Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
An Insight into Donor Blood Unit’s Wastage in a Hospited Blood Bank from Pakistan
Sadia Sultan1*, Samar Abbas Jaffri2, Syed Muhammad Irfan3, Syed Muhammad Usman4, Sheeza Nadeem4, Usman Waheed5 and Hasan Abbas Zaheer52Department of Medicine, Liaquat National Hospital and Medical College, Karachi, Pakistan
3Department of Hematology and Blood Bank, Liaquat National Hospital and Medical College, Karachi, Pakistan
4Department of Medicine, Jinnah Medical and Dental College, Karachi, Pakistan
5Safe Blood Transfusion Program, Government of Pakistan, Pakistan
Sadia Sultan, Laboratory services, Consultant Hematologist, National Medical Centre, Karachi, Pakistan, Tel: 3186624636, Email: sadiasultan96@yahoo.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Objective: Blood supplies in developing countries are often limited and blood wastage in low socio-economic countries usually led to a very serious consequence. Therefore, we analyzed the wastage of blood products amid limited supply to identify areas where apposite intervention could be employed to avoid such wastage. Methods: A cross-sectional study was conducted on the wastage of blood products during the years 2015-2016 at our tertiary care hospital. Donor’s demographical data includes name, age, gender; contact number, and type of donor (replacement or voluntary) were recorded on a structured questionnaire. All donors were selected according to established inclusion criteria considering age (≥ 18 years), body weight (≥ 50 g/dL), hemoglobin levels (≥ 12.5 g/dl), various reasons for the blood wastage were noted and recorded. The data were analyzed using IBM statistics SPSS version 22 (IBM Corp., Armonk, NY). Results: A total of 33,456 bags of blood were collected during the study period, each was segregated into three components, with a total of 10,0368 units. Data indicated that 10977 units (10.9%) of blood components were wasted. 5643 (5.6%) units were discarded due to Transfusion Transmitted Infections (TTI), remaining 5334 (5.3%) due to miscellaneous reasons. In reactive units, Hepatitis C, Hepatitis B, Syphilis, and HIV reactivity rates were found to be 2.1%, 1.6%, 1.7%, and 0.09% respectively. Of the miscellaneous reasons, 4574(4.5%) units of platelet concentrates were discarded; of which 3750 (3.7%) were expired, 767 (0.7%) due to red cell contamination, and 57 (0.05%) due to lipemic appearance. For packed red cells, 726 (0.7%) units were wasted due to stock time expiry and 24 (0.02%) wasted due to hemolysis. Only 10 (0.009%) units of fresh frozen plasma were wasted due to ruptured units. Conclusions: The blood wastage rate is low as compared to other developing countries and appears high in comparison with the developed world. An appropriate inventory management structure along with the training and regular staff competency testing is necessary to ensure optimum utilization and minimize wastage.
Keywords
Blood products, Blood wastage, Expired blooda
Introduction
Blood transfusion plays an indispensable role in the health care system. In developing countries, the demands for blood exceed than blood supply. As per World Health Organization (WHO) statistics, more than 70% of developing nations collect less than half of the blood required to meet their requirements [1]. Therefore, blood services face the overwhelming challenge of making ample supplies of blood products, as well as ensuring the safety of these products.
Blood banks have a major responsibility to ensure a regular supply of blood, but donor dearth and concomitant wastage are major issues in blood availability. According to WHO data, the blood wastage is accredited to poor inventory management, deprived manufacturing practices, inadequate storage, and shipment. It is anticipated that blood wastage is responsible for the loss of five million blood units annually [2,3]. Dropping the rate of blood wastage through proper stock management and optimal blood utilization practice may overcome the impact of low blood donations.
Today in developed countries, the blood wastage rate is reported to be between 0.1% and 6.7% [4]. However, there is limited information available on blood wastage in Asian countries including Pakistan. Blood wastage monitoring is not a priority in the majority of blood banks in Pakistan because of other overwhelming problems such as suboptimal standards, inadequate screening practices, blood-borne infection, and low blood donation rate [5].
Efforts focused to monitor the likelihood of blood wastage could yield benefits when addressed in the setting of resource-limited countries. Blood transfusion services, by identifying the causes of wastage and applying preventive measures, have significantly reduced the wastage rate from 4% to less than 1% [6]. Therefore, this study is carried out to investigate the prevalence of blood wastage in the setting of a limited supply of blood units and identify areas where appropriate preventive intervention could be applied to prevent such blood wastage.
Materials and Methods
Setting
This prospective cross-sectional study, extended from January 2015 to December 2016, was conducted at the Liaquat National Hospital and Medical College, Pakistan, which is around a 700-bed tertiary care teaching institute. Our blood bank comprises well-trained skilled technicians, experienced faculty, and state-of-the-art equipment. Whole blood units are fractionated into components in 100% of units collected.
Donor’s demographical data includes name, age, gender; contact number, and type of donor (replacement or voluntary) were recorded on a structured questionnaire. All donors were selected according to established inclusion criteria considering age (≥ 18 years), body weight (≥ 50 g/dL), hemoglobin levels (≥ 12.5 g/dl), hematocrit levels (PCV) ≥ 38%, pulse rate (50-100 beats/min) with normal blood pressure.
Donors with high-risk behavior, having a history of jaundice, intravenous drug abuse, non-marital sexual contacts, tattooing, and recent blood transfusion or recent surgery were deferred and excluded from the study. Written consent was obtained from all the qualifying donors.
Data for the last 2 years were collected from the maintained departmental database. Data regarding blood donation, discard of blood components and the reason to discard blood were collected.
The Institutional clearance from the ethical and research committee of the Hospital was taken before the study.
The data collected was recorded on a Microsoft spreadsheet and later statistical analysis was carried out using IBM statistics SPSS version 22 (IBM Corp., Armonk, NY). For quantitative variables, results were reported as the mean (± SD). Frequency and percentages were calculated for categorical variables.
Results
A total of 33456 blood donors were donated over 2 years. Amongst them, 33270 (99.4%) were replacement donors and 186 (0.5%) were voluntary blood donors with a mean age of 28.09 ± 9.04 years. Blood donors comprised of 33360 (99.7%) males and 96 (0.2%) females.
A total of 33,456 bags of blood were collected during the study period. Each blood bag was segregated into three components, with a total of 10,0368 units (33,456 each for packed red cell, platelets concentrate, and fresh frozen plasma). Data indicated that 10977 units (10.9%) of blood components were wasted due to various reasons; 5643 (5.6%) units wasted due to Transfusion Transmitted Infections (TTI), remaining 5334 (5.3%) due to miscellaneous reasons. In reactive (TTI ) units, Hepatitis C , Hepatitis B, Syphilis and HIV reactivity rates were found to be 2.1% (n=2121), 1.6% (n=1686), 1.7% (n=1737) and 0.09% (n=99) respectively.
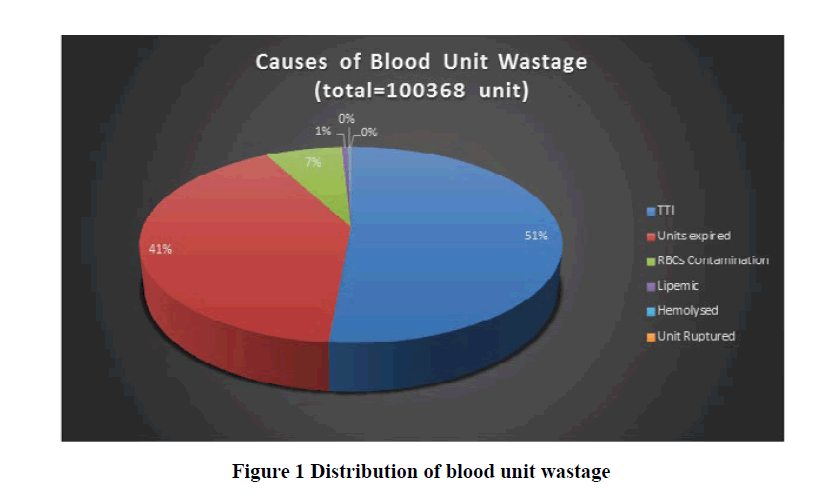
For miscellaneous reasons, 5334 (5.3%) units were discarded. 4574 (4.5%) units of platelet concentrates were discarded of which 3750 (3.7%) were expired, 767 (0.7%) due to red cell contamination, and 57 (0.05%) due to lipemic appearance. For packed red cells, 726 (0.7%) units were wasted due to stock time expiry and 24 (0.02%) wasted due to hemolysis. Lastly only 10 (0.009%) units of fresh frozen plasma were wasted due to ruptured units (Figure 1).
Discussion
According to WHO facts, the donation rate is 32.1 donations in high-income countries and only 4.6 donations in lowincome countries per 1000 citizens [7]. The current status in developing countries is alarming due to the limited rate of blood donation with simultaneous increases in blood usage every year. The situation is furthermore complicated due to concomitant blood wastage due to various distinct reasons.
The present study attempts to analyze the rate of blood wastage at a tertiary health care center during the period 2015-2016 in Pakistan. An insight on blood wastage frequency helps to design an outline or measures to prevent such wastage prospectively. To the best of our knowledge, this is the first comprehensive report from our part of the world. No local data is available for comparison. However, the reported blood wastage rate is highly variable from 0.1% to 25% in various regional and international studies. In this study, we observed that over 2 year period, the blood wastage rate was 10.9%. It showed that blood product wastes were highly linked with 3 common causes; transfusiontransmitted infections expired blood products and red cell contamination. Results showed that the wastage rates were high in platelet concentrates (4.5%), followed by packed red cells and plasma according to the type of blood products. Furthermore, there is a very low prevalence of female donors. It is due to the general perception in Pakistani society that females already carry a high social burden of families so they should not be consulted for blood donation. Now the blood donation societies are visited by the girl’s college to encourage the female to step forward for the blood donation.
Published data from neighbor India reported the blood discard rate as variable from 0.6% and 14.6% [8]. Our results are intermediary as compared with Indian studies. In another study reported from Iran, out of a total of 30913 units of collected blood, 3048 (9.8%) units were discarded [9]. When compared our results with the report from Uganda, the blood wastage rate is very high, as surprisingly blood wastage was zero in Uganda [10]. A blood center in Malaysia reported 2.3% of blood units wasted and the main reasons for wastage were due to technical consideration [11]. Similarly, Beckwith, et al. recorded a 3.0% of wastage rate in the blood bank of the United Kingdom [12]. This low rate of blood wastage could be attributed to continued follow-ups, monthly meetings with staff and their retraining, strong blood inventory management considering the ratio of waste to usage, and an important regular blood wastage audits being effective in reducing such wastage.
Another recent study from the Netherlands determined the blood units’ wastage rate of 7.5% which was decreased to 1% of the units dispensed, after implementation of the various preventive strategies [13]. In contrast to our findings, one recent study from Guyana reported a very high rate of blood units wasted accountable in 25.4% of units collected in their blood bank, this high rate of wastage was attributed to various reasons includes expired blood units, broken seals, and broken cold chain [14].
Our data indicated that the wastage rate is highest in platelet concentrates accredited to its shortest expiry. In one Malaysian study, the author also concluded the highest rate of wastage in platelets component; 3909 (6.0%) platelets out of a total of 390636 units were wasted due to red cell contamination [11]. Saluja, et al. encountered a wastage rate of 20.8% in platelets due to non-utilization (expired) during the storage period [15]. This higher rate was attributed to non-acceptance by physicians in transfusing ABO incompatible platelets and secondly to shortage shelf life up to 3 days in their study [15]. One large-scale study conducted in 17 blood centers in 10 European countries, reported the mean platelet discard rates between 6.7% and 25% in three years duration with the mean discard rates remains at 13% annually [16].
The main reason for the discard of blood units in our study was seropositivity for transfusion-transmitted infections. When compared this finding with the studies from India and Nigeria outcome was similar [11,17]. This higher prevalence in donors is alarming and is likely to adversely affect the donation pool in long term. Stringent donor selection and deferral criteria, promoting voluntary donation and cautious donor screening are suggested to ensure maximum blood safety.
Blood inventory management is both demanding and critical; to ensure enough timely availability of each product at the same time to diminish its wastage. In our blood bank, we maintained our inventory depending upon our outcome/ demand. Taking into account our main limitation is lacking online blood bank software. The online blood bank management software systems are specially designed for the process, storage, analysis, and retrieval of information related to blood inventory and administration.
Lastly, 57 units were wasted because of gross lipemic appearance, which is usually seen in a donor who donated after eating high fatty meals. In the UK, such blood donations are not utilized for issuance [18]. However, lipaemia does not affect the product safety but might interfere in the serological results for viral marker testing, so it seems worth effective to discard those lipemic units, which we did [19,20].
Conclusion
TTI and expired blood remain major causes of blood wastage in our hands. We recommend reviewing policies for blood management and the reduction of blood wastes. This would require technical supervision of blood product making, incorporating blood bank management software for inventory, and regular blood wastage audits for effective reduction of product wastage.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgments
The authors are thankful to all the doctors and staff members of the Blood Bank Division of Liaquat National Hospital and Medical College, Karachi for their support during the study. The authors are also thankful to Dr. Ali Yasir (The Searle Company Limited) for the assistance in manuscript submission and publication.
References
- World Health Organization. "Availability, safety and quality of blood products. Report by the Secretariat." Sixty-Third World Health Assembly A 63, 2009. https://apps.who.int/iris/bitstream/handle/10665/2389/A63_20-en.pdf?sequence=1&isAllowed=y
- World Health Organization. "Availability, safety and quality of blood products. Executive Board." EB125/5, 2009. https://apps.who.int/gb/archive/pdf_files/EB125/B125_5-en.pdf
- Clark, J. A., and M. M. Ayoub. "Blood and component wastage report: A quality assurance function of the hospital transfusion committee." Transfusion, Vol. 29, No. 2, 1989, pp. 139-42.
- Heitmiller, Eugenie S., et al. "Blood wastage reduction using Lean Sigma methodology." Transfusion, Vol. 50, No. 9, 2010, pp. 1887-96.
- Sultan, Sadia, et al. "Trends of venereal infections among healthy blood donors at Karachi." Archives of Iranian Medicine, Vol. 19, No. 3, 2016, pp. 192-96.
- Zoric, Lana, et al. "Blood wastage reduction: A 10-year observational evaluation in a large teaching institution in France." European Journal of Anaesthesiology (EJA), Vol. 30, No. 5, 2013, pp. 250-55.
- World Health Organization. "Blood safety and availability. Fact sheet." 2020. https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability
- Kumar, Alok, et al. "Analysis of reasons for discarding blood and blood components in a blood bank of tertiary care hospital in central India: A prospective study." International Journal of Medicine and Public Health, Vol. 4, No. 1, 2014, pp. 72-74.
- Far, Rafat Mohebbi, et al. "Determination of rate and causes of wastage of blood and blood products in Iranian hospitals." Turkish Journal of Hematology, Vol. 31, No. 2, 2014, pp. 161-67.
- Natukunda, B., H. Schonewille, and C. Th Smit Sibinga. "Assessment of the clinical transfusion practice at a regional referral hospital in Uganda." Transfusion Medicine, Vol. 20, No. 3, 2010, pp. 134-39.
- Morish, Mohammed, et al. "Quality indicators for discarding blood in the National Blood Center, Kuala Lumpur." Asian Journal of Transfusion Science, Vol. 6, No. 1, 2012, pp. 19-23.
- Beckwith, Hannah, et al. "A review of blood product usage in a large emergency department over a one-year period." Emergency Medicine Journal, Vol. 27, No. 6, 2010, pp. 439-42.
- Bots, M., et al. "Strategies to reduce wastage of red blood cell units." Vox Sanguinis, Vol. 110, No. 2, 2016, pp. 143-49.
- Kurup, Rajini, et al. "A study on blood product usage and wastage at the public hospital, Guyana." BMC Research Notes, Vol. 9, No. 1, 2016, pp. 1-6.
- Saluja, K., et al. "Platelet audit: Assessment and utilization of this precious resource from a tertiary care hospital." Asian Journal of Transfusion Science, Vol. 1, No. 1, 2007, pp. 8-11.
- Veihola, Marketta, et al. "Variation of platelet production and discard rates in 17 blood centers representing 10 European countries from 2000 to 2002." Transfusion, Vol. 46, No. 6, 2006, pp. 991-95.
- Atinuke, Fasola Foluke, Shokunbi Wuraola Adebola, and Kotila Taiwo Rachael. "Blood wastage rate in a Sub-Saharan African hospital based blood bank." International Blood Research & Reviews, Vol. 4, No. 4, 2015, pp. 1-6.
- Mbahi, Musa, Virgil Reddy, and Aida Narvios. "Milky platelet concentrate: A second look." Transfusion (Philadelphia, PA), Vol. 46, No. 6, 2006, p. 877.
- Canadian Blood Services. "Visual Assessment Guide." 2009, pp. 1-30. https://profedu.blood.ca/sites/msi/files/VAG_en.pdf
- American National Red Cross. "Visual Inspection Reference Guide." 2006, pp. 6-26.