Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 12
Assessing the Efficacy of Low Cost Indigenously Produced Soya Based Ready to Use Therapeutic Food with Standard Indigenously Produced Peanut Based Ready to Use Therapeutic Food
Lavina Fernandes*, Alka Rajendra Jadhav, Prachi Karnik, Blossom Rodrigues, Divya Ananthasubramanian and Annapurna KoliIndia
Lavina Fernandes, Nutrition Rehabilitation, Research and Training Centre, Department of Pediatrics, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India, Email: lavinaa.fernandes@gmail.com
Received: 23-Nov-2020 Accepted Date: Dec 21, 2020 ; Published: 28-Dec-2020
Abstract
Background: Ready-to-Use Therapeutic Food (RUTF) is considered a gold standard in management of Severely Acute Malnourished (SAM) children. Its use is limited in resource poor settings due to cost constraint. We prepared Soya based RUTF costing 25% less using WHO recommendations. Objective: To compare efficacy between soya based RUTF named as Soya-Medical Nutrition Therapy (S-MNT) and standard Peanut based RUTF named as Peanut-Medical Nutrition Therapy (P-MNT) in treatment of SAM. Methods: This open randomized controlled trial enrolled children between (6-60) months, diagnosed as SAM by WHO criteria. Subjects were divided into two groups that received S-MNT or P-MNT for 12 weeks. Main outcome measures were rate of weight gain (g/kg/day) and change in nutritional status. Result: Of 125 SAM children enrolled, 78 completed 12 weeks of intervention. At week 2, rate of weight gain in P-MNT was 2.8 g/kg/day and S-MNT was 2.43 g/kg/day (p=0.662). At 12 weeks, it was 0.75 g/kg/day in P-MNT and 0.87 g/kg/day in S-MNT (p=0.821). The mean rate of weight gain in P-MNT group was 2.49 g/kg/day while in S-MNT group was 1.78 g/kg/day which were statistically not significant. 75% subjects recovered from SAM in S-MNT while 89.13% in P-MNT (p=0.496). Pre and Post mean weight in both the groups were significant (p<0.001). 25% subjects had less than 30% consumption of S-MNT compared to 13.04% in P-MNT group. Conclusion: S-MNT was found to be as efficacious as P-MNT and hence can be a good alternative in SAM management. Soya based RUTF reduces cost of therapy without compromising the nutritional quality of RUTF.
Keywords
Malnutrition, Severe acute malnutrition, Undernutrition
Introduction
In spite of various measures, malnutrition still persists as a major public health challenge. Severe Acute Malnutrition (SAM) is a life-threatening condition. It is characterized by a rapid deterioration in nutritional status over a short period of time. Children suffering from SAM have weakened immunity, increasing their risk of death due to greater frequency and severity of common infection. Severe Acute Malnutrition (SAM) is a major cause of death in children under 5, and its prevention and treatment are critical to child survival and development. In 2018, 17 million were SAM globally of which more than half lived in South Asia [1,2]. South Asia’s wasting prevalence of 15.2% represents a situation requiring a serious need for intervention with appropriate treatment programs. According to National Family Health Survey- 4, 7.5% of Indian children under 5 and 9.4% in Maharashtra are SAM [3].
A SAM child cannot consume large volumes of locally available foods due to decreased appetite and physiological changes in the gastrointestinal tract, hence making it additionally difficult to eat the desired quantity as per their nutritional requirement. Ready to Use Therapeutic Foods (RUTF) has been well documented in reducing case-fatalities among SAM children and have been used widely in Community based Management of Acute Malnutrition programs (CMAM) [4]. The use of RUTF in the acute phase of malnutrition rehabilitation is recommended with a therapeutic intention and not as food. The cost of RUTF is still considered a significant barrier in programs dealing with management of SAM. The constant efforts to reduce the cost of therapy are on-going. The most commonly used RUTF which is indigenously produced and named as P-MNT in this trial is a mixture of peanut paste, milk powder, sugar, vegetable oil, vitamins, minerals and emulsifier [5,6]. P-MNT has demonstrated a high rate of recovery and weight gain in a trial previously conducted at our centre [7]. However, the peanut paste in P-MNT is very expensive for sustainable use in a resource limited setting. Soyabean is rampantly grown in India. Soybean by-products like Processed Soya flour is a cheaper alternative to peanut paste. It is a source of complete protein (51.46%) with a good biological value (72.8%) [8,9]. Malnourished children often suffer from diarrheal illnesses, soybean can also be used in such cases.
Soya based RUTF (S-MNT) reduces cost without much compromising the nutritional quality of RUTF. However, no research studies document the effect of Soya Based RUTF on Severe Acute Malnutrition (SAM). Thereby this study was conceptualized to compare the impact of S- MNT and P-MNT in SAM children.
Methods
Study Design
This research aimed to develop a Soya based RUTF (S-MNT) and compare it with standard Peanut based RUTF (PMNT). We hypothesized that S-MNT would not be inferior to the P-MNT with regard to recovery rate and rate of weight gain and can be used in management of SAM as an alternative to P-MNT. The trial was registered at Clinical Trials Registry-India [CTRI/2018/02/012171] and approved by the Staff Research Society Ethics committee of the LTM Medical College, Mumbai.
Study Population
Study participants were selected from children referred to OPD and/or admitted at Nutrition Rehabilitation, Research and Training Centre (NRRTC) situated at Urban Health Centre, Dharavi associated with Lokmanya Tilak Municipal Medical College and General Hospital, and a tertiary care hospital situated in Mumbai, India. NRRTC enrolled all children aged (6-59) months who were diagnosed with SAM as per WHO criteria, which was defined as MUAC <115 mm or Weight for height Z score <-3 SD or presence of bilateral pitting edema of nutrition origin [10]. Children with any medical complication at enrollment or inability to consume food orally or children already on any nutritional supplement were excluded from the study. Children with congenital or acquired disorder affecting growth, presence of any food allergy or intolerance or a history of treatment of SAM in the previous 3 months were also excluded.
All subjects were examined by Medical officer to confirm the diagnosis of SAM and check for any present medical complications. Medical complications were defined using the WHO CMAM and Integrated management of childhood illness standard definition [11,12]. Subjects compliant towards the inclusion criteria were randomly assigned to receive either S-MNT or P-MNT. Weight, height/length and MUAC were measured and interpreted following WHO recommended procedures [13]. Randomization was performed using a computer generated sequentially numbered randomization list. The ingredients used for preparing Soya based RUTF (S-MNT) are Defatted soya flour, skimmed milk powder, oil, sugar, emulsifier and micronutrient premix compared to Peanut based RUTF (P-MNT) where soya flour is replaced with peanut paste. Sensory evaluation on both the products was done using hedonic scale on normal children aged 4 to 10 years old. Table 1 shows detailed nutrient composition of S-MNT and P-MNT. Both S-MNT and P-MNT meet the WHO 2007 recommendations for formulating a ready to use therapeutic food [14]. The children in both the group were administered MNT in a dose of 175 kcal/kg/day of the present body weight for period of twelve weeks. Anthropometric indices and proportion of MNT intake was monitored weekly.
| Component | WHO recommendations | Unit | S-MNT | P-MNT |
|---|---|---|---|---|
| Energy | 520-550 | kcal | 547.75 | 560 |
| Protein | 13-16.5 (10%-12 % of total energy ) | g | 14.62 | 14.6 |
| Carbohydrate | 41-58 | g | 45.03 | 49 |
| Fat | 26-36.6 (45%-60% of total energy) | g | 31.05 | 34.5 |
| Sodium | <290 | mg | 193.04 | 135 |
| Potassium | 1100-1400 | mg | 1320.1 | 1220 |
| Calcium | 300-600 | mg | 628.93 | 578 |
| Phosphorous | 300-600 | mg | 521.11 | 288 |
| Magnesium | 80-140 | mg | 105.2 | 84 |
| Iron | 10-14 | mg | 14.24 | 12 |
| Zinc | 11-14 | mg | 13.24 | 12 |
| Copper | 1.4-1.8 | mg | 1.51 | 1.5 |
| Selenium | 20-40 | mcg | 24.2 | 20 |
| Iodine | 70-140 | mcg | 89.24 | 80 |
| Vitamin A | 0.8-1.2 | mg | 1.14 | 1.1 |
| Vitamin D | 15-20 | mcg | 18.26 | 17.1 |
| Vitamin E | >20 | mg | 25.6 | 20.6 |
| Vitamin K | 15-30 | mcg | 24.98 | 21 |
| Vitamin C | >50 | mg | 60.17 | 53 |
| Vitamin B1 | >0.5 | mg | 0.92 | 0.6 |
| Vitamin B2 | >1.6 | mg | 2.69 | 1.9 |
| Vitamin B6 | >0.6 | mg | 0.78 | 0.6 |
| Vitamin B12 | >1.6 | mcg | 1.79 | 1.76 |
| Vitamin B9 | >200 | mcg | 253.01 | 210 |
| Vitamin B3 | >5 | mg | 9.24 | 5.31 |
| Vitamin B5 | >3 | mg | 3.25 | 3.1 |
| Vitamin B7 | >60 | mcg | 68.01 | 66 |
| n-6 fatty acid | 3%-10% of total energy | % | 3 | 5.01 |
| n-3 fatty acid | 0.3%-2.5% of total energy | % | 0.31 | 0.5 |
Table 1: Nutritional composition of S-MNT and P-MNT
Statistical Analysis
The data obtained from all patients were filled in predesigned Proforma and then tabulated on MS Excel program. All observations were analyzed using SPSS software. We used the t test for paired or unpaired data to compare between two groups of quantitative data and student’s chi-square test to compare proportions.
Results
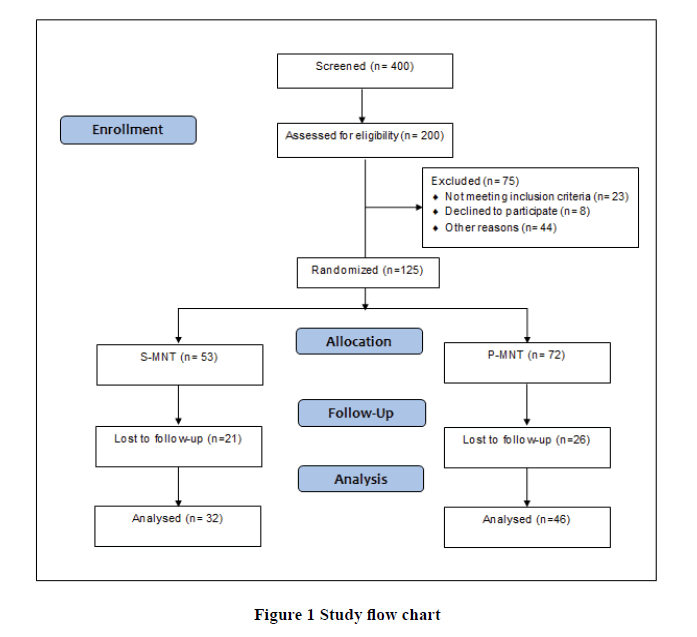
The details of enrollment and movement of subjects from screening to data analysis are depicted in Figure 1. Baseline characteristics of children enrolled in each study group are shown in Table 2. A total of 400 children were screened and 200 subjects were diagnosed with SAM. 75 were excluded because they did not meet the study inclusion criteria. 125 children were enrolled and randomized. At the end of the study, 78 children remained for follow-up, from which 32 received S-MNT and 46 received P-MNT. The mean weight in P-MNT group increased from 7.2 kg at baseline to 8.59 kg and 8.72 kg at 8 weeks and 12 weeks respectively (Table 3). The mean weight in S-MNT group on enrollment was 6.92 kg and at the end of the study 7.98 kg and 7.74 kg at 8weeks and 12 weeks respectively which was found to be highly significant (p<0.001).
| Participants (n) | S-MNT | P-MNT |
| 32 | 46 | |
| Age Group | ||
| 6-12 months (n, %) | 16 (30.19%) | 21 (29.17%) |
| 1-3 years (n, %) | 30 (56.6%) | 33 (45.83%) |
| 3-5 years (n, %) | 7 (13.21%) | 18 (25%) |
| Male sex (n, %) | 21 (39.62%) | 31 (43.06%) |
| Anthropometry | ||
| Weight, kg | 6.92 ± 2.05 | 7.20 ± 1.87 |
| Height, cm | 72.56 ± 11.33 | 75.23 ± 10.87 |
| Midupper arm circumference, cm | 11.50 ± 1.16 | 11.65 ± 0.99 |
Table 2: Baseline characteristics of children enrolled in the trial
| Mean Weight | Rate of Weight Gain | ||||
|---|---|---|---|---|---|
| S-MNT | P-MNT | S-MNT | P-MNT |
p-value |
|
| On enrollment | 6.92 (2.06) | 7.20 (1.87) | |||
| Week 1 | 6.96 (2.05) | 7.39 (1.96) | 2.67 (5.56) | 2.34 (5.39) | 0.749* |
| Week 2 | 7.18 (1.88) | 7.49 (1.93) | 2.42 (4.53) | 2.8 (4.01) | 0.662* |
| Week 3 | 7.02 (1.94) | 8.03 (1.95) | 2.1 (4.61) | 3.19 (4.73) | 0.357* |
| Week 4 | 6.99 (1.95) | 8.10 (2.00) | 1.08 (4.92) | 3 (4.26) | 0.102* |
| Week 5 | 7.07 (1.98) | 8.27 (1.88) | 1.87 (3.6) | 2.81 (3.98) | 0.373* |
| Week 6 | 7.12 (1.97) | 8.24 (2.06) | 1.48 (3.87) | 3.04 (3.32) | 0.164* |
| Week 7 | 7.81 (2.30) | 8.23 (2.05) | 2.33 (3.41) | 2.18 (5.17) | 0.911* |
| Week 8 | 7.98 (1.92) | 8.59 (2.08) | 1.21 (3.69) | 2.32 (4.46) | 0.45* |
| Week 12 | 7.74 (1.98) | 8.72 (2.05) | 0.87 (1.7) | 0.75 (1.77) | 0.821* |
Table 3: Mean Weight Gain (kg) and Rate of Weight Gain (gm/kg/day)
The rate of weight gain was found to be highest in the initial two weeks in S-MNT group i.e. 2.67 g/kg/day in week 1 and 2.42 g/kg/day in week 2. At week 12, the rate of weight was lowest in both the group i.e. 0.87 g/kg/day in S-MNT and 0.75g/kg/day in P-MNT. The mean rate of weight gain was found to be higher in P-MNT (2.49 g/kg/day) than SMNT (1.78 g/kg/day). On comparison, the rate of weight gain between both groups was found to be comparable and statistically insignificant (Table 3).
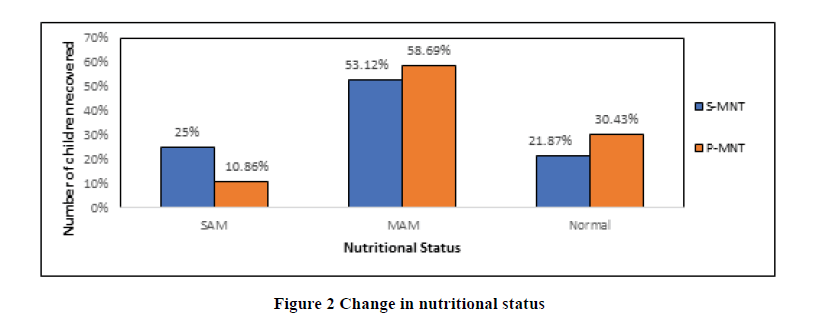
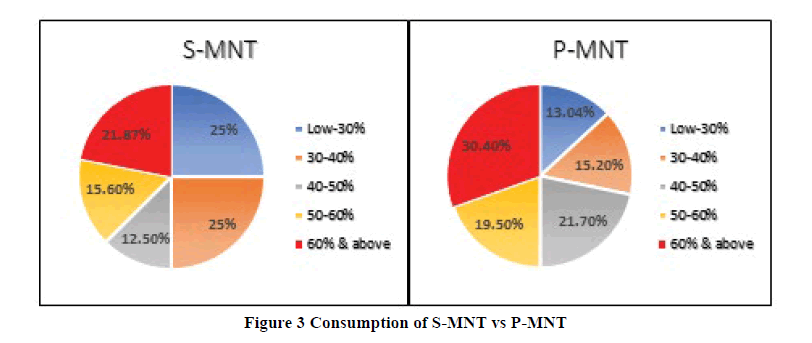
At the end of treatment, 75% had recovered (i.e. WHZ> -2SD and MUAC>115 mm) in S-MNT group compared to 89.13% in P-MNT group (p=0.496) (Figure 2). In the Figure 3, we can see that 37.47% consumed more than 50% in S-MNT compared to 49.90 % in P-MNT. Overall, the p-value was comparable but P-MNT was more acceptable than S-MNT.
Currently there are no studies available with composition similar to S-MNT. The mean rate of weight gain in P-MNT group and in S-MNT group during intervention was comparable to study done by Ciliberto et al., (2.8 g/kg/d) [15]. Other studies like Diop et al., (15.6 g/kg/d), Manary et al., (7 g/kg/d) and Thakur et al., (9.5 g/kg/d) showed a better rate of weight gain with Peanut based RUTF in comparison to the results found in our study [16-18]. The mean weight difference between S-MNT and P-MNT group at the end of the study was not significant (p-value=0.13) thus indicating that the evidence supported the hypothesis.
A higher rate of weight gain was observed in the initial weeks in the S-MNT. Compliance in both the groups was comparable and not satisfactory; therefore, the overall rate of weight gain was less in both the groups. The compliance was found to be unsatisfactory because most of the subjects belonged to lower income group and couldn’t afford to bear the travelling expenses to visit the hospital. An observation was made that when the nutritional status of the subjects fairly improved, adherence to the treatment plan decreased and default rate increased.
This study has an important practical application. High cost is one of the major reasons of not using RUTF for management of SAM and resulting into reducing the coverage and sustainability of SAM treatment program. In addition, locally produced RUTF will contribute towards strengthening local food manufacturing or improving local agricultural market, both of which are important in prevention of malnutrition.
Removing peanut from the RUTF recipe also confers several advantages. Peanuts are more prone to contamination by aflatoxins thus increasing the cost of quality assurance adding to final cost of the product. This increase in the cost reduces the ease at which such products can be produced indigenously in countries that require them [19,20]. The raw material cost in our small-scale indigenous production unit per cup (92 gm) of P-MNT and S-MNT is Rs. 20 and Rs. 15 respectively. This reduction of 25% in the cost can be further increased in a large scale set-up. Additionally, although incidences of Peanut allergy is less common in low income countries, a rising trend is being observed which may affect the programs treating SAM [21,22].
Limitations of our study were: (i) Small sample size (ii) Children were not supervised daily for consumption of MNT in both groups; (iii) The default rate was high.
Conclusion
SAM children need safe, palatable foods with macronutrients and micronutrients tailored to their needs in order to recover. Many studies around the world have shown that providing RUTF successfully supports early recovery of SAM children. Our study demonstrated that the new soya-based formulation is comparable to peanut based with respect to rate of weight gain and recovery rate. It is a cheaper alternative. It can be used as an alternative RUTF in resource poor setting and clinical medical condition like peanut allergy.
Declerations
Acknowledgement
1) Dean, LTMGH.
2) Head of Department, Dept. of Pediatrics, LTMGH.
3) Dr. Bharat Parekh, Toddler Food Partners.
4) Dr. Shivram Murty, Toddler Food Partners.
5) Dr. Narendra Shah, CTARA, IIT Bombay
Funding Source:
1) Toddler Food Partners, USA
2) TATA Motors Private Limited
Conflict Of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- United Nations Children's Fund, Malnutrition in Children-UNICEF DATA, 2020. https://data.unicef.org/topic/nutrition/malnutrition/
- Collins, Steve, et al. "Management of severe acute malnutrition in children." The Lancet, Vol. 368, No. 9551, 2006, pp. 1992-2000.
- 2015-2016 National Family Health Survey (NFHS-4). Ministry of Health and Family Welfare, Government of India. April, 2019. http://rchiips.org/nfhs/nfhs-4Reports/India.pdf
- UNICEF. "Ready-to-use therapeutic food for children with severe acute malnutrition." Position paper. Available at: https://www. unicef. org/media/files/Position_Paper_Ready-to-use_therapeutic_food_for_children_with_severe_acute_malnutrition__June_2013. Pdf, 2013.
- Briend, André, et al. "Ready-to-use therapeutic food for treatment of marasmus." The Lancet, Vol. 353, No. 9166, 1999, pp. 1767-8.
- Manary, Mark J. "Local production and provision of ready-to-use therapeutic food (RUTF) spread for the treatment of severe childhood malnutrition." Food and Nutrition Bulletin, Vol. 27, No. 3_suppl3, 2006, pp. S83-S9.
- Jadhav, Alka, et al. "A Randomized controlled facility based trial to assess the impact of indigenously prepared Ready To Use Therapeutic Food (RUTF) for children with severe acute malnutrition in India." Pediatric Oncall, Vol. 13, No. 4, 2016, pp. 93-8.
- Food data central, Agricultural Research Service. USDA. Oct. 2019. https://fdc.nal.usda.gov/fdc-app.html#/food-details/174275/nutrients.
- Food and Agriculture Organization. Food Policy and Food Science Service. Amino-acid content of foods and biological data on proteins: Teneur Des Aliments en Acides Aminés Et Données Biologiques Sur Les ProtéinesTeneur Des Aliments en Acides Aminés Et Données Biologiques Sur Les Protéines. 1970.
- World Health Organization. "WHO child growth standards and the identification of severe acute malnutrition in infants and children: joint statement by the World Health Organization and the United Nations Children's Fund." 2009.
- Nicoll, Angus. "Integrated management of childhood illness in resource-poor countries: an initiative from the World Health Organization." Transactions of the Royal Society of Tropical Medicine and Hygiene, Vol. 94, No. 1, 2000, pp. 9-11.
- World Health Organization. Guideline: updates on the management of severe acute malnutrition in infants and children. World Health Organization, 2013.
- World Health Organization. "Training course on child growth assessment." Geneva: WHO, 2008, pp. 17-25.
- World Health Organization and UNICEF. "Community-based management of severe acute malnutrition: a joint statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children's Fund." 2007.
- Ciliberto, Michael A., et al. "Home-based therapy for oedematous malnutrition with ready-to-use therapeutic food." Acta Paediatrica, Vol. 95, No. 8, 2006, pp. 1012-5.
- Diop, El Hadji Issakha, et al. "Comparison of the efficacy of a solid ready-to-use food and a liquid, milk-based diet for the rehabilitation of severely malnourished children: a randomized trial." The American Journal of Clinical Nutrition, Vol. 78, No. 2, 2003, pp. 302-7.
- Manary, Mark J., et al. "Home based therapy for severe malnutrition with ready-to-use food." Archives of Disease in Childhood, Vol. 89, No. 6, 2004, pp. 557-61.
- Thakur, Govind Singh, H. P. Singh, and Chhavi Patel. "Locally-prepared ready-to-use therapeutic food for children with severe acute malnutrition: a controlled trial." Indian Pediatrics, Vol. 50, No. 3, 2013, pp. 295-9.
- Khlangwiset, Pornsri, and Felicia Wu. "Costs and efficacy of public health interventions to reduce aflatoxin-induced human disease." Food Additives and Contaminants, Vol. 27, No. 7, 2010, pp. 998-1014.
- Khlangwiset, Pornsri, Gordon S. Shephard, and Felicia Wu. "Aflatoxins and growth impairment: a review." Critical Reviews in Toxicology, Vol. 41, No. 9, 2011, pp. 740-55.
- Yang, Zhenyu. "Are peanut allergies a concern for using peanut-based formulated foods in developing countries?." Food and Nutrition Bulletin, Vol. 31, No. 2_suppl2, 2010, pp. S147-S53.
- Prescott, Susan L., et al. "A global survey of changing patterns of food allergy burden in children." World Allergy Organization Journal, Vol. 6, No. 1, 2013, pp. 1-12.