Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 3
Allogeneic Peripheral Blood Stem Cell Transplant in Griscelli’s Syndrome: A Rare Case Report
Mohit Chowdhry1*, Ankita Sharma1, Soma Agrawal1, Manoj Mishra1, Atish Bakane2 and Gaurav Kharya22Department of Paediatric Hemato-Oncology & BMT-CT, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi, India
Mohit Chowdhry, Department of Transfusion Medicine, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi, India, Email: mohit_c@apollohospitalsdelhi.com
Received: 21-Feb-2022, Manuscript No. ijmrhs-22-55095 (M); Editor assigned: 22-Feb-2022, Pre QC No. ijmrhs-22-55095 (M); Reviewed: 18-Mar-2022, QC No. ijmrhs-22-55095 (M); Revised: 20-Mar-2022, Manuscript No. ijmrhs-22-55095 (M); Published: 31-Mar-2022
Abstract
Background: Griscelli Syndrome (GS) type 2 is a rare autosomal recessive disease caused by mutations in the RAB27A gene. Griscelli syndrome is of three types with GS type 2 being the most common variety. It is primarily characterized by a combination of partial albinism, Hemophagocytic Lymphohistiocytosis (HLH), and neurological impairment. GS 2 is mostly lethal unless an allogeneic Peripheral Blood Stem Cell (PBSC) transplantation is performed in time. Case Presentation: We hereby describe a case of GS type 2 in a 3-year-old boy who presented with central nervous involvement and primary HLH. He was also a post-COVID-19 recovered case and had been treated for Cytomegalovirus (CMV) reactivation. The patient was first managed for primary HLH following HLH-2004 protocol using a combination of dexamethasone and etoposide followed by a haploidentical peripheral blood stem cell transplantation and has shown a good response with complete donor chimerism. Conclusion: PBSC transplantation in GS when performed promptly with proper care and support can be successful in providing the patient with a new lease of life.
Keywords
Griscelli syndrome, Hemophagocytic lymphohistiocytosis, Peripheral blood stem cell transplantation
Abbreviations
GS: Griscelli Syndrome, HLH: Hemophagocytic Lymphohistiocytosis, PBSC: Peripheral Blood Stem Cell, CMV: Cytomegalovirus, BMT: Bone Marrow Transplant, GvHD: Graft versus Host Disease
Introduction
Griscelli’s Syndrome (GS) was first described by Griscelli and Siccardi in 1978 at a hospital in Paris [1]. The disease is predominantly found in the Turkish and the Mediterranean population [2].
The disease is usually diagnosed between 4 months and 7 years of age [3]. It can present with a mutation in 3 genes namely MYO5A (GS 1), RAB27A (GS 2), and MLPH (GS 3) genes [4]. GS 2 is the most common mutation seen [5].
We present this case due to the rarity of the disease and to emphasize the involvement of a multidisciplinary team comprising haematologists, anaesthetists, transfusion medicine specialists for efficient management of a patient suffering from GS. The Department of Transfusion Medicine forms the backbone of such a program as it plays a pivotal role right from the screening of both the recipient and the suitable donor for the presence of transfusiontransmitted infections, performing the PBSC harvest cryopreserving the stem cell product if needed, and meeting all the routine and specialized transfusion requirements of the recipients such as providing irradiated or washed products as and when required throughout transplantation.
Case Report
The patient, a 3-year-old boy, was admitted to our hospital in the Bone Marrow Transplant (BMT) unit as a known case of GS with central nervous involvement and primary HLH. He was also a post-COVID-19 recovered case with aspiration pneumonitis and had been treated for Cytomegalovirus (CMV) reactivation.
As per history, the child was born of a non-consanguineous marriage, at the age of 1.5 years. He presented with fever, loose stools, cold and cough, the hypopigmented patch below the right eye and lower lips, silvery grey hair, and mild generalized oedema. He was suspected to be suffering from GS and therefore mutation testing for the same was performed. He was found to harbour a mutation in the RAB27A gene which confirmed the diagnosis of Griscelli’s-2 syndrome. His parents and younger brother were found to be negative for the same mutation. He also had an elder brother who died at 18 months of age owing to an apparent brain infection.
The option of an allogeneic stem cell transplant was discussed with the family. There was no Matched-Related Donor (MRD) in the family. The child was initially planned for a Matched Unrelated Donor (MUD) harvest and transplant but due to the ongoing COVID-19 pandemic, the product could not be procured. At our hospital, the child was first managed for primary HLH following HLH-2004 protocol using a combination of dexamethasone and etoposide.
Later on, the parents of the patient were counselled for a haploidentical PBSC transplantation due to the unavailability of Matched Sibling Donor (MSD) and MUD. After obtaining the consent of the parents, the younger sibling a 1-yearold male was tested and found to be negative for GS mutation and was considered eligible to be the donor for the haploidentical PBSC transplantation with an HLA matching score of 7/10. The risks and benefits of the transplant were explained to the parents. This included the aggressive nature of the disease and the associated high risk due to secondary HLH of the CNS and relapse. The younger sibling i.e., the donor was then put on a mobilization regime, namely injection of Granulocyte-Colony Stimulating Factor (G-CSF) 150 microgram and injection plerixafor 3 mg to increase the mobilization of the CD 34+ hematopoietic progenitor cells in the peripheral blood. The allogeneic PBSC harvest was done the next morning. The equipment used for harvesting the PBSC was Spectra Optia apheresis (System 1 P0 4552, Terumo BCT, Lakewood, CO, USA). A minimum dose of 10 million CD 34+ cells per kg body weight of the recipient had been targeted. The bodyweight of the recipient was 17.7 kg. The vitals of the donor including oxygen saturation was monitored throughout the procedure. During the procedure, continuous I.V. infusion of diluted calcium gluconate was given to the donor to prevent citrate-related side effects. The right femoral vein was used for performing the procedure. The irradiated PRC unit was used to perform the customized priming of the machine. Customized priming is done to reduce the percentage of the donor’s blood in the extracorporeal circuit which further reduces the likelihood of any hypotensive reaction occurring during the harvesting procedure. The extracorporeal volume should not exceed more than 15% of the TBV of an adult donor or more than 10% in the case of a pediatric donor. It is done in cases where the donor weighs less than 25 kg or belongs to the pediatric age group. The desired yield target of 10 million cells per Kg bodyweight of the recipient could not be achieved in the initial sitting and the harvest had to be repeated the next day. The same mobilization regime was repeated for the next day’s PBSC. The details of the procedures performed over two days have been shown in Table 1. No adverse effects on the donor were observed on either of the two occasions while carrying out the harvest. The patient or the recipient was also put under a conditioning regime for the haploidentical HSCT. The regime used was the combination of TTF(±(rATG/Grafalon) i.e., Thiotepa, fludarabine, treosulfan with grafalon. Following a successful PBSC harvest, the product was transfused in two parts under all aseptic conditions. The procedure was uneventful. Prophylaxis against graft versus host disease was done by administering a combination of cyclophosphamide, mycophenolate mofetil, and sirolimus, the doses of which were gradually tapered off.
| Day | Pre-procedure CD34 count (cells/uL) | Total Volume of blood processed (ml) | TBV* | Volume of ACD* used (ml) | Product volume (ml) | CD34 count in product (cells/uL) | Dose of CD34 cells in the product (106/kg body weight of recipient | The total duration of the procedure time (minutes) |
|---|---|---|---|---|---|---|---|---|
| 1 | 156 | 5682 | 5.3 | 575 | 300 | 305 | 5.16 | 431 |
| 2 | Not performed | 6480 | 6.0 | 591 | 288 | 365 | 5.67 | 446 |
| TBV*: Total Blood Volume; ACD*: Anticoagulant Citrate Dextrose | ||||||||
The gradual improvement in the clinical condition of the patient following the transplantation is depicted below in Table 2.
| Day + of transplantation | Clinical condition/development observed in the patient | Remarks |
|---|---|---|
| 1+ | Febrile episodes lasting for one week | Managed using injection paracetamol 300 mg+ i.v. antibiotics+ routine medications |
| 5+ | Febrile neutropenia | Granulocyte donors were screened for the presence of TTIs by CMIA and Rapid test techniques. A crossmatch was also performed using the donor’s red cells and the recipient’s serum sample as a final check for compatibility. |
| 6+ | Granulocyte harvested, transfused to the patient after irradiation. | |
| 14+ | Improved motor skill development. The child was able to stand with support, hold objects vocalize, and responded to sounds and his appetite had also improved. He remained afebrile. | |
| 18+ | Continuous improvement in motor skills and overall health of the patient. | Patient samples sent for chimerism analysis |
| 21+ | 100% donor chimerism established | The patient was discharged in a stable condition with the feeding tube attached as he was not able to take oral feeds. |
The blood samples of the patient had been sent to an outside laboratory for chimerism analysis and 100% donor chimerism had been established on day 21+. Thereafter, the patient has been on regular follow-up in the OPD. The patient’s blood samples (on day +45 and +60) were also sent to the same laboratory to assess for chimerism analysis, and 100% donor chimerism had been reported on each occasion. He has shown a good response to the graft. Continuous improvement has been recorded in the form of achievement of the developmental milestones, improvement in the CNS, and ability to stand without support. The feeding tube has also been removed as the patient is now able to take oral feeds.
Discussion
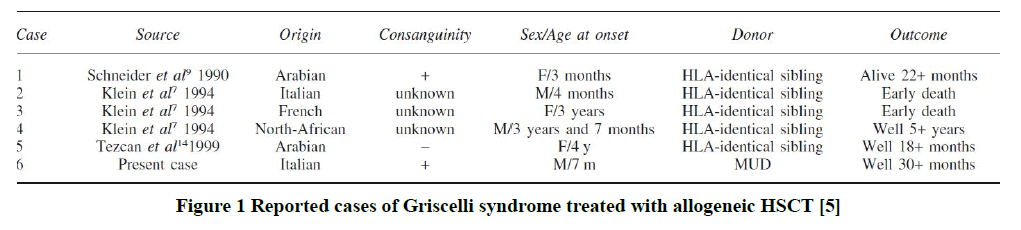
Allogeneic HSCT is the only curative treatment available for genetically induced HLH. As reported by Arico, et al., in their study, few cases of successful HSCT from a compatible donor have been reported in children with GS [5]. The same is shown in Figure 1.
Figure 1. Reported cases of Griscelli syndrome treated with allogeneic HSCT [5]
GS is a rare autosomal recessive disorder. Three genes present on chromosome 15q21 are responsible for GS manifestations [6]. The three types of GS have been identified namely type 1, type 2, and type 3. Each of them has been characterized by its genetic mutation and sign and symptoms [7].
Patients of GS1 have a particularly neurological impairment and normal immune system, while GS2 is mainly characterized by immunological dysfunction with the development of HLH. In GS type 3, unusually light-coloured hair and skin are the only usual presentations. The long-term prognosis of GS is poor and, in most cases, death happens in the first decade of life [8]. In our study, the patient was diagnosed as a case of GS type 2 with isolated CNS involvement and primary HLH and had received treatment as per HLH 2004 protocol. The HLH treatment algorithms targeting hyperinflammation are usually based on pediatric protocols, such as HLH-94 and HLH-2004, which may result in overtreatment and unnecessary toxicity in adults [9].
The child had undergone allogeneic (haploidentical) PBSC transplantation which is the only possible cure for this condition. The recipient had been put on anti-bacterial and anti-fungal medications besides a GvHD prophylaxis using a combination of Post-transplantation Cyclophosphamide (PtCy), sirolimus, and mycophenolate mofetil. The dosages of the same were gradually tapered off.
This was the first time that we had performed allogeneic PBSC transplantation in a case of GS. A multidisciplinary approach is needed to manage such cases right from the time of donor mobilization till post-transplantation care. Detailed testing of the donor for possible GS mutation followed by testing for Transfusion Transmitted Infections (TTIs) namely HIV, Hepatitis B surface antigen, Hepatitis C virus, malaria, and syphilis is imperative before performing the stem cell harvest. As the donor for stem cells was a 1-year-old child, adequate measures were taken by the transfusion medicine team for the stem cell harvest. Customized priming of the apheresis machine was done using PRC to fulfil the requirement of the extracorporeal volume of the machine’s circuit to reduce the likelihood of any possible hypotensive episodes in the donor during the procedure. The PRC used for this purpose was of the same group as that of the donor and crossmatch compatible (AHG phase) with the donor’s serum. The PRC had been irradiated to minimize the possibilities of GvHD. The procedure was uneventful. However, it had to be repeated the next day since the desired targeted yield wasn’t achieved. The possible reason for the same could be donor-related such as an insufficient mobilization of the CD 34+ stem cells. After obtaining the required dose of CD34+stem cells, the transplant was performed the next day. Special care had been taken by providing irradiated cellular components to the recipient following transplantation. The patient had been discharged in a stable condition and complete donor chimerism had been achieved by day 21+ of transplantation. The post-transplantation chimerism analysis was done by Polymerase Chain Reaction (PCR) fragment analysis. Since then, his condition has improved significantly and he is doing well at present with complete donor chimerism as demonstrated in his periodic chimerism analysis reports.
Conclusion
Thus we can conclude that PBSC transplantation in GS when performed promptly with proper care and support can be successful in providing the patient with a new lease of life.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Consent to Participate and Publish
Written, informed consent was obtained from the patient at the time of admission that the data may be used for any research or academic purposes.
No harm was brought to the patient during the study. There were no animal subjects involved during the study period.
Funding Sources
No funding was obtained for any aspect of the study.
References
- Kharkar, Vidya, et al. "Griscelli syndrome: A new phenotype with circumscribed pigment loss?" Dermatology Online Journal, Vol. 13, No. 2, 2007.
Google Scholar Crossref - Sheela, S. R., Manoj Latha, and Susy J. Injody. "Griscelli syndrome: Rab 27a mutation." Indian Pediatrics, Vol. 41, No. 9, 2004, pp. 944-47.
Google Scholar Crossref - Carter, P. Gonzalez, et al. " Griscelli-Prunieras syndrome: Report of two cases." Annals of Pediatrics, Vol. 70, No. 2, 2009, pp. 164-67.
Google Scholar Crossref - Bizario, Joao, et al. "Griscelli syndrome: Characterization of a new mutation and rescue of T-cytotoxic activity by retroviral transfer of RAB27A gene." Journal of Clinical Immunology, Vol. 24, No. 4, 2004, pp. 397-410.
Google Scholar Crossref - Rajyalakshmi, R., and R. N. Chakrapani. "Griscelli syndrome type 2: A rare and fatal syndrome in a South Indian boy." Indian Journal of Pathology & Microbiology, Vol. 59, No. 1, 2016, pp. 113-16.
Google Scholar Crossref - Durmaz, Asude, et al. "Molecular analysis and clinical findings of Griscelli syndrome patients." Journal of Pediatric Hematology/Oncology, Vol. 34, No. 7, 2012, pp. 541-44.
Google Scholar Crossref - Szczawinska-Poplonyk, Aleksandra, et al. "Pulmonary lymphomatoid granulomatosis in Griscelli syndrome type 2." Viral Immunology, Vol. 24, No. 6, 2011, pp. 471-73.
Google Scholar Crossref - Nejad, Seyed Ebrahim Mansouri, et al. "Griscelli syndrome: A case report." Iranian Journal of Child Neurology, Vol. 8, No. 4, 2014, pp. 72-75.
Google Scholar Crossref - Ishii, Eiichi. "Hemophagocytic lymphohistiocytosis in children: Pathogenesis and treatment." Frontiers in Pediatrics, Vol. 4, 2016, p. 47.
Google Scholar Crossref