Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 2
An Increasing Cancer Burden in Tertiary Care Health Centers of Chandigarh: The Hospital Based Study
Pandey A, Dimri K, Suraj*, Vias P, Kaur A and Rathee NDimri K, Suraj, Department of Radiation Oncology, Government Medical College and Hospital, Chandigarh, India, Email: surajbba87@gmail.com
Received: 30-Dec-2020 Accepted Date: Feb 11, 2021 ; Published: 18-Feb-2021
Abstract
The study emphasised the increasing cancer burden in tertiary care health centres of Chandigarh. The patients from neighbouring states were coming to UT (Union Territory of Chandigarh) for cancer-related treatment due to the unavailability of tertiary healthcare facilities. It was also observed that most of the patients were coming to Chandigarh in advance stage of cancer i.e. more than 57.54%. Various factors were influencing the increase in the burden of cancer in UT.
Material and Methods: The prospective study was conducted among registered cancer patients of Radiation Oncology and other departments in GMCH and PGIMER Chandigarh. Both primary and secondary data was used throughout the study.
Results: In the female, Ca Breast (37.15%) and in male, Ca Lip and Oral cavity (16.1%) were prevalent cancer. There were (30.83%) illiterate patients with a monthly average income of Rs.4608.27 and loss of average income due to cancer was Rs.119914.51. History of smoking was present in 25.60% of patients. Tobacco chewing (6.1%) and alcohol intake were present in 21.3% respectively. Around 41.5% of patients were non-vegetarian and the use of green vegetable was also very low. The use of junk food was very high (78.7%). Only 0.2% out of 30.7% of patients who were doing exercise, were doing it for adequate time.
Conclusion: Cancer is an increasing burden not only on hospitals but also on cancer patients as well as their families; treatment of Cancer is quite costly for average and BPL income group of families. Lifestyle factors may play a significant role in the causation of cancer. There is a definite degree of delay in the management of cancer, which can be reduced with further studies.
Keywords
Cancer burden, Expenditure, Lifestyle, Physical activity, Satisfaction
Introduction
Subjective tinnitus is the most common and manifest auditory symptom of an existing pathology in the auditory In the contemporary world, cancer is a very serious topic for discussion, which has its unforgettable impact (deaths, mental trauma, out of pocket expenditure, development of families, etc.) on an individual’s life as well as the families of survivals. Today no place remains untouched by cancer. Cancer is an upcoming problem of every country which may directly or indirectly increase the burden not only on the health care centres but also on the individual’s pocket, which may push back the family growth towards backwardness.
According to the WHO, ‘Chronic Diseases’ are the leading cause of death and disability among individuals globally. The four most prominent chronic diseases are as following; cardiovascular diseases, cancer, Chronic Obstructive Pulmonary Disease (COPD), and type-2 diabetes [1]. The term “Cancer” is (derived from the Greek word “Karkinos” for crab) literally defined as, an abnormal growth of cells which tend to proliferation of cell in an uncontrolled way and some cases, to the metastasize (spread) [2].
According to the Indian Council of Medical Research (ICMR), it is estimated that by the year 2020, 1.7 million new patients are going to be registered with a cancer diagnosis and more than 0.88 million deaths with such disease [3]. Chandigarh (UT) is an economically advanced city of India, characterized by rapid population growth due to the migratory population and changing lifestyle. Here the pattern of cancer often varies considerably as compared to the rest of the country. Many previous studies show that cancer patients from neighbouring states are coming to Chandigarh for cancer treatment due to a lack of tertiary care facilities at their native places. Chandigarh is equipped with good roads as well as train connectivity to reach up to tertiary health care facilities, also has the infrastructure to access the health care facilities in the term of curative and palliative care, cancer diagnostic techniques, trained health care professionals, etc. All these features related to cancer treatment attract the patients to have treatment at Chandigarh, due to the availability of tertiary healthcare facilities, such as the Post Graduate Institute of Medical Research and Education (PGIMER) and Government Medical College and Hospital (GMCH). Although, Government Medical College and Hospital (GMCH), is set in a developing and progressive phase, as far as equipment & facilities for cancer patients are concern. The patients from 7 (seven) neighbouring states, Haryana, Punjab, Himachal Pradesh, Uttar Pradesh, Uttarakhand and Bihar, are coming to Chandigarh for various treatments including ‘Cancer’ due to poor facilities available at their places. The lack of guidance and awareness mislead the patients to take the cancer-related treatment which may be resulted in delay at the primary, secondary and tertiary level.
Review of Literature
According to GLOBOCAN 2018, the new cancer cases detected in India, over the total population i.e. 135,40,51855 including both sexes (Males-70,15,46,980 and Females-65,25,04,878). The top 5 cancer sites oral cavity, lung, stomach, colo-rectum, and oesophagus were prevalent in the male population and among the female population breast, cervix uteri, ovary, oral cavity and colo-rectum cancers were most prevalent. In 2018, the 5,70,045 new cases (males) of cancer registered and the 5,87,249 (females) were recorded, the cumulative population of recorded cancer was 11,57,294 (11 million approx) new cancer cases. In 2018, the number of new cases of deaths due to cancer was recorded, i.e. Males-4,13,519 and Females-371302, the total deaths were recorded as approximately, 7,84,821. Table 1 represented the number of new cases in 2018, including both males and females; it showed the carcinoma breast (14.04%) was most prevalent amongst both genders other than top 5 cancers such are lip and oral cavity (10.37%), cervix uteri (8.37%), lung (5.86%) and stomach (4.96%). The females including all age groups, that the breast cancer was ranked 1st with 1,62,468 cases followed by cervix uteri 96,922, and Ovary 36,170. The males’ cases with lip and oral cavity cancer were on top in 2018 with 92,011 new cases, followed by lung 48,698, stomach 38,818 and colorectum 36,687 [4].
| S. No. | Cancer Site | ICD Code | New Cases | Deaths | ||||
|---|---|---|---|---|---|---|---|---|
| Number | Rank | % | Number | Rank | % | |||
| 1 | Breast | C50 | 162468 | 1 | 14 | 87090 | 1 | 11.1 |
| 2 | Lip, oral cavity | C00-C06 | 119992 | 2 | 10.4 | 72616 | 2 | 9.3 |
| 3 | Cervix uteri | C53 | 96922 | 3 | 8.4 | 60078 | 4 | 7.7 |
| 4 | Lung | C33-C34 | 67795 | 4 | 5.9 | 63475 | 3 | 8.1 |
| 5 | Stomach | C16 | 57394 | 5 | 5 | 51429 | 5 | 6.6 |
| 6 | Esophagus | C15 | 52396 | 6 | 4.5 | 46504 | 6 | 5.9 |
| 7 | Leukemia | C91-C95 | 42055 | 7 | 3.6 | 32471 | 7 | 4.1 |
| 8 | Ovary | C56 | 36170 | 8 | 3.1 | 24015 | 9 | 3.1 |
| 9 | Larynx | C32 | 28721 | 9 | 2.5 | 17640 | 15 | 2.2 |
| 10 | Brain, CNS | C70-C72 | 28142 | 10 | 2.4 | 24003 | 10 | 3.1 |
| 11 | Non-Hodgkin lymphoma | C82-C86 | 28110 | 11 | 2.4 | 23510 | 11 | 3.0 |
| 12 | Liver | C22 | 27670 | 12 | 2.4 | 25627 | 8 | 3.3 |
| 13 | Colon | C18 | 27605 | 13 | 2.4 | 19548 | 14 | 2.5 |
| 14 | Gallbladder | C23-C24 | 25999 | 14 | 2.2 | 19676 | 13 | 2.5 |
| 15 | Hypopharynx | C12-C13 | 25947 | 15 | 2.2 | 8804 | 22 | 1.1 |
| 16 | Prostate | C61 | 25696 | 16 | 2.2 | 17184 | 16 | 2.1 |
| 17 | Rectum | C19-C20 | 24251 | 17 | 2.1 | 20056 | 12 | 2.6 |
| 18 | Bladder | C67 | 18926 | 18 | 1.6 | 10231 | 19 | 1.3 |
| 19 | Thyroid | C73 | 18688 | 19 | 1.6 | 5128 | 25 | 0.65 |
| 20 | Oropharynx | C09-C10 | 17903 | 20 | 1.5 | 14953 | 17 | 1.90 |
| 21 | Kidney | C64-C65 | 15454 | 21 | 1.3 | 9911 | 20 | 1.30 |
| 22 | Corpus uteri | C54 | 13328 | 22 | 1.2 | 5010 | 27 | 0.64 |
| 23 | Multiple myeloma | C88-C90 | 12923 | 23 | 1.1 | 9900 | 21 | 1.30 |
| 24 | Pancreas | C25 | 10860 | 24 | 0.94 | 10528 | 18 | 1.30 |
| 25 | Penis | C60 | 9938 | 25 | 0.86 | 6930 | 23 | 0.88 |
| 26 | Hodgkin lymphoma | C81 | 9115 | 26 | 0.79 | 5714 | 24 | 0.73 |
| 27 | Salivary glands | C07-C08 | 7676 | 27 | 0.66 | 5106 | 26 | 0.65 |
| 28 | Vagina | C52 | 5208 | 28 | 0.45 | 2918 | 30 | 0.37 |
| 29 | Nasopharynx | C11 | 5086 | 29 | 0.44 | 3715 | 28 | 0.47 |
| 30 | Anus | C21 | 4895 | 30 | 0.42 | 3486 | 29 | 0.44 |
| 31 | Testis | C62 | 4414 | 31 | 0.38 | 1955 | 32 | 0.25 |
| 32 | Vulva | C51 | 3446 | 32 | 0.30 | 1756 | 33 | 0.22 |
| 33 | Melanoma of skin | C43 | 3048 | 33 | 0.26 | 2053 | 31 | 0.26 |
| 34 | Mesothelioma | C45 | 1676 | 34 | 0.14 | 1577 | 34 | 0.20 |
| 35 | Kaposi sarcoma | C46 | 92 | 35 | 0.01 | 56 | 35 | 0.01 |
Table 1 Distribution of new cases and deaths in 2018, India[4].
It is studied that cancer is one of all non-communicable diseases affecting the economy of India, as well as the rest of the world. The Out Pocket Expenditure (OPE) for cancer care in a private hospital setting is nearly about three times that of the government facilities (National Sample Survey Office, 2014). Approximately 40% of cancer patients hospitalized are financed, mainly through borrowing money, sale of assets and contribution from friends and relatives. The medical expenditure mainly includes doctor’s fees, investigation charges (blood tests, X-ray, CT-scan, MRI, PET scan, ultrasonography, mammography, biopsy, FNAC, etc.), Chemotherapy/radiation charges, expenditure on medicines, bed charges and other miscellaneous expenses (like attendant charges, physiotherapy charges, personal medical appliances, blood transfusion and oxygen charges). The total expenditure is the aggregation of medical expenditure and transport charges for the patients, food transport on others, expenditure on others, expenditure on escorts and their lodging charges [2]. The treatment for cancer disease is one of the costliest treatment amongst all the chronic diseases, it has various treatments included, e.g. surgery, chemotherapy, radiation therapy, hormonal therapy, immunotherapy, stem cell therapy etc [5].
Cancer is also the second most common disease in India which is responsible for maximum mortality. The world’s population is expecting to be 7.5 billion by the year 2020 and it is predicted that about 15.0 million new cancer cases will be diagnosed with deaths of about 12.0 million cancer patients. It is believed that in near future the number of cancer patients will increase in the developing and underdeveloped countries, which may be risen to 70%; that is a serious issue for all and requires a lot of planning to prevent the disease. The magnitude of the cancer problem in the Indian sub-continent is annually increasing which is estimated at approximately 11 million by 2018 [6]. The top 5 (five) cancers sites such as breast, oral, cervical, gastric and lung cancers are most prevalent in India [7]. It was observed that the deaths rate was increasing rapidly due to cancer disease in India i.e. from 8,19,354 (2004) to 9,79,786 (2010), which was increased by 19.5%. illustrated in Table 2 [8].
| Year | No. of deaths due to cancer |
|---|---|
| 2004 | 819354 |
| 2005 | 846635 |
| 2006 | 863575 |
| 2007 | 907838 |
| 2008 | 846172 |
| 2009 | 962832 |
| 2010 | 979786 |
Table 2 Cancer mortality in India[8].
The most common cancer prevalence amongst the males is Ca Lung followed by Ca Stomach globally but in the more developed countries the Ca Prostate is prevalent. On the other hand, the Ca Breast and Ca Cervix are prevalent worldwide amongst females, as well as the Ca Cervix is most prevalent in less developed countries. Carcinomas of the lung, colorectal, and stomach are most common among both men and women, globally (Table 3) [9].
| Year | Region | New Cases (in Millions) | Deaths (in Millions) |
|---|---|---|---|
| 2000 | More developed countries | 4.7 | 2.6 |
| Less developed countries | 5.4 | 3.6 | |
| All countries | 10.1 | 6.2 | |
| 2020 | More developed countries | 6 | 3.5 |
| Less developed countries | 9.3 | 6.3 | |
| All countries | 15.3 | 9.8 |
Table 3 Number of cancer-related deaths in the world estimated for the year 2000 and projected cancer incidence for the year 2020[9].
The ‘cancer’ disease is a very complex group of diseases which may have direct or indirect and known or unknown causes, such are as follows, Unhealthy lifestyle, tobacco (both smoking and chewing), poor diet and physical inactivity, increasing BMI, alcohol, genetic, pollution or chemicals, radiations etc. [10,11]. Cancer can be prevented at a certain level, if an individual may follow few habits such areas home-made food with a lot of green leafy vegetables, fruits and dry fruits, regular exercise (walking, cycling, swimming and other exercises according to age and circumstances, around 45 minutes a day) or maybe thrice a week, no smoking or alcohol, avoid an increase in BMI, Pollution and exposure to radiation). Cancer therapy along with mere treatment also encompasses management of pain and psychological trauma; it is often referred to as care beyond cure [12,13].
In the first encounter with cancer news or diagnosis, the patient, as well as the patient’s attendants, are often undergoing extreme mental trauma and stress coupled with apprehension and uncertainty. The experience is worsened by financial distress of long term treatment and the disruption of normal life, side effects of radiotherapy, chemotherapy and healing experience from surgery, add to already negative experience. A study conducted by the Public Health Foundation of India at Bhubaneswar, on the cancer patient’s satisfaction levels in cancer care elicits the trauma of cancer patients in Indian public health. Most of the tertiary health care where cancer treatment is available are located mostly in metropolitan cities which may take many hours and long distance to reach for treatment. There is a lack of diagnostic skills among primary healthcare doctors, delay in referrals often worsens the situation [12,14]. Social stigma also associated with cancer due to changes in body image e.g. (Breast removal in MRM surgeries), misconceptions about cancer-related treatment, cancer mortality and false belief that cancer is contagious [12,15].
Aim and Objectives of the Study• To explore the socio-demographic profile of cancer survivals
• To assess the cancer burden in tertiary care settings of Chandigarh
• To study the existing comorbidities in cancer patient
• To analysis the lifestyle of the patient including daily diet and physical activity
Inclusion and Exclusion
Inclusion:
• All cancer diagnosed patients coming for treatment
• All social, economic, religion and geographical background
• All age group and gender
Exclusion:
• Non-cancerous patients
• Those patients are not willing to participate in the study
Materials and Methods
The research was cross-sectional and descriptive in which both quantitative and qualitative methods were used. The retrospective data were collected by using primary and secondary methods during the study. The primary data was collected directly from the patients along with their accompanying attendants, family members and caretakers through interview. The semi-structured interview schedule was developed and used during the data collection throughout the study. The primary data included demographic details, other external or internal factors, encompassing lifestyle pattern, diet habits, exercise and substance use, such factors may be directly or indirectly related to the cancer causation. The primary data also described the previous treatment received for cancer if diagnosed outside the host institutions; the primary level of delay for treatment initiation was studied during the research, the socio-economic impact of cancer on the family if the patient was the breadwinner of the family and the impact on other family members accompanying the patient. The level of satisfaction of cancer survivals during the treatment with the cancer facilities and management received at host institutions was also incorporated. The secondary source of the data was retrieved from the case files stored in record rooms that included the demographic profile, clinical details along with cancer diagnosis, type of cancer, primary and secondary cancer site, the staging of the patients, treatment taking related to cancer, change in BMI, follow updates and other details associated with treatment. The longitudinal study was started from the first day of registration of the recorded cancer patients. The registered patient was fully observed for at least 5 to 6 months by investigators to get the best results during the study. The study period for the whole research was two consecutive years including 18 months for data collection, quarterly report writing and follow-up and six months was kept reserved for data entry and management, data analysis and report writing. The data analysis was done by using MS-Excel and IBM SPSS Statistics 20 (Statistical Package for Social Science), the Mean (average), Standard Deviation, Standard Error and correlation were calculated by using statistical software. Some tests were applied, e.g. One-way Anova, (2-tailed) Karl Pearson’s/Spearman’s Correlation, Significance (p-value) and Skewness. The universe of the study was cancer patients attending Government Medical College and Hospital (GMCH), Sector-32, Chandigarh and Post- Graduate Institute for Medical Education and Research (PGIMER), Sector-12, Chandigarh. All OPD (Out-Patient Department) and IPD (In-Patient Department) were included in the study and data were collected from those patients who were coming to attending the health care facility during the study period. This was done to the generalization of findings for the heterogeneous population in the study. The patients were enrolled on and after 2nd January 2017 till 1st January 2019. The patients diagnosed with rare cancer disease were also enrolled and studied. The interview method was followed to collect the data from cancer survivals with the help of the semi-structured interview schedule which consisted of various sections meeting the requirement and objectives of the study.
Results
The results are based on the data retrieved from the primary and secondary source of collected data during the study. According to the study, there were 3012 patients diagnosed with cancer coming to OPDs were interviewed, including gender and all categories of age, income, demographic group, cancer site, etc. If patients were unable to respond then the close relative or attendant were interviewed by taking pre-consent and only willing to participate in the study were included. The following results were as per data collected, evaluated, interpreted and divided into different categories.
Socio-Economic Status of Patients Coming for Treatment
The overall incidence of cancer patients coming to tertiary care centres of Chandigarh for treatment and classification based on age and locality shown in the Table 4 maximum patients lies between the age group 22 years to 80 years i.e. 2886 which was 95.81% patients amongst 3012 (Male: 1398 and Female: 1614) patients. The male population coming from rural areas were 996 and from urban it was 402. Similarly, the female population coming from rural areas were 1054 and 560 from urban areas (total rural population was 2050 which was 68% among 3012 respondents on the other hand 962 from urban which was 32%) (One-way ANOVA test applied on age and locality (rural/urban), the p-value was ≤ 0.025, mean age rural: 51.01, urban: 52.25, total: 51.40, SD=Rural: 14.28, Urban: 13.82, total: 14.14, Skewness=rural: -ve 410, urban: -ve 540, total: -ve 451). As compared to the family members of the cancer patients the overall education level was high, e.g. there were 906 (30%) illiterate among 3012 patients, whereas in the family members only 72 (2.39%) were found illiterate among 3012 families of cancer patients. The overall percentage was higher as compared to education level from Matric to Post Graduation in families, i.e. 2593 (86%) and education level among patients, i.e. 1043 (34%). There were 589 patients and 99 family members of cancer patients have educational qualification up to primary level. The income levels of the cancer survivals those who are coming for their treatment to the tertiary care centres viz. GMCH-32 and PGIMER-12. The figure shows the monthly income level of the patient which is below Rupees 10,000 to Rupees 1,00,000. There were 2637 (87.54%) patients who responded that they had income below Rs. 10,000 and only 375 (12.46%) had an income of more than Rs. 10,000 which was very low to survive and of course for bearing the expenditure of cancer treatment which usually exceeded out of pocket. Applying Karl Pearson’s and Spearman’s Rho 2-tailed level correlation, the 73.4% or 2210=n patients had income between Rs. 1000.01 to Rs. 13,500, which was significant and ≤ 0.05, SD=0.641, SE=0.12. The loss of Rs. 1001 to Rs. 2,50,900 was significantly ≤ 0.05 beard by 92.4% or 2789=n, SD=0.508, SE=0.009 patients or family during the treatment of cancer. 680 patients had income ≤ Rs. 1000 i.e. 22.6% and 184 patients or family beard the loss between Rs. 2,50,901 to Rs. 5,00,800 i.e. 6.1% only. The cancer treatment included not only the cost of medicines but also included the travelling cost, investigation charges (Histopathology, cytology, Bio-Chemistry, Haematology, USG, Endoscopy, X-Ray, CT-Scan, MRI-Scan, PET-Scan and sometimes genetic studies). During the treatment patients unable to work which had a direct impact on their income in the case of the patients was a breadwinner of the family itself. There were only 526 patients who had BPL (Below Poverty Line) (mean=1.83, significant ≤ 0.05) cards which provided some financial relaxation in treatment investigations in the government hospitals only. It was not much very useful because some important investigations had long waiting appointments but the cancer patients could not wait for long and also poor patient could not afford the expensive investigations, surgeries and treatment from the privacy settings.
| Age-wise distribution | Rural | Urban | Total |
|---|---|---|---|
| 02-11 | 11 | 5 | 16 |
| 12-21 | 56 | 24 | 80 |
| 22-31 | 111 | 38 | 149 |
| 32-41 | 290 | 115 | 405 |
| 42-51 | 505 | 218 | 723 |
| 52-61 | 553 | 298 | 851 |
| 62-71 | 418 | 203 | 621 |
| 72-81 | 86 | 51 | 137 |
| 82-91 | 19 | 9 | 28 |
| 91 and above | 1 | 1 | 2 |
| Total | 2050 | 962 | 3012 |
| Cancer patients from the age-group of 02 years to 91 years and above. | |||
Table 4 Shows the overall incidence of cancer patients based on age and locality.
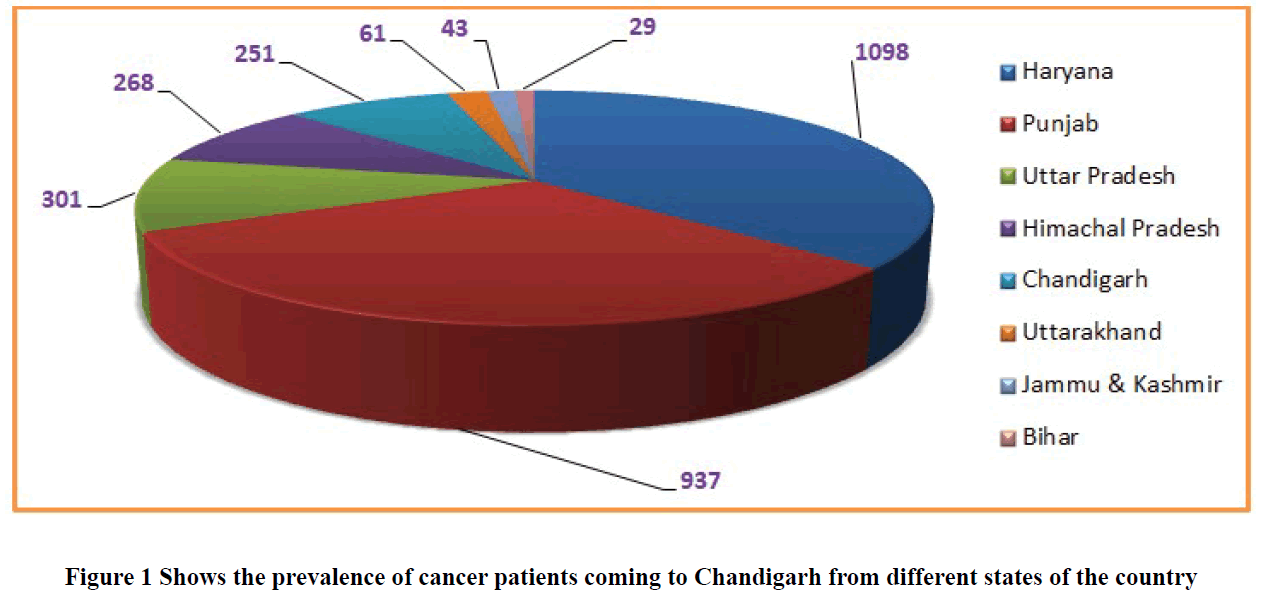
Many patients were coming to the GMCH-32 and PGIMER-12, for cancer treatment from various states shown in Figure 1 e.g. 1098 (36.5%) patients among 3012 recorded patients from Haryana, followed by 937 (31.1%) were from Punjab, 301 (10%) Uttar Pradesh, 268 (8.9%) Himachal Pradesh, 251 (8.3%) Chandigarh, 61 (2%) Uttarakhand, 43 (1.4%) Jammu and Kashmir and 29 (0.96%) were from Bihar state. Unavailability of an appropriate number of tertiary care centre, lack of guidance and late referrals to advance care centres may play a significant role in increasing the burden of cancer in Chandigarh. It has also plays important role in the delay in the initiation of cancer-related treatment. However, it may lead the cancer disease from the initial stage to the advance stage cancer which is incurable and only palliative treatment is available at this stage.
Lifestyle of Cancer Patients before Diagnosis
The lifestyle plays an important role in the life of an individual, which decides health and well-being. If a person has a good lifestyle including a healthy diet, physical activity, and workout or exercise that prevents many communicable and non-communicable diseases the cancer is one of them. If an individual holds a poor lifestyle including an unhealthy diet like junk food, tobacco use (smoking and chewing), alcohol consumption, etc., it can be causing a lot of diseases including cancer. Though many patients belong to BPL and low-income group families patients had a habit of consuming health hazardous substance and non-vegetarian diet, while checking the correlation between BPL families and substance abuse patients there were significant results came out i.e. while computing (mean of BPL families= 1.83, SD=0.380), (mean of smoking=1.74, SD=0.436), (mean of alcohol=1.79, SD=0.409), (mean of chewing tobacco=1.94, SD=0.240) and (mean of non-vegetarian diet=1.58, SD=0.493), the estimated error: 199.76 whereas the standard error: 5.528 and it was significant ≤ 0.05. There were 25.6% (771) patients had a smoking habit of Biddi, Cigarette and Hukka, 6.1% (184) patients had a habit of chewing Tobacco, Jarda, Gutkha, Beetle Nuts, Pan, etc., and 21.3% (641) patients had a habit of consuming alcohol, many of them had either one type of consuming the substance. There were 41.5% (1251) consuming non-vegetarian diet regularly including (red meat 31.1%, white meat 35.1%, raw meat 0.2%, and egg 33.6%) and around 58.5% (1761) were vegetarian. Nearly, around 78.7% (2370) consumed junk food in the form of samosa, pakoda, pizza, burger, chips, and other salts, sugar, refined flour containing food. Junk food may be defined as “those commercial products, including candy, bakery goods, ice cream, salty snacks and soft drinks, which have little or no nutritional value but have plenty of calories, salt, and fats”. An unhealthy diet is one of the major risk factors for a range of chronic diseases, including cardiovascular diseases, cancer, diabetes and other conditions linked to obesity. It is highly recommendations for an individual’s healthy diet to include eating seasonal fruits, vegetables, legumes, nuts and grains in a balanced amount, eliminate the excessive use of salt, sugars and fats in diet [16,17]. Only 30.7% (924) patients accepted the habit of exercise most of them were irregular and 69.3% (2088) had no exercise habit. Along with a healthy diet and exercise, proper sleep is also important, 46.1% (1390) were having Regular sleep, 38.3% (1153) were having Average sleep and 15.6% (469) having irregular sleep habit. Somehow such lifestyle factors influencing the individual’s life and has have a direct or indirect impact on the spread of cancer.
Stages of Cancer Patients, Co-Morbidities in Cancer Patients and Family History, BMI (Body Mass Index), and Problems Faced by Patients during Treatment
The present study reveals that the cancer burden on Chandigarh, according to the current study 3012 patients were interviewed and followed up in 24 months from both tertiary care centres GMCH and PGIMER in the period of 2017- 19. There were 8.67% (261) patients belongs to Stage I of cancer, 22.47% (677) patients were Stage II, 24.47% (737) patients were Stage III and 33.07% (996) where belongs to Stage IV of cancer. There were 20.3% (611) of the breast, 16.1% (485) oral cavity, 8.2% (247) oesophagus, 8.1% (244) cervix, 4.5% (135) were lung cancer patients and rest were laryngeal, sarcoma, ovarian, gallbladder, colon and other cancers.
In Table 5 out of 3012 respondents, 8.53% (257) had a family history of cancer, in which 3.15% (95) patients accepted that their mother had cancer, 2.39% accepted that their father had cancer, 2.15% (65) patients accepted that their brother had cancer and 2.05% (62) patients accepted that their sister had cancer. The mean value of family cancer history= 1.91, SD=0.279, patients were absolutely in a good state (in months) mean=16.70, SD=28.59 and the time gap between the first symptom developed and the first consultation to doctor (in days) mean=78.92, SD=333.359, (p-value ≤ 0.01). The respondents have also various co-morbidities besides cancer and some patients have a cancerous family history. Out of 3012 patients, 18% (527) have hypertension, 9% (268) have diabetes, 7% (194) kidney or gall bladder stones and 4% (128) have respiratory diseases. The BMI (Body Mass Index) of 3012 patients was calculated according to both International and Asian standard. According to the International standard scale, 23.9% (721) were categorised in a pre-obesity stage which may be considered on borderline, the 7% (212) patients lied in obesity class I to class III, 45.1% (1358) were having normal weight and 23.9% (721) were underweight category shown in Table 6.
| First Degree Relatives | Frequency | Percent |
|---|---|---|
| Family history of cancer | 257 | 8.53% |
| Mother | 95 | 3.15% |
| Father | 72 | 2.39% |
| Sister | 62 | 2.05% |
| Brother | 65 | 2.15% |
| NA | 2755 | 91.46% |
| Total | 3012 | 100.00% |
Table 5 The cancer history in first degree relatives of cancer patients.
| BMI (Body Mass Index) | SCALE | Frequency | Percent |
|---|---|---|---|
| <18.5 | Underweight | 721 | 23.9 |
| 18.5-24.9 | Normal weight | 1358 | 45.1 |
| 25.0-29.9 | Pre-obesity | 721 | 23.9 |
| 30.0-34.9 | Obesity class I | 181 | 6 |
| 35.0-39.9 | Obesity class II | 28 | 0.9 |
| 40> | Obesity class III | 3 | 0.1 |
| Total | 3012 | 100 | |
Table 6 BMI (Body Mass Index), according to international standard [18].
Table 7 shows that the measurement of BMI according to Asian standard in which the 32.83% (989) patient falls in ‘Lean’ weight category, 30.99% (933) patient falls in ‘Obese’ weight category, 23.93% (721) patient falls in ‘Normal’ weight category and 12.25% (369) patient falls in ‘Over’ weight category.
| BMI (Body Mass Index) | Scale | Frequency | Percent |
|---|---|---|---|
| <18.5 | Lean | 989 | 32.83 |
| 18.5-22.9 | Normal | 721 | 23.93 |
| 23.0-24.9 | Overweight | 369 | 12.25 |
| 25> | Obese | 933 | 30.99 |
| Total | 3012 | 100 | |
Table 7 BMI (Body Mass Index), according to Asian standard [19].
Table 8 shows the problems faced by cancer patients coming to Chandigarh for treatment, 18.4% (555) patients faced financial problems during the whole cancer-related treatment, 4% (120) patients faced travelling problem, 16.2% (489) patients suffered from both financial and travelling problem, 10.6% (319) patients faced the problem of accommodation along with financial and travelling problems and 6.8% (205) patients faced other health issues than cancer during treatment. There were only 30.7% (924) of patients were physically active; they spent their time walking, exercise, household work etc. The Karl Pearson’s/Spearman Rho correlation between BMI, age and locality (i.e. Rural and Urban) was significant ≤ 0.000, SD=0.610 and SE=0.011.
| Problems faced | Frequency | Percent |
|---|---|---|
| Financial | 555 | 18.4 |
| Financial, travelling | 489 | 16.2 |
| Accommodation, financial, travelling | 319 | 10.6 |
| Health issues | 205 | 6.8 |
| Travelling | 120 | 4 |
| Financial, travelling | 67 | 2.2 |
| Financial, travelling, health issues | 12 | 0.4 |
| Financial, Mental Stress | 9 | 0.3 |
| Lack of guidance | 8 | 0.3 |
| Accommodation, travelling | 5 | 0.2 |
| Financial, health issues | 7 | 0.2 |
| Mental Stress | 6 | 0.2 |
| Study loss | 6 | 0.2 |
| Travelling, health issue | 5 | 0.2 |
| Travelling | 5 | 0.2 |
| Delay in treatment by a doctor | 2 | 0.1 |
| Accommodation | 1 | 0 |
| Family issues | 1 | 0 |
| Financial, family issues | 1 | 0 |
| Financial, lack of guidance | 1 | 0 |
| Financial, abandonment | 1 | 0 |
| Financial, lack of awareness | 1 | 0 |
| Financial, study loss | 1 | 0 |
| Harassment, exploitation | 1 | 0 |
| Travelling, Mental stress | 1 | 0 |
| No | 1183 | 39.3 |
| Total | 3012 | 100 |
Table 8 Problem faced by cancer patients during the treatment.
Discussion
As the various studies conducted by individuals or institutions reflects the increasing incidence of cancer epidemiology worldwide. The carcinoma of the breast is the most common cancer on the planet, as compared to the world the developed countries are more affected with this approximately 50% of breast cancers has diagnosed and it’s estimated that in India over 100,000 new cases of breast cancer will be diagnosed annually in nearest future. An ICMR-PBCR (Indian Council for Medical Research-Population Based Cancer Registry) data claims that more than 30% of women of the urban population of big cities like New Delhi, Mumbai, Ahemdabad, Kolkata, and Trivandrum. The increasing incidence of cancer from 0.5% to 2% annually has studied all over the Indian sub-continent in all age groups but it was noted more in below 45 years of the population [20].
According to WHO (World Health Organization) 2018, 18.1 million new cancer cases were diagnosed and nearly about 9.6 million deaths were registered causing cancer. The study revealed that throughout the lifespan of the world’s population, one out of five men and one out of six women developed cancer, and the death ratio is one out of 8 men & one out of eleven women died due to cancer disease only. It is estimated that the 5 years of a cancer diagnosis, called 5-year prevalence is existing among 43.8 million PLCD (Population Living with Cancer Disease). While studying the global data in 2018, on cancer incidence it shockingly came into existence i.e. around 60% out of the total cancer population, including men, women, newly diagnosed and cancer deaths was happened only in the Asian region. And viewing the European country’s data on cancer incidence was 23.4% and only 9.0% of deaths were recorded causing cancer as compared to the global death rate. If talking only about America, the cancer incidence was 21.0% of the global cancer population and deaths due to cancer was 14.4% as compared to the world’s cancer-causing death rate. On the account of cancer site, the carcinoma of the lung, breast among female and colorectal ranked top three cancers among all cancers and also lung stood tall at first place in death followed by colorectal at second place and fifth place reserved for breast cancer respectively and collectively these are responsible for 1st/3rd incidence and mortality globally. In 2018, there were 2.1 million cases diagnosed with lung and female breast contributing nearly about 11.6% of the total cancer burden worldwide. The 1.8 million Colorectal cancer cases were estimated approximately around 10.2% of the total population known as the third most commonly diagnosed cancer, followed by prostate cancer at fourth position with 1.3 million cases i.e. 7.1%, and stomach cancer stands at fifth place with 1.0 million cases i.e. 5.7% [21]. A study was conducted on 169 cancer patients consisted (21.3%) urological malignancies, (18.0%) were haematological cancer, (15.0%) head and neck cancer and (14.0%) breast cancer [22]. Vijayvergia. N, et al. defined that the poor lifestyle including smoking and alcohol intake may have chances up to 35% to developed second malignancies, in fact, other risk factors like physical inactivity, poor diet, increasing body weight etc., also influence the chance of second malignancies [23]. It is observed that due to over body weight or increasing BMI (Body Mass Index) has more chances to develop carcinoma of breast and prostate up to 70%, colorectal, oesophagus, pancreatic, liver, cervix, ovary, as well as non-Hodgkin lymphoma and multiple myeloma. A study reveals that an adjuvant chemotherapy therapy given to women with a BMI ≥ of 30 kg/m2 had a poor prognosis with hormone-receptor-positive tumours as compared to women with a normal BMI. On the other hand, adjuvant endocrine therapy given to postmenopausal women with positive hormone receptors, including stage I to stage III breast cancer showed that women with BMI ≥ 35 kg/m2 or more than this had a chance of recurrence of disease as compared to the women with BMI ≤ 23 kg/m2 [23]. In the study conducted in Italy and Switzerland in 1998, those who smoked 25 cigarettes or more per day, has greater chances of risk of oropharyngeal cancer up to seven-fold. In the association with laryngeal cancer, individuals who don’t even smoke but consumes alcohol 25 g/ml, 50 g/ml, or 100 g/ml per day respectively found a high risk of cancer. A metaanalysis study of 20 controlled groups of laryngeal cancer and all together included more than 3,500 cases reported a strong direct relationship between alcohol consumption and high risk of laryngeal cancer [24]. Smoking is injurious to health, almost every individual heard once in a life, cigarettes, cigars, pipe tobacco, biddi, etc., are made from dried tobacco leaves, and other harmful ingredients are added for flavour or pleasure. While smoking such a substance produces smoke due to the burning of harmful tobacco and a complex mixture of chemicals added to it. Tobacco smoke is made up of more than 7,000 chemicals, including over 70 known to produce cause carcinogens which may lead to harmful heart/lung diseases and of course cancer too. Figure 2, it is showing the harmful chemicals found in any form of tobacco smoking, which is extremely responsible for causing the deadliest diseases including cancer [25].
Smokeless tobacco or chewing tobacco contains nicotine, individual get into its addiction if starts consuming likewise, smoking tobacco and nicotine starts circulating into the bloodstream. By quitting tobacco consumption turns into an intense craving, rapid irritation/depression and it also increases appetite. It also causes cancer of the oral cavity, e.g. lip, tongue, buccal mucosa, etc., and also increases the chances of pancreatic cancer and oropharyngeal cancer. Sometimes tobacco increases the chances of the pre-cancerous lesion in the mouth called leukoplakia (small white patches) [26].
In a study conducted by Sharon Y Do, et al. on 84 cancer patients, among them 74% had chronic pulmonary disease, whereas, on the other hand, 50% of them had multiple co-morbidity history [27]. A comparison study was conducted by Roy. S, et al. on 560 patients, were divided into two equal groups i.e. Group 1 and Group 2, contains 280 (50%- 50%) patients each. Group 1 included 280 (50%) cancer patients and Group 2 (50%) non-cancerous patients. Group 1 had more co-morbidities than the group 2, such are as follows, Hypertension 180 (64.3%), Hyperlipidaemia 157 (56.1%), Osteoarthritis 96 (34.3), Hypothyroidism 61 (21.8), Diabetes mellitus 61 (21.8%), Coronary artery disease 61 (21.8%), Vitamin D deficiency 48 (17.1%), Anxiety disorder 45 (16.1%), Depression 38 (13.6%), Asthma 32 (11.4%), Chronic kidney disease 30 (10.7%), Chronic obstructive airway disease 20 (7.1%), Cerebrovascular accident 15 (5.4%), Peripheral arterial disease 14 (5.0%), Congestive heart failure 12 (4.3%), Carotid stenosis 7 (2.5%), Bipolar disorder 3 (1.1%), Liver disease 2 (0.7%) and Schizophrenia 1 (0.4%) [28].
Table 9 shows the common symptoms of cancers which are useful in the early detection of disease and further help in the treatment of cancer at the early stage. For example, breast cancer is the most common cancer among the female population and it is possible to detect at an early stage if the following symptoms noticed, a lump in the breast and pain, asymmetry, skin retraction, recent nipple retraction, blood-stained nipple discharge, eczematous changes in areola [29,30].
| Site of cancer | Common symptoms |
|---|---|
| Breast | Lump in the breast, asymmetry, skin retraction, recent nipple retraction, blood-stained nipple discharge, eczematous changes in areola |
| Cervix | Post-coital bleeding, excessive vaginal discharge |
| Colon and rectum | Change in bowel habits, unexplained weight loss, anaemia, blood in the stool (rectal cancer) |
| Oral cavity | White lesions (leukoplakia) or red lesions (erythroplakia), growth or ulceration in the mouth |
| Naso-pharynx | Nosebleed, permanently blocked nose, deafness, nodes in the upper part of the neck |
| Larynx | Persistent hoarseness of voice |
| Stomach | Upper abdominal pain, recent onset of indigestion, weight loss |
| Skin Melanoma | Brown lesion that is growing with irregular borders or areas of patchy colouration that may itch or bleed |
| Other skin cancers | Keratosis (lesion or sore on the skin that does not heal) |
| Urinary bladder | Pain, frequent and uneasy urination, blood in the urine |
| Prostate | Difficulty (long time) in urination, frequent nocturnal urination |
| Retinoblastoma | White spot in the pupil, convergent strabismus (in a child) |
| Testis | Swelling of one testicle (asymmetry) |
Table 9 Signs and symptoms which may help in early detection of cancer [30].
Conclusion
The study was conducted on cancer patients coming to tertiary care settings for treatment to the Chandigarh because there was a lack of cancer-related treatment at their locality. Most of the patients were coming from neighbouring states of Chandigarh and increasing the burden in local hospitals of the city which couldn’t be ignored. The patients of the city are suffering from long waiting treatment, including surgeries, chemotherapy, radiotherapy, MRI, CT-Scans and other basic investigation. It may result in a delay of one to two months for starting the treatment which may increase the stage of the disease. The incidence of cancer patients increasing every year in the institute where the study was conducted is as follows. In the year 2015 there were 1750 patients new cancer patients got registered, in the year 2016 there were 1800 patients, in the year 2017 there were 1959 patients, in the year 2018 there were 1969 patients and in the year 2019, there were 2222 patients registered the increasing growth rate of burden is approximately 78.75% in 05 years only.
There were 37.15% (600) Ca Breast patients, followed by 15.05% (243) were Ca Cervix patients prevalent among female and 15.46% (216) were Ca Oral Cavity patients followed by 8.30% (163) Ca Oesophagus prevalent among male cancer patients. This represented the increasing cancer burden on hospitals day by day. Cancer treatment is very costly; in a study, the delay of two to three months was observed due to unawareness and lack of guidance about cancer symptoms, treatment. It was also observed the personal ignorance and family ignorance may result in the delay in the initiation of cancer-related treatment. It was impacted the out of pocket expenditure on individual and family 46.9% of patients spent Rs. 50,000/- to Rs. 1,00,000/- , there were 11.4% spent Rs. 1,50,000/- to Rs. 2,50,000/- around 6.1% spent Rs. 2,50,000 to Rs. 5,00,000/- approximately 1.5% patients spent more than Rs. 5,00,000/- before coming to the host institutes for treatment. A lot of the patients 12.5% (378) need to dispose of the assets like land, house, jewellery, cattle, etc., 52.9 % (1592) borrowed the money for cancer treatment at a heavy rate of interests. When patients visited the GMCH and PGIMER the proper guidance and facilities were provided in the form of poor free treatment, financial assistance, grief counselling, counselling for quitting substance use (smoking, alcohol, tobacco) diet and physical exercise. The overall satisfaction level of patients was calculated by using (How to Set Half Rating Scale (Poor to Excellent) by HeshamZebida) the 95.3% (2870) responded to excellent after taking treatment included behaviour of doctors, staff, and all facilities provided to patients.
The burden of cancer can be reduced if preventive measures adopted, healthy diet and physical activity may also prevent the chances of cancer. The elimination of the use of tobacco, alcohol and smoking also prevents cancer and proper guidance and awareness of symptoms and treatment can lessen the chance of mortality.
Declarations
Acknowledgement
This study was conducted under the project sponsored by Indian Council for Medical Research, New Delhi, India to the Department of Radiation Oncology, Government Medical College and Hospital, Chandigarh, India, in year January 2017 to January 2019.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- World Health Organization. "Integrated chronic disease prevention and control."World Health Organization. Available online: http://www. who. int/chp/about/integrated_cd/en/(accessed on 2 February 2013),2016.
- Rajpal, Sunil, Abhishek Kumar, and William Joe. "Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014."PloS One,Vol. 13, No. 2, 2018, p. e0193320.
- Nandakumar, A. "Over 17 Lakh New Cancer Cases in India by 2020: ICMR. New Delhi, India: ICMR; 2016. May 19,[Last accessed on 2016 Oct 20]."
- Dar, M., and K. Sharma. "Burden of cancer in India: GLOBOCAN 2018 estimates incidence, mortality, prevalence and future projections of cancer in India."Journal of Emerging Technologies and Innovative Research,Vol. 6, No. 6, 2018, pp. e505-14.
- NIH National Cancer Institute. "Types of Cancer Treatment." https://www.cancer.gov/about-cancer/treatment/types
- Ali, Imran, Waseem A. Wani, and Kishwar Saleem. "Cancer scenario in India with future perspectives."Cancer Therapy,Vol. 8, 2011, pp. 56-70.
- India Against Cancer. "Common Cancers." http://cancerindia.org.in/common-cancers/
- Chandrani, Debrani. "Health seeking behaviour of tobacco related cancer patients: A study of cachar district Assam." 2013. https://shodhganga.inflibnet.ac.in/handle/10603/21163#
- World Health Organization."National cancer control programmes: policies and managerial guidelines." World Health Organization, 2002.
- WebMD. "Cancer Center." https://www.webmd.com/cancer/default.htm
- American Cancer Society. "What causes cancer?" https://www.cancer.org/cancer/cancer-causes.html
- Access Health International. "Cancer Care in India: The mental and financial burdens." 2018. https://accessh.org/cancer-care-india-mental-financial-burdens/
- Néron, Andrée. "Care beyond cure: Management of pain and other symptoms: Published in collaboration with l’Association des pharmaciens des établissements de santé du Québec (AP ÉS) and the Canadian Society of Hospital Pharmacists (CSHP)."The Canadian Journal of Hospital Pharmacy,Vol. 62, No. 2, 2009, p. 178.
- Mahapatra, Sandeep, Sukdev Nayak, and Sanghamitra Pati. "Quality of care in cancer: An exploration of patient perspectives."Journal of Family Medicine and Primary Care,Vol. 5, No. 2, 2016, pp. 338-42.
- Kaur, Reetinder. "Cultural beliefs, cancer and stigma: Experiences of patients from Punjab (India)."Studies on Ethno-Medicine,Vol. 9, No. 2, 2015, pp. 247-54.
- NDTV Food. "What Is Junk Food? Why Is It Bad For You?" https://food.ndtv.com/food-drinks/what-is-junk-food-why-is-it-bad-for-you-1772375
- World Health Organization. "Healthy diet." https://www.who.int/news-room/fact-sheets/detail/healthy-diet
- World Health Organization, Regional Office for Europe. "Body mass index-BMI" https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
- Aziz, Nuzhat, Sailaja Devi Kallur, and Praveen Kumar Nirmalan. "Implications of the revised consensus body mass indices for Asian Indians on clinical obstetric practice."Journal of Clinical and Diagnostic Research: JCDR,Vol. 8, No. 5, 2014, p. OC01.
- Agarwal, Gaurav, and Pooja Ramakant. "Breast cancer care in India: The current scenario and the challenges for the future."Breast Care,Vol. 3, No. 1, 2008, pp. 21-27.
- International Agency for Research on Cancer. "Latest global cancer data, 2018."World Health Organization,2018, pp. 13-15.
- Jadoon, Nauman A., et al. "Assessment of depression and anxiety in adult cancer outpatients: A cross-sectional study."BMC Cancer,Vol. 10, No. 1, 2010, pp. 1-7.
- Vijayvergia, Namrata, and Crystal S. Denlinger. "Lifestyle factors in cancer survivorship: Where we are and where we are headed."Journal of Personalized Medicine,Vol. 5, No. 3, 2015, pp. 243-63.
- Pelucchi, Claudio, et al. "Cancer risk associated with alcohol and tobacco use: Focus on upper aero-digestive tract and liver."Alcohol Research and Health,Vol. 29, No. 3, 2006, pp. 193-98.
- The Oral Cancer Foundation. "Tobacco as a cause." https://oralcancerfoundation.org/understanding/tobacco/tobacco-as-a-cause/
- Mayo Clinic. "Chewing tobacco: Not a safe product." https://www.mayoclinic.org/healthy-lifestyle/quit-smoking/in-depth/chewing-tobacco/art-20047428
- Do, Sharon Y., David A. Bush, and Jerry D. Slater. "Comorbidity-adjusted survival in early stage lung cancer patients treated with hypofractionated proton therapy."Journal of Oncology,Vol. 2010, 2010.
- Roy, Satyajeet, et al. "Comparison of comorbid conditions between cancer survivors and age-matched patients without cancer."Journal of Clinical Medicine Research,Vol. 10, No. 12, 2018, pp. 911-19.
- Famous Bloggers. "How to Set Half Rating Scale 1-5 (Poor to Excellent) by Words." 2012. https://famousbloggers.net/rating-scale.html
- World Health Organization."Cancer Control: Knowledge Into Action: WHO Guide for Effective Programmes. Policy and Advocacy. Module 3." World Health Organization, 2008.