Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 12
A Systematic Review of Complications during Insertion of Central Venous Catheterization Guided by Ultrasound versus and Anatomical Landmark
Hassan Shaaib*, Abdulrahman Al-Otaibi, Abdul Karim Antar Al-Otaibi, Ahmed Ali Alshamrani, Majed Ahmed Alqarni, Ibrahim Omran Mahzri and Hatem Maqbool AlkhaldiHassan Shaaib, Department of Anesthesia Technology, Prince Sultan Military College of Health Sciences, Saudi Arabia, Email: hshuaaieb@psmchs.edu.sa
Received: 16-Nov-2020 Accepted Date: Dec 21, 2020 ; Published: 28-Dec-2020
Abstract
Background: Central Venous Catheter (CVC) is an interventional procedure used during anesthesia and critical care for the administration of drugs, fluids and to measure blood pressure as well as other medical uses. There are two methods for the insertion of a Central Venous Catheter, ultrasound imaging, and anatomical landmarks. The CVC is inserted into a central vein such as the internal jugular, Subclavian, and femoral veins in sterile procedures with as few attempts as possible to reduce complications. Objective: The study aimed to review the incidence of complications during the insertion of central venous catheterization guided by ultrasound versus an anatomical landmark. Methodology: The researchers collected papers that met the criteria and were already published in databases, i.e., the Wiley digital library, Scopus, PubMed, Google Scholar, and Cochrane Databases in the period of (2000-2020). The sample consisted of 25 articles. Mesh headings searched included ultrasound, anatomical landmark, central venous cannulation, and complications. Result: Findings of 24 (96%) Randomized Controlled Trials (RCT) in different parts of the world revealed that the ultrasound imaging method has fewer complications than anatomical landmark during central venous cannulation, A p-value <0.05, and only 1(4%) study showed the insignificance with the p-value is >0.05. Conclusion: According to all previous studies, the review concluded that ultrasound imaging is more effective in reducing complications compared to the anatomical landmark technique in patients requiring central venous catheter insertion. And this review is recommending further studies to discover other factors that can reduce the complications.
Keywords
Central venous catheter, Complications, Ultrasound, Anatomical landmark
Introduction
Central venous cannulation is commonly indicated in the care of critically ill patients for various purposes. Anyhow, this routine procedure has complications that every provider should recognize, consider, and be able to manage, either directly or with immediate specialized assistance. Complications can occur at the time of catheter insertion and include vascular, cardiac, pulmonary, and placement complications. Late complications include dysfunction and infection of the device. Peripherally inserted central venous access has an altered complication profile that clinicians should consider when deciding on central venous access but are still associated with the same spectrum of complications as the centrally placed catheter [1].
A Central Venous Catheter (CVC) is a tube placed into a large vein in the Subclavian, internal jugular, and femoral veins. The purpose of this tube is to administer medication or fluids that are unable to be taken by mouth and measure Central Venous Pressure (CVP) for critically ill patients or in major surgical cases. There are different types of central venous catheter used for a different purpose, which is a single lumen and multiple lumens (double or triple lumen). Single lumen is for insertion only medications or fluids. Multiple lumens are for injection of drugs, intravenous fluids, and Central Venous Pressure (CVP) monitoring. A central line pertains to a catheter inserted into a central vein such as the internal jugular, Subclavian, and femoral veins for purposes of diagnosing and treating critically ill patients [2].
The use of ultrasound guidance in central venous catheterization is based on recommendations agreed by many medical societies and government agencies. i.e., the Agency for Healthcare Research and Quality, the National Institute for Health and Clinical Excellence in the UK, the American Society of Echocardiography, and the Society of Cardiovascular Anesthesiologists. Despite these recommendations, the use of ultrasound for central venous catheterization are still very low [3].
Central venous catheterization is frequent in use and essential medical intervention. Despite its regular practice, it is still linked with a high incidence of complications, especially infection and catheter tip embolization. The addition of ultrasound guidance to the technique has proved significant change to the better regarding the time and number of attempts for successful catheterization [4].
A sterile procedure must be performed successfully with as few attempts as possible. to avoid adverse consequences including hematoma from mistakenly puncturing the artery instead of a vein, infection, pneumothorax from puncture of the lungs, thrombosis, embolism, vena cava laceration, and nerve injury [1].
A lot of benefits are gained from the use of ultrasound as a real-time guiding the Central Venous Catheters (CVCs) when it is compared with landmark techniques for the placement of (CVCs). These include faster procedure times as well as lower complication rates [5].
The likelihood of the complications depends on the characteristics of the patient, clinician expertise, the care environment, and the risks inherent in the procedure. Central vein catheters have traditionally been inserted by using anatomical landmarks. There are three main veins for insertion Central vein catheter that are subclavian, Internal Jugular (IJV), and femoral CVC insertions. The left IJV cannulation is more time-consuming. When compared to other cannulation sites, left IJF is associated with a higher incidence of complications. The use of ultrasound improves the success rate and decreases the number of complications during Internal Jugular Venous (IJV) cannulation [6].
Many studies agreed that dynamic and static US guidance during central venous catheter insertion was connected with improved first cannulation attempts and in general success rates of introduction by junior residents [7].
Previously, CVC placement is performed using landmark techniques based on the knowledge of anatomic structures and palpation of arteries next to the veins. These landmark techniques cannot account for anatomic variations at the CVC insertion site. Anatomic changes to the “normal anatomy,” however, have been described in a relevant proportion of patients for the Internal Jugular Vein (IJV), the Subclavian Vein (SV), and the Femoral Vein (FV) [4].
For many years the landmark technique has been accepted as a standard approach for CVC. Still, literature has challenged this practice and caused an ideal shift toward ultrasound-guided intravenous access. Nevertheless, the anatomic landmark method is a common practice among pediatric surgeons. However, they know it does not allow for accurate visualization of the vein and the surrounding structures and increasing the risk of complications. The American College of Surgeons supports the use of ultrasound in central venous catheter placement in the adult population; however, this concept is not globally [8].
Many techniques have been nominated to decide a proper insertion depth of the Central Venous Catheter (CVC). Among the methods, the carina is recommended as a useful target level for the CVC tip position. And a lot of studies evaluated the sternal head of a right clavicle and the nipples as anatomic landmarks for determining the optimal depth of CVC [9].
Ultrasound imaging (US) can be used in different ways to facilitate CVC placement. Static US (also called the indirect US) describes a technique using ultrasound only before CVC placement to identify the anatomy of the target vein (mapping) and adjacent anatomic structures (including the patency of the vein and its dimensions and depth from the skin) [9].
On the opposite, real-time US (also called the direct US) pronounce a skill of needle insertion and vessel puncture under continuing US control (i.e., the needle is always visualized on the US screen). It is also referred to as “US guidance” [10].
Although the placement of a Central Venous Catheter (CVC) is a routine procedure in intensive care medicine and anesthesiology, severe acute complications (such as arterial puncture or cannulation, hematoma, hemothorax, or pneumothorax) occur in a relevant proportion of patients [9].
Cannulation of the internal jugular or femoral vein by inexperienced residents when it is guided by ultrasound appears to be more reliable than the Landmark (LM) or other methods and was associated with a lower mechanical complication rate among ICU patients [11].
Ultrasound-guided intravenous access, whether peripheral or central, can reduce procedural time and complications, and is associated with higher satisfaction. Obtaining venous access is often a vital component of emergency department patient care, in patients with difficult venous access, or who urgently require central venous access for therapy and resuscitation [12].
Proper methods in any clinical practice are one of the fewer complications, and this study assures, using an ultrasound technique for central venous cannulation will achieve the benefit. This technique may result in fewer adverse events compared to the landmark approach. The studies conducted in this area have investigated the complications of central venous catheters individually and compare the incidence of these complications when using ultrasound versus anatomical landmarks. This systematic review study aims to review the difficulties of central venous cannulation and associate them with ultrasound versus anatomical landmark techniques.
Methods
Inclusion Criteria
This study is running based on the guideline for conducting systematic review studies (Cochran) and using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [13]. The study included all randomized control studies published in peer-reviewed journals. Only the papers in English which had examined the complications of central venous cannulation either by ultrasound-guided technique or anatomical landmark approaches were included. The minimum sample size of the reviewed documents was 25.
The main objective of this study was to compare the complications of CVC when using the ultrasound versus the anatomical landmark approach.
Search Strategy
In the current study, the international databases (Wiley library, PubMed, Google Scholar were searched from the time of 2000 until July 30, 2020. The keywords were used based on Medical Subject Headings (MESH) and Emtree and then merged. The keywords used in English included ultrasound, anatomical landmark, central venous cannulation, and complications.
Selecting the Studies and Extracting Information
According to the study protocol and the inclusion criteria, two of the researchers investigated the title and abstract of the studies separately, and then the repeated cases were eliminated. In the next stage, the full text of the papers was examined, and the necessary information was extracted. In cases where a disagreement occurred for selecting the studies, a consensus method was used to resolve the dispute between the writers. The items of the extracted information included general information (first author, year, country, sample size, data collection method), and the search consists of (complications of insertion of central venous catheter by ultrasound imaging versus anatomical landmark technique).
Quality of Studies
Investigation on the quality of studies was performed using the Jadad scale for reporting randomized controlled trials. The main advantages of this scale are that it is easy to use; it contains many of the essential elements that have empirically been shown to correlate with bias, and it has known reliability and external validity [14,15].
Results
Assortment of Studies
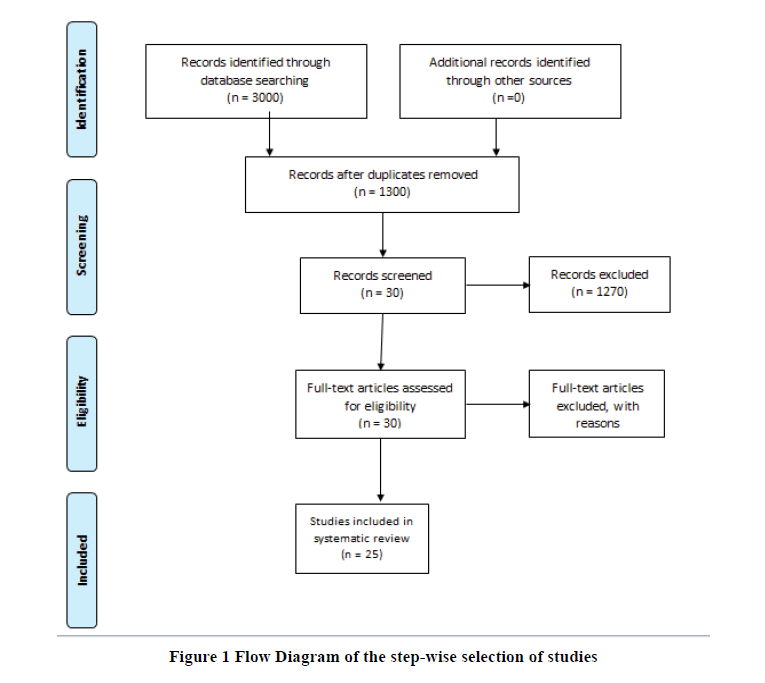
Based on the keyword search across different databases, the researchers found more than 3000 papers, out of which 1300 were non-repeated. In the next step, the study investigated the non-repeated documents based on their title and abstract and removed bout 1270 papers. In the next stage, the team of researchers found 30 articles, and 25 Randomized controlled trials entered the final step. The team excluded five documents at this stage, and the rest included studies that had been conducted in different parts of the world internationally (Figure 1). In the final stage (n=25), randomized controlled studies composed of 5301 participants (Table 1).
| Studies References | Nation | Design | No. of patients | UL group | LA group | p-value |
|---|---|---|---|---|---|---|
| 1. (7) | USA | RCT | 115 | 57 | 58 | <0.01 |
| 2. (16) | Egypt | RCT | 100 | 50 | 50 | <0.05 |
| 3. (17) | Turkey | RCT | 380 | 190 | 190 | <0.01 |
| 4. (18) | Turkey | RCT | 584 | 292 | 292 | =0.04 |
| 5. (19) | Iran | RCT | 321 | 160 | 161 | =0.04 |
| 6. (20) | India | RCT | 60 | 30 | 30 | <0.05 |
| 7. (21) | Italy | RCT | 148 | 74 | 74 | 0.001 |
| 8. (22) | Pakistan | RCT | 60 | 30 | 30 | =0.024 |
| 9. (23) | Nepal | RCT | 120 | 60 | 60 | =0.001 |
| 10. (24) | Jordan | RCT | 203 | 101 | 102 | <0.001 |
| 11. (25) | Turkey | RCT | 100 | 50 | 50 | <0.05 |
| 12. (3) | Macedonia | RCT | 400 | 200 | 200 | =0.0008 |
| 13. (8) | The USA. | RCT | 150 | 75 | 75 | =0.0001 |
| 14. (11) | France | RCT | 118 | 59 | 59 | =0.01 |
| 15. (5) | Germany | RCT | 157 | 78 | 79 | <0.0001. |
| 16. (26) | China | RCT | 214 | 107 | 107 | <0.05 |
| 17. (27) | Turkey | RCT | 100 | 50 | 50 | =0.041 |
| 18. (28) | Romania | RCT | 60 | 30 | 30 | <0.05 |
| 19. (29) | Nepal | RCT | 111 | 58 | 53 | =0.001 |
| 20. (30) | Greece | RCT | 900 | 450 | 450 | <0.001 |
| 21. (31) | India | RCT | 450 | 225 | 225 | =0.04 |
| 22. (32) | Egypt | RCT | 100 | 50 | 50 | <0.05 |
| 23. (33) | Egypt | RCT | 60 | 30 | 30 | <0.05 |
| 24. (34) | Iran | RTC | 200 | 100 | 100 | <0.0001 |
| 25. (35) | Iran | RTC | 90 | 45 | 45 | =0.750 |
| Total | 5301 | 2651 | 2650 | |||
Table 1: Key Feature of the selected studies that compare the ultrasound versus anatomical landmark in reducing complications of central venous cannulation
Discussion
The present systematic review was conducted to compare the complications of Central Venous Catheterization (CVC) among ultrasound-guided methods versus anatomical landmarks. By using international databases from 2000 until July 30, 2020, the present study found ultrasound methods reduced the complications as compared with the anatomical landmarks. After recorded and analyzed all papers we found out, 25 Randomized Controlled Trials (RCT) studies, which include 5795 patients, examined the complications occurring with ultrasound imaging versus an anatomical landmark technique for central venous catheterization.
Brass et al., in Germany, demonstrated a Randomized and quasi-randomized controlled trial for comparing twodimensional ultrasound or Doppler ultrasound versus an anatomical ‘landmark’ technique. During the insertion of subclavian or femoral venous catheters to evaluate by using both methods, the study results showed the ultrasound technique offers small benefits in safety and quality when compared with an anatomical landmark technique [2].
In contrast to the previous study in Iran, Fathi et al., pull out a comparison between central venous cannulation of the internal jugular vein using ultrasound-guided and anatomical landmark-guided techniques. Patients undergoing the study were randomly divided into two groups According to the results of this study, under current conditions and due to limited resources and a lack of adequate training, the use of anatomical landmarks will continue to be the preferred method of treatment in Iran [16].
Turker et al., supported the same idea in Turkey when they compared the landmark-guided technique versus the ultrasound-guided method for internal jugular vein cannulation in spontaneously breathing patients. Patients who required internal jugular vein cannulation were randomly assigned. They received the cannulation either by using the landmark- or ultrasound-guided technique. The researchers recorded a failed catheter placement, some complications, the number of attempts, and the time to successful catheterization, as well as the demographics of each patient. The result showed a higher complication rate in the landmark group than in the ultrasound-guided group (p<0.01) [17].
This another study in which Kayir et al., in Turkey, evaluate the effectiveness of needle-guiding ultrasound for internal jugular venous cannulation compared with the landmark. Patients were divided into two groups. Group U for catheterization with ultrasound guidance and Group L are performed with the anatomic landmark technique. The rate of success in the procedure and the frequency of complications for both methods were compared. Group U produced success and complication rates significantly better than Group L, the landmark technique (p=0.04 and p=0.00001, respectively). This study illustrated that the use of ultrasonography reduced complication rates as compared to the landmark technique [18].
The advantages of ultrasound-guided central venous catheter insertion over the anatomical landmark technique regarding ease of insertion and safety are determined in Pakistan. Patients in the study were selected and randomly divided into two groups; the central catheter was inserted under aseptic conditions, and including ease of access, several attempts, arterial punctures, and other complications in both groups were recorded. Result: Ultrasound guidance resulted in statistically significant comfort of insertion (p=0.024) While decreasing the attempts to gain venous access as compared to the anatomical landmark group (p=0.0453). Two cases of arterial puncture were recorded in the anatomical landmark group, while no arterial puncture occurred in the ultrasound group. Conclusion: Ultrasound guidance for central catheter insertion makes it easy and safe as it allows better identification of vascular structures. It also reduces the rate of complications associated with central catheter insertion and improves the success rate, thereby justifies its cost [19].
Youssef et al., Egypt, compare the outcome of an ultrasound-guided technique versus an anatomical landmark-guided technique for central venous catheterization. Patients were assigned into two groups (A) and (B), respectively, and the study stated the use of ultrasound-guided central venous catheterization has better results and higher-safety in comparison to anatomical landmark-based technique, as well as the mechanical complications in which significantly lower [20].
During 2019 in Italy, a study compared the effectiveness of a real-time ultrasound with a landmark-guided technique for the subclavian vein. Two groups of 74 consecutive patients were recruited, each undergoing subclavian vein catheterization. One group included patients from the intensive care unit, studied by using an ultrasound-guided technique. The other group included patients from surgery or emergency units, considered by using a landmark technique. As a result, confirmed the use of an ultrasound-guided technology for Subclavian catheterization offers advantages in terms of a reduced number of attempts and complications [21].
In India, they determined if US guidance could be successful in the number of attempts and rates of acute complications when patients were prospectively randomized in two groups of 30 each LM and US. The number of attempts, success rate, access time and difficulties, were noted by US guidance during Subclavian vein catheterization in the firstattempt with success and improves access time with a reduced average number of attempts and complications [22].
A study conducted by Shrestha et al., in Nepal, to find out if an ultrasound technique has advantages over the conventional landmark technique in a prospective randomized comparative study. The outcome measures were compared between the groups. In conclusion, the survey agreed with ultrasound for the success rate besides minimizes the time and complications during internal jugular vein cannulation. It can be referred to as a rescue technique in cases of a failed landmark technique [23].
In contrast, in most of the studies about the benefit of ultrasound methods, Iranians, recently stated that neither of the ways of ultrasound guidance and anatomical landmarks had a significant superiority in terms of the success rate. And the complications of insertion the reason for the absence of a substantial difference between the two groups in the above parameters were the anesthesia residents’ insufficient personal skills in performing the ultrasound [24].
Recently in Jordan 2020, a study showed real-time ultrasound-guided Central Venous Catheterization (CVC) when demonstrated, can reduce insertion and procedure time as well as having fewer complications compared to the landmark technique. The technique was newly introduced to Jordan University Hospital. They concluded the ultrasound method could increase the efficiency and reduce the complications which justify the costs of implementing this technique [25-33].
Conclusion
According to all previous studies, the review concluded that ultrasound imaging is more effective in reducing the number of insertion attempts, complication, compared to the anatomical landmark technique in patients requiring central venous catheter insertion. The findings of this study can be effectively implemented in the clinical practice of central venous cannulation.
Recommendations
The research team, based on the recommendations taken from the previous RCT, encourages the use of ultrasoundguidance for central venous access to achieve the best practice with low complications and applies training of anatomic landmark techniques, especially in junior practitioners.
Ethical approval
The manuscript is a systematic review, and it does not involve human subjects and hence the need for ethical approval
Declerations
Conflict of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Kornbau, Craig, et al. "Central line complications." International Journal of Critical Illness and Injury Science, Vol. 5, No. 3, 2015, pp. 170.
- Brass, Patrick, et al. "Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization." Cochrane Database of Systematic Reviews, No. 1, 2015.
- Sazdov, Darko, Marija Jovanovski Srceva, and Zorka Nikolova Todorova. "Comparative analysis of ultrasound guided central venous catheterization compared to blind catheterization." Prilozi, Vol. 38, No. 2, 2017, pp. 107-14.
- Hoffman, Taryn, et al. "Ultrasound-guided central venous catheterization: A review of the relevant anatomy, technique, complications, and anatomical variations." Clinical Anatomy, Vol. 30, No. 2, 2017, pp. 237-50.
- Maecken, T., et al. "Ultrasound-guided catheterisation of the subclavian vein: freehand vs needle-guided technique." Anaesthesia, Vol. 70, No. 11, 2015, pp. 1242-9.
- Sulek, Cheri A., Mark L. Blas, and Emilio B. Lobato. "A randomized study of left versus right internal jugular vein cannulation in adults." Journal of Clinical Anesthesia, Vol. 12, No. 2, 2000, pp. 142-5.
- Dodge, Kelly L., et al. "Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents." Journal of Ultrasound in Medicine, Vol. 31, No. 10, 2012, pp. 1519-26.
- Bruzoni, Matias, et al. "A prospective randomized trial of ultrasound-vs landmark-guided central venous access in the pediatric population." Journal of the American College of Surgeons, Vol. 216, No. 5, 2013, pp. 939-43.
- McGee, David C., and Michael K. Gould. "Preventing complications of central venous catheterization." New England Journal of Medicine, Vol. 348, No. 12, 2003, pp. 1123-33.
- Dietrich, Christoph F., et al. "Ultrasound-guided central vascular interventions, comments on the European Federation of Societies for Ultrasound in Medicine and Biology guidelines on interventional ultrasound." Journal of Thoracic Disease, Vol. 8, No. 9, 2016, pp. E851-68.
- Airapetian, Norair, et al. "Ultrasound-guided central venous cannulation is superior to quick-look ultrasound and landmark methods among inexperienced operators: a prospective randomized study." Intensive Care Medicine, Vol. 39, No. 11, 2013, pp. 1938-44.
- Panebianco, Nova L. "Ultrasound-guided vascular access." Emergency Point-of-Care Ultrasound, 2017, pp. 287-95.
- Jefferies, Diana, et al. "The importance of academic literacy for undergraduate nursing students and its relationship to future professional clinical practice: A systematic review." Nurse Education Today, Vol. 60, 2018, pp. 84-91.
- Halpern, Stephen H., and M. Joanne Douglas. "Appendix: Jadad scale for reporting randomized controlled trials." Evidence-based Obstetric Anesthesia. Oxford, UK: Blackwell Publishing Ltd, 2005, pp. 237-8.
- Halpern, Stephen H., and M. Joanne Douglas, eds. "Evidence-based obstetric anesthesia." John Wiley & Sons, 2008.
- Fathi, Mehdi, et al. "Central venous cannulation of the internal jugular vein using ultrasound-guided and anatomical landmark techniques." Anesthesiology and Pain Medicine, Vol. 6, No. 3, 2016 pp. e35803.
- Turker, Gurkan, et al. "Internal jugular vein cannulation: an ultrasound-guided technique versus a landmark-guided technique." Clinics, Vol. 64, No. 10, 2009, pp. 989-92.
- Kayir, Selcuk, et al. "Internal jugular vein catheterization: The landmark technique versus ultrasonography guidance in cardiac surgery." Cureus, Vol. 11, No. 2, 2019, pp. e4026.
- Rehman, Abdul, Huma Zeb, and Abid Ullah Khan Niazi. "Ultrasound guidance increases the safety and ease of insertion of central venous catheters in patients undergoing elective procedures." Anaesthesia, Pain & Intensive Care, Vol. 19, No. 4, 2019, pp. 474-7.
- Yousef, Ayman A., et al. "An Ultrasound Guided Technique of Central Venous Catheterization versus Anatomical Landmark Guided Technique in Medical Intensive Care Patients." The Egyptian Journal of Hospital Medicine, Vol. 72, No. 4, 2018, pp. 4236-40.
- Sidoti, Anna, et al. "Ultrasound-versus landmark-guided subclavian vein catheterization: a prospective observational study from a tertiary referral hospital." Scientific Reports, Vol. 9, No. 1, 2019, pp. 1-7.
- Singam, Amol P., Ashok Chaudhary, and Shruti Shrey. "Anatomical Landmark Guided versus Ultrasound-Guided Technique for Subclavian Vein Cannulation in Critically Ill Patients." Journal of Krishna Institute of Medical Sciences (JKIMSU), Vol. 8, No. 4, 2019, pp. 50-7.
- Shrestha, Babu Raja, and B. Gautam. "Ultrasound versus the landmark technique: a prospective randomized comparative study of internal jugular vein cannulation in an intensive care unit." Journal of the Nepal Medical Association, Vol. 51, No. 182, 2011, pp. 56-61.
- Faiz, Seyed Hamid Reza, et al. "Comparison Between Ultrasound Guidance and the Landmark Technique for the Internal Jugular Vein Cannulation in Adult Patients by Anesthesia Residents or Inexperienced Operators." Iranian Heart Journal, Vol. 19, No. 3, 2018, pp. 30-7.
- Akelma, Hakan, et al. "A comparison of the rates of success and complications in the application of central venous catheters applied with ultrasonography or the landmark method." Harran Üniversitesi Tıp Fakültesi Dergisi, Vol. 16, No. 2, 2019, pp. 250-6.
- Miao, Jianzhong, et al. "Randomized clinical trial comparing ultrasound-guided procedure with the Seldinger’s technique for placement of implantable venous ports." Cell Biochemistry and Biophysics, Vol. 70, No. 1, 2014, pp. 559-63.
- Dolu, Hasan, et al. "Comparison of an ultrasound-guided technique versus a landmark-guided technique for internal jugular vein cannulation." Journal of Clinical Monitoring and Computing, Vol. 29, No. 1, 2015, pp. 177-82.
- Mitre, Clin I., et al. "Ultrasound-guided external jugular vein cannulation for central venous access by inexperienced trainees." European Journal of Anaesthesiology (EJA), Vol. 27, No. 3, 2010, pp. 300-3.
- Karakitsos, Dimitrios, et al. "Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients." Critical Care, Vol. 10, No. 6, 2006, pp. 1-8.
- Palepu, Gopal B., et al. "Impact of ultrasonography on central venous catheter insertion in intensive care." The Indian Journal of Radiology & Imaging, Vol. 19, No. 3, 2009, pp. 191-8.
- Saleh, Abdelwahab A., Alaa El-Din M. Sayed, and Abdallah M. Ahmed. "Comparative study between ultrasound-guided internal jugular venous catheter insertion versus conventional method in children." Al-Azhar Assiut Medical Journal (AAMJ), Vol. 12, No. 4, 2014, pp.322-38.
- Montazar, Seyyed Hosein, et al. "Comparison of Complications and the Rate of Success of Central Venous Catheters with Ultrasound Guidance or Conventional Methods in Emergency Department." International Journal of Medical Investigation, Vol. 7, No. 2, 2018, pp. 21-9.
- Bani Hani, Amjad et al. “The Effectiveness of Real-Time Ultrasound-Guided Central Venous Catheterization: A Comparison with the Landmark Technique in Jordanian Patients.” Research Journal of Medical Sciences, Vol. 13, No. 6, 2020, pp. 109-14.