Research Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 3
An Analysis of the Presentations of Rhino-Orbital Mucormycosis Amidst the COVID Pandemic: A Case Series Report
Kintu S Shah*, Jineel B Bhatt, Reema M Rawal, Zainab S Dohadwala, Shailjaa N Shah and Kinjal G PatelKintu S Shah, Department of Ophthalmology, C.H. Nagri Eye Hospital, Ellisbridge, Ahmedabad, India, Email: kintushah@yahoo.com
Received: 11-Oct-2022, Manuscript No. IJMRHS-22-76876; Editor assigned: 13-Oct-2022, Pre QC No. IJMRHS-22-76876 (PQ); Reviewed: 27-Oct-2022, QC No. IJMRHS-22-76876; Revised: 09-Mar-2023, Manuscript No. IJMRHS-22-76876 (R); Published: 16-Mar-2023
Abstract
Mucormycosis infection is caused by a group of filamentous molds belonging to the order Mucorales. Source of infection maybe inhalation of spores, contaminated food or inoculation into cut skin or open wounds. In developed countries, mucormycosis occurs primarily in severely immunocompromised hosts (e.g. those with hematological malignancies, organ transplantation, neutropenia, autoimmune disorders or other impairments in immunity). More than 100 cases of mucormycosis in people with COVID-19 have been reported, of which 4 of 5 cases were from India and others from the rest of the world. COVID-19 being an immunocompromising condition and steroids being an important part of therapy led to increasing number of cases of rhino-orbital mucormycosis. Our aim is study ocular presentation of the disease amidst COVID-19 peak.
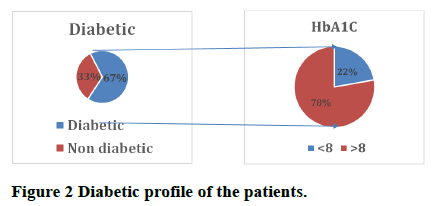
Materials and methods: COVID-19 patients (primary and referral) of rhino-orbital mucormycosis reaching a tertiary health care institute of Ahmedabad were diagnosed via clinical microbiological and radiological tests and evaluated. Vision, ocular movements and slit lamp bio-microscopy of conscious ambulatory patients, bed side examination of critical patients and detailed retinal evaluation of all the patients was done. Systemic comorbidities were noted and diabetic profile was done.
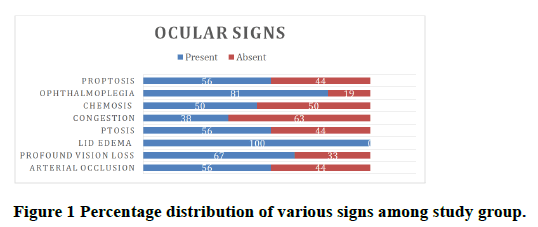
Results and conclusions: Following findings were noted: Lid edema (n=30, 100%), profound vision loss (n=21, 73.33%), ophthalmoplegia (n=26, 86.67%), arterial occlusion (n=16, 60%), Ptosis (n=16, 60%), chemosis (=16, 60%), proptosis (n=16, 60%), Congestion (n=9, 33.33%). Thus, these are the signs to look out for in patients admitted for COVID-19 disease.
Keywords
Mucormycosis, COVID-19, Immunocompromised, Diabetes mellitus, Arterial occlusion
Introduction
Coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV- 2) has been associated with a wide range of opportunistic bacterial and fungal infections [1-3]. Recently, rising mucormycosis cases in people with COVID-19 have been increasingly reported world-wide, mainly from India. The primary reason that appears to be facilitating mucorales spores to germinate in people with COVID-19 is an ideal environment of hypoxia, high glucose (diabetes, new-onset hyperglycemia, steroid induced hyperglycemia), acidic medium (metabolic acidosis, Diabetic Ketoacidosis (DKA), high iron levels (increased ferritins) and decreased phagocytic activity of White Blood Cells (WBC) due to immunosuppression (SARS-CoV-2 mediated, steroid mediated or background comorbidities) coupled with several other shared risk factors including prolonged hospitalization with or without mechanical ventilators [4].
Etiopathology: Mucormycosis is a rare but fatal fungal infection that usually affects patients with altered immunity. Mucormycosis is an angioinvasive disease caused by mold fungi of the genus Rhizopus, Mucor, Rhizomucor, Cunninghamella and Absidia of order: Mucorales, class: Zygomycetes [5]. The Rhizopus oryzae is most common type and responsible for nearly 60% of mucormycosis cases in humans and also accounts for 90% of the Rhino Orbital Cerebral (ROCM) form [6]. Mode of contamination occurs through the inhalation of fungal spores.
Globally, prevalence is nearly 80 times higher (0.14 per 1000) in India compared to developed countries, in a recent estimate of year 2019-2020 [7-9]. In other words, India has highest cases of the mucormycosis in the world. Long term use of corticosteroids has often been associated with several opportunistic fungal infections including aspergillosis and mucormycosis, even a short course of corticosteroids has recently been reported to link with mucormycosis especially in people with DM. A cumulative prednisone dose of greater than 600 mg or a total methyl prednisone dose of 2 g-7 g given during the month before, predisposes immunocompromised people to mucormycosis [10]. There are few case reports of mucormycosis resulting from even a short course (5-14 days) of steroid therapy, especially in people with DM [11]. Surprisingly, 46% of the patients had received corticosteroids within the month before the diagnosis of mucormycosis in the European confederation of medical mycology study [12].
These observations tempted us to study the recent presentations of rhino-orbital mucormycosis amidst COVID-19 pandemic.
Materials and Methods
Ethical review: Applied for ethical review board at NHL municipal medical college Ahmedabad.
Place and duration of study: SVP municipal hospital and CH Nagri eye hospital, Ahmedabad (1 month).
Sample size: 30
Study design: Observational cross sectional study
Methodology: Oral consent of RTPCR positive for COVID-19 patients or their relatives who presented to the eye clinic as well as the ones admitted for treatment in other medical disciplines that were diagnosed on clinical suspicion and confirmed by CT scan of orbit and endonasal swab culture for rhino-orbital mucormycosis were taken and their reports were analysed. Those who tested negative were excluded. A sample size of 30 patients was achieved whose demographic details were noted. History of ocular and other systemic complaints were noted. History of systemic illness including diabetes mellitus was asked and Hyperglycemic index (HbA1C) value was tested. Detail history about the COVID-19 infection and treatment taken was noted. Vision, ocular movements and slit lamp bio-microscopy of conscious ambulatory patients, bed side examination of critical patients and detailed retinal evaluation of all the patients was done.
Inclusion criteria: All patients visiting tertiary medical care tested RTPCR positive for COVID-19 in year 2021 and diagnosed with rhino-orbital mucormycosis via radiological or by microbiological methods giving consent were included in the study.
Exclusion criteria: All patients who tested negative via radiological or by microbiological methods for mucormycosis or were RTPCR negative for COVID-19 were excluded from the study.
RESULTS
Following findings were noted (Figures 1 and 2).
• Bed side referral patients were more than OPD.
• 75% patients were more than 50 years of age and were males.
• 16 patients who had an aggravated disease course had poor glycemic control.
Discussion
Lid edema, ophthalmoplegia and profound vision loss (Up to hand movement and perception of light) were the most common signs in majority of the subjects. OPD patients were less than referral which may suggest debilitating nature of the disease. Old age and male gender might be a non-modifiable risk factor. Dr. Salomon reported a case to warn of the possibility of COVID-19 as a trigger of diabetic ketoacidosis which could predispose an invasive fungal infection or another high risk disease in 2021, our study had similar observation [13]. Dr Muthukrishnan noted a case of retinal artery occlusions and orbital apex syndrome can occur in the patients suffering from mucormycosis in immunocompetent patient while we observed its increased incidence in COVID infected patients [14]. As noted by Dr Lahane, presence of diabetes or altered glycemic profile increases the risk [15]. Our study also had a similar observation. Whereas other studies showed a male preponderance our study had one fourth of its sample as females.
Conclusion
We concluded that rhino-orbital mucormycosis has lid-edema, profound vision loss and ophthalmoplegia when it occurs in COVID-19 patients. Awareness about diagnosis by these signs should be spread in all medical disciplines to reduce the time in ophthalmic referral and intervention.
Limitations
• Small sample size due to COVID-19 restrictions.
• Long term follow-up of the patient not possible.
References
- Reid G, et al. Mucormycosis. In Seminars in Respiratory and Critical Care Medicine, Vol. 41, No. 01, 2020, pp. 99-114.
[Crossref] [Google Scholar] [PubMed]
- Singh AK, et al. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes and Metabolic Syndrome, Vol. 15, No. 4, 2021, pp. 102146.
[Crossref] [Google Scholar] [PubMed]
- Kubin CJ, et al. Characterization of bacterial and fungal infections in hospitalized patients with COVID-19 and factors associated with healthcare associated infections. Open Forum Infectious Disease, Vol. 8, No. 6, 2021, pp. ofab201.
[Crossref] [Google Scholar] [PubMed]
- Eucker J, et al. Mucormycoses. Mycoses, Vol. 44, No. 7, 2001, pp. 253-260.
[Crossref] [Google Scholar] [PubMed]
- Sugar AM. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 5th edition, Elsevier, New York, USA, 2000.
- Skiada A, Pavleas I and Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: An Update. Journal of Fungi, Vol. 6, No. 4, 2020, pp. 265.
[Crossref] [Google Scholar] [PubMed]
- Chander J, et al. Mucormycosis: Battle with the deadly enemy over a five year period in India. Journal of Fungi, Vol. 4, No. 2, 2018, pp. 46.
[Crossref] [Google Scholar] [PubMed]
- Prakash H and Chakrabarti A. Global epidemiology of mucormycosis. Journal of Fungi, Vol. 5, No. 1, 2019, pp. 26.
[Crossref] [Google Scholar] [PubMed]
- Lionakis MS and Kontoyiannis DP. Glucocorticoids and invasive fungal infections. Lancet, Vol. 362, No. 9398, 2003, pp. 1828-1838.
[Crossref] [Google Scholar] [PubMed]
- Hoang K, et al. A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Medical Mycology Case Reports, Vol. 29, No. 1, 2020, pp. 22-24.
[Crossref] [Google Scholar] [PubMed]
- Skiada A, et al. Zygomycosis in Europe: Analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) working group on zygomycosis between 2005 and 2007. Clinical Microbiology and Infection, Vol. 17, No. 12, 2011, pp. 1859-1867.
[Crossref] [Google Scholar] [PubMed]
- Waizel-Haiat S, et al. A case of fatal rhino-orbital mucormycosis associated with new onset diabetic ketoacidosis and COVID-19. Cureus, Vol. 13, No. 2, 2021, pp. e13163.
[Crossref] [Google Scholar] [PubMed]
- Vallinayagam M, et al. Rhino-orbital mucormycosis manifesting as orbital apex syndrome with CRAO in an immunocompetent patient. Journal of Delhi Ophthalmological Society, Vol. 30, No. 1, 2019, pp. 58-61.
- Sen M, et al. Mucor in a viral land: A tale of two pathogens. Indian Journal of Ophthalmology, Vol. 69, No. 2, 2021, pp. 244-252.
[Crossref] [Google Scholar] [PubMed]
- Bawankar P, et al. Central retinal artery occlusion as the presenting manifestation of invasive rhino orbital cerebral mucormycosis. Taiwan Journal of Ophthalmology, Vol. 10, No. 1, 2020, pp. 62-65.
[Crossref] [Google Scholar] [PubMed]