [1-4]. In our study, the survival of bladder preservation therapy was found to be non-inferior to the survival of radical cystectomy patients.
More studies would be needed in the future to bring bladder preservation therapy into the main line of treatment. Bladder preservation therapy is a boon in itself as patients retain their quality of life. It is a limitation that ethically, a randomized controlled trial is not feasible to compare radical cystectomy and bladder preservation therapy.
Comparisons between surgical series and bladder preservation protocols are hindered by the difference in pathologic staging (used in surgical series) and clinical staging (used in bladder preservation series). This bias would tend to favor surgical series since clinical staging generally tends to understage patients.
Although results between bladder conservation approaches and modern radical cystectomy series for muscle-invasive bladder cancer appear comparable, no prospective randomized trial to compare both modalities have been performed. In our opinion, radical cystectomy continues to be the standard of care for muscle-invasive bladder cancer. However, we think that there are enough data to justify a formal prospective randomized trial to compare radical cystectomy vs. tri-modality bladder-conserving protocol in patients who would have been eligible for the RTOG protocols.
However, more research is required before we can confidently choose bladder preservation therapy over radical cystectomy for patients with muscle invasive bladder cancer for select patients.
Limitations of the Study
• Short follow-up period.
• Follow-up compliance issues in 16.4% of cases.
• Three patients had different histology than urothelial carcinoma. They were adenocarcinoma and leiomyosarcoma.
• Four patients recruited in the study already had undergone TURBT before recruitment at another center and their initial disease data were collected retrospectively which might have the potential for having some inaccuracy. Although these patients were later followed prospectively after recruitment.
Conclusion
The majority (70%) of patients with muscle invasive bladder carcinoma chose or were suitable to undergo bladder preservation therapy and the rest (30%) chose or were suitable to undergo radical cystectomy. In the bladder preservation therapy group, the majority (82.2%) of patients underwent chemo-radiation after TUR biopsy, 4.1% of patients underwent partial cystectomy and 13.7% of patients underwent maximal (radical) TURBT followed by chemoradiation. A complete response to chemoradiation i.e. complete disappearance of tumor on follow-up cystoscopy, imaging, and scar biopsy was observed in more than half of the cases (58.9%). Overall survival, recurrence-free survival, disease-specific survival, and bladder intact survival in the bladder preservation therapy group at 22 months follow-up (Median follow-up period-11.97 months) were 80.8%, 56.2%, 84.9%, and 75.3% respectively. A minority of patients (6.85%) required salvage radical cystectomy. On univariate analysis, higher clinical T stage, incomplete TURBT, incomplete response to chemo-radiation, and poor performance status (higher ECOG score) were associated with decreased survival in the bladder preservation therapy group, although in multivariate analysis, none of these parameters were found to be statistically significant. Mortality and morbidity of bladder preservation therapy were acceptable. On Kaplan Meier curve analyses of different parameters for survival, we found that survival of patients decreased with TURBT being incomplete, with incomplete response to chemo-radiation, and with increasing clinical T stage. Survival of bladder preservation therapy patients was non-inferior to the survival of radical cystectomy patients at 22 months of follow-up.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Grossman, H. Barton, et al. "Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer." New England Journal of Medicine, Vol. 349, No. 9, 2003, pp. 859-66.
Google Scholar Crossref - Sherif, Amir, et al. "Neoadjuvant cisplatinum based combination chemotherapy in patients with invasive bladder cancer: A combined analysis of two Nordic studies." European Urology, Vol. 45, No. 3, 2004, pp. 297-303.
Google Scholar Crossref - Stein, John P., et al. "Radical cystectomy in the treatment of invasive bladder cancer: Long-term results in 1,054 patients." Journal of Clinical Oncology, Vol. 19, No. 3, 2001, pp. 666-75.
Google Scholar Crossref - Zehnder, Pascal, et al. "Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: A comparative study." The Journal of Urology, Vol. 186, No. 4, 2011, pp. 1261-68.
Google Scholar Crossref - Shabsigh, Ahmad, et al. "Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology." European Urology, Vol. 55, No. 1, 2009, pp. 164-76.
Google Scholar Crossref - Knoedler, John J., et al. "Does partial cystectomy compromise oncologic outcomes for patients with bladder cancer compared to radical cystectomy? A matched case-control analysis." The Journal of Urology, Vol. 188, No. 4, 2012, pp. 1115-19.
Google Scholar Crossref - Capitanio, Umberto, et al. "Partial cystectomy does not undermine cancer control in appropriately selected patients with urothelial carcinoma of the bladder: A population-based matched analysist." Urology, Vol. 74, No. 4, 2009, pp. 858-64.
Google Scholar Crossref - Huddart, Robert A., et al. "Life and death of spare (selective bladder preservation against radical excision): Reflections on why the spare trial closed." BJU International, Vol. 106, No. 6, 2010, pp. 753-55.
Google Scholar Crossref - National Institute for Clinical Excellence. "Bladder cancer: Diagnosis and management, NICE guideline [NG2]." 2015.
Google Scholar - Kaufman, Donald S., et al. "Selective bladder preservation by combination treatment of invasive bladder cancer." New England Journal of Medicine, Vol. 329, No. 19, 1993, pp. 1377-82.
Google Scholar Crossref - Tester, William, et al. "Combined modality program with possible organ preservation for invasive bladder carcinoma: Results of RTOG protocol 85-12." International Journal of Radiation Oncology* Biology* Physics, Vol. 25, No. 5, 1993, pp. 783-90.
Google Scholar Crossref - Tester, William, et al. "Neoadjuvant combined modality program with selective organ preservation for invasive bladder cancer: Results of Radiation Therapy Oncology Group phase II trial 8802." Journal of Clinical Oncology, Vol. 14, No. 1, 1996, pp. 119-26.
Google Scholar Crossref - Shipley, W. U., et al. "Phase III trial of neoadjuvant chemotherapy in patients with invasive bladder cancer treated with selective bladder preservation by combined radiation therapy and chemotherapy: Initial results of Radiation Therapy Oncology Group 89-03." Journal of Clinical Oncology, Vol. 16, No. 11, 1998, pp. 3576-83.
Google Scholar Crossref - Kaufman, Donald S., et al. "The initial results in muscle-invading bladder cancer of RTOG 95-06: Phase I/II trial of transurethral surgery plus radiation therapy with concurrent cisplatin and 5-fluorouracil followed by selective bladder preservation or cystectomy depending on the initial response." The Oncologist, Vol. 5, No. 6, 2000, pp. 471-76.
Google Scholar Crossref - Hagan, Michael P., et al. "RTOG 97-06: Initial report of a phase I-II trial of selective bladder conservation using TURBT, twice-daily accelerated irradiation sensitized with cisplatin, and adjuvant MCV combination chemotherapy." International Journal of Radiation Oncology* Biology* Physics, Vol. 57, No. 3, 2003, pp. 665-72.
Google Scholar Crossref - Kaufman, Donald S., et al. "Phase I-II RTOG study (99-06) of patients with muscle-invasive bladder cancer undergoing transurethral surgery, paclitaxel, cisplatin, and twice-daily radiotherapy followed by selective bladder preservation or radical cystectomy and adjuvant chemotherapy." Urology, Vol. 73, No. 4, 2009, pp. 833-37.
Google Scholar Crossref - Krause, Frens Steffen, et al. "15-year survival rates after transurethral resection and radiochemotherapy or radiation in bladder cancer treatment." Anticancer Research, Vol. 31, No. 3, 2011, pp. 985-90.
Google Scholar - Efstathiou, Jason A., et al. "Long-term outcomes of selective bladder preservation by combined-modality therapy for invasive bladder cancer: The MGH experience." European Urology, Vol. 61, No. 4, 2012, pp. 705-11.
Google Scholar Crossref - Mak, Raymond H., et al. "Long-term outcomes in patients with muscle-invasive bladder cancer after selective bladder-preserving combined-modality therapy: A pooled analysis of Radiation Therapy Oncology Group protocols 8802, 8903, 9506, 9706, 9906, and 0233." Journal of Clinical Oncology, Vol. 32, No. 34, 2014, pp. 3801-09.
Google Scholar Crossref - James, Nicholas D., et al. "Radiotherapy with or without chemotherapy in muscle-invasive bladder cancer." New England Journal of Medicine, Vol. 366, No. 16, 2012, pp. 1477-88.
Google Scholar Crossref - Hoskin, Peter J., et al. "Radiotherapy with concurrent carbogen and nicotinamide in bladder carcinoma." Journal of Clinical Oncology, Vol. 28, No. 33, 2010, pp. 4912-18.
Google Scholar Crossref - Gakis, Georgios, et al. "ICUD-EAU International Consultation on Bladder Cancer 2012: Radical cystectomy and bladder preservation for muscle-invasive urothelial carcinoma of the bladder." European Urology, Vol. 63, No. 1, 2013, pp. 45-57.
Google Scholar Crossref - Huddart, Robert A., et al. "Randomized noninferiority trial of reduced high-dose volume versus standard volume radiation therapy for muscle-invasive bladder cancer: Results of the BC2001 trial (CRUK/01/004)." International Journal of Radiation Oncology* Biology* Physics, Vol. 87, No. 2, 2013, pp. 261-69.
Google Scholar Crossref - Mitin, Timur, et al. "Transurethral surgery and twice-daily radiation plus paclitaxel-cisplatin or fluorouracil-cisplatin with selective bladder preservation and adjuvant chemotherapy for patients with muscle invasive bladder cancer (RTOG 0233): A randomised multicentre phase 2 trial." The Lancet Oncology, Vol. 14, No. 9, 2013, pp. 863-72.
Google Scholar Crossref - Shipley, W. U., et al. "Selective bladder preservation by combined modality protocol treatment: Long-term outcomes of 190 patients with invasive bladder cancer." Urology, Vol. 60, No. 1, 2002, pp. 62-67.
Google Scholar Crossref - Rodel, Claus, et al. "Combined-modality treatment and selective organ preservation in invasive bladder cancer: Long-term results." Journal of Clinical Oncology, Vol. 20, No. 14, 2002, pp. 3061-71.
Google Scholar Crossref - Housset, Martin, et al. "Combined radiation and chemotherapy for invasive transitional-cell carcinoma of the bladder: A prospective study." Journal of Clinical Oncology, Vol. 11, No. 11, 1993, pp. 2150-57.
Google Scholar Crossref - Chung, Peter WM, et al. "Long-term outcome of radiation-based conservation therapy for invasive bladder cancer." Urologic Oncology: Seminars and Original Investigations, Vol. 25, No. 4, 2007.
Google Scholar Crossref - Gray, Phillip J., et al. "Clinical-pathologic stage discrepancy in bladder cancer patients treated with radical cystectomy: Results from the national cancer data base." International Journal of Radiation Oncology* Biology* Physics, Vol. 88, No. 5, 2014, pp. 1048-56.
Google Scholar Crossref - Eswara, Jairam R., et al. "Complications and long-term results of salvage cystectomy after failed bladder sparing therapy for muscle invasive bladder cancer." The Journal of Urology, Vol. 187, No. 2, 2012, pp. 463-68.
Google Scholar Crossref - Ramani, Vijay AC, et al. "Differential complication rates following radical cystectomy in the irradiated and nonirradiated pelvis." European Urology, Vol. 57, No. 6, 2010, pp. 1058-63.
Google Scholar Crossref - Chiang, Yun, et al. "A role of multimodality bladder-preserving therapy in patients with muscle-invasive bladder cancer plus hydronephrosis with or without pelvic nodal involvement." Journal of the Formosan Medical Association, Vol. 116, No. 9, 2017, pp. 689-96.
Google Scholar Crossref - Giacalone, Nicholas J., et al. "Long-term outcomes after bladder-preserving tri-modality therapy for patients with muscle-invasive bladder cancer: An updated analysis of the Massachusetts General Hospital experience." European Urology, Vol. 71, No. 6, 2017, pp. 952-60.
Google Scholar Crossref - Sweeney, Patrick, Elroy D. Kursh, and Martin I. Resnick. "Partial cystectomy." Urologic Clinics of North America, Vol. 19, No. 4, 1992, pp. 701-11.
Google Scholar Crossref - Holzbeierlein, Jeffrey M., et al. "Partial cystectomy: A contemporary review of the Memorial Sloan-Kettering Cancer Center experience and recommendations for patient selection." The Journal of Urology, Vol. 172, No. 3, 2004, pp. 878-81.
Google Scholar Crossref - Smaldone, Marc C., et al. "Long-term results of selective partial cystectomy for invasive urothelial bladder carcinoma." Urology, Vol. 72, No. 3, 2008, pp. 613-16.
Google Scholar Crossref - Kassouf, Wassim, et al. "Partial cystectomy for muscle invasive urothelial carcinoma of the bladder: A contemporary review of the MD Anderson Cancer Center experience." The Journal of Urology, Vol. 175, No. 6, 2006, pp. 2058-62.
Google Scholar Crossref - Bazzi, Wassim M., et al. "Partial cystectomy after neoadjuvant chemotherapy: Memorial Sloan Kettering Cancer Center contemporary experience." International Scholarly Research Notices, Vol. 2014, 2014.
Google Scholar Crossref - Fahmy, Nader, et al. "Practice patterns and recurrence after partial cystectomy for bladder cancer." World Journal of Urology, Vol. 28, No. 4, 2010, pp. 419-23.
Google Scholar Crossref - Ma, B., et al. "Lymphovascular invasion, ureteral reimplantation and prior history of urothelial carcinoma are associated with poor prognosis after partial cystectomy for muscle-invasive bladder cancer with negative pelvic lymph nodes." European Journal of Surgical Oncology (EJSO), Vol. 39, No. 10, 2013, pp. 1150-56.
Google Scholar Crossref - Lyons, Matthew D., and Angela B. Smith. "Surgical bladder-preserving techniques in the management of muscle-invasive bladder cancer." Urologic Oncology: Seminars and Original Investigations, Vol. 34, No. 6, 2016, pp. 262-70.
Google Scholar Crossref - Clark, P. E., et al. "Bladder cancer. NCCN Clinical Practice Guidelines in Oncology 2016." Journal of the National Comprehensive Cancer Network, Vol. 14, 2016, pp. 1213-24.
Google Scholar Crossref - Bruins, Harman M., et al. "Long‐term outcomes of salvage radical cystectomy for recurrent urothelial carcinoma of the bladder following partial cystectomy." BJU International, Vol. 111, No. 3b, 2013, pp. E37-E42.
Google Scholar Crossref