Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 4
A Study on Etiology and Clinical Pr ofile of Respiratory Distress among Neonates Received in NICU at a Tertiary Care Centre in Hyderabad
Mohammad Kamil Ahmed, C.V.S. Lakshmi* and Uppin Narayan ReddyC.V.S. Lakshmi, Department of Pediatrics, Princess Esra Hospital, Deccan College of Medical Sciences, Hyderabad, Telangana, India, Tel: 040- 24340169, Email: lakshmicvsdr@gmail.com
Received: 25-Mar-2021 Accepted Date: Apr 20, 2021 ; Published: 27-Apr-2021, DOI: o
Abstract
Background: Respiratory distress is the most frequent cause of admission in neonatal intensive care in both term and preterm infants. The clinical presentation of respiratory distress can vary from mild to severe respiratory distress requiring mechanical ventilation, and also depends on the respiratory support received before referral to a higher center. The etiology for respiratory distress depends on fetal, maternal, and environmental risk factors, and also on gestational age and birth weight. Objectives: This study was performed to assess and analyze the risk factors, etiology, clinical profile, morbidity, and mortality of neonates admitted with respiratory distress in NICU. Methods: This was a prospective study was done on 292 neonates admitted to Neonatal Intensive Care Unit (NICU) with respiratory distress. General information, socioeconomic status, detailed perinatal history, and clinical examination were documented. Results: 292 neonates admitted with respiratory distress were included in the study. Around 151 (51.7%) babies were born prematurely. The mode of delivery was LSCS in 254 (87.16%) neonates. The most important risk factors were delivery by Cesarian section and maternal infection (49%). Transient tachypnea of the newborn (45.2%), Congenital pneumonia (22.2%), and Late-onset sepsis (10.9%) were the most common causes of respiratory distress. 32.1% of these infants required respiratory support in the form of invasive and non-invasive ventilation. Only 3 infants (1.03%) of infants expired during the study period, due to severe RDS and late referral to the hospital. Conclusion: The most important risk factors for respiratory distress are delivery by Cesarian section and maternal infection. Early referral and early respiratory support help in better outcomes.
Keywords
Neonates, NICU, Respiratory distress, Cesarean section, Respiratory support
Abbreviations
NICU: Neonatal Intensive Care Unit, SPO2: Saturation of Oxygen, TTNB: Transient Tachypnoea of New-Born, CPAP: Continuous Positive Airway Pressure, NIPPV: Non-Invasive Positive Pressure Ventilation
Introduction
Respiratory distress is among the most important reasons for admission to a neonatal intensive care unit. 15% of term infants and 29% of late preterm infants admitted to the neonatal intensive care unit experience significant respiratory morbidity [1]. Premature neonates are also more likely to be admitted, i.e. neonates born before 34 weeks of gestation. According to research conducted in JIPMER, Pondicherry, Preterm infants had the highest incidence (30%) followed by post-term infants (20.9 %) and term babies 4.2% [2].
Respiratory distress in a new-born is recognized as one or more signs of the increased breathing activity, such as tachypnea, nasal flaring, chest retraction, or grunting. Normally, the respiraatory rate of new-born respiration is between 40 and 60 breaths per minute [1]. Tachypnea is characterized as a respiratory rate of more than 60 breaths per minute. Tachypnea is a mechanism of compensation for hypercarbia, hypoxemia, or acidosis (both metabolic and respiratory, making it a normal, but nonspecific, finding in large in a large variety of cardiovascular, metabolic, or systemic diseases [3,4].
Factors that raise the risk of neonatal respiratory disorders include respiratory distress syndrome, intermittent neonatal tachypnea, meconium aspiration syndrome, air leakage, pulmonary hemorrhage, pulmonary edema, congenital structural lung or thoracic defects, etc. Non-respiratory causes of respiratory distress include metabolic disorders such as hypothermia or hyperthermia, hypoglycemia, polycythemia, cardiac disorders, birth asphyxia, metabolic acidosis, and various inborn errors of metabolism [5-8].
The clinical presentation of respiratory distress in the newborn includes apnea, cyanosis, expiratory grunting, inspiratory stridor, nasal flaring, poor feeding, and tachypnea (more than 60 breaths per minute) [9]. The severity of respiratory distress can be assessed by using objective scoring systems like Downes score for term infants, and the Silverman Anderson scoring system for both term and preterm infants. Initial evaluation of respiratory distress includes vital parameter monitoring including SPO2, detailed general physical and systemic examination to rule out non-respiratory causes of respiratory distress, Chest X-ray, blood sugar, complete blood picture, and sepsis screen evaluation. It is advisable to place a nasogastric tube before ordering a chest X-ray to rule out anatomical malformations like tracheaesophageal fistula. Further assessment is based on the interpretation of the above basic investigations.
The respiratory distress, if not identified promptly and treated can lead to respiratory failure and cardiopulmonary arrest. Therefore, the neonatologist needs to identify the risk factors, signs, and symptoms of respiratory distress for early diagnosis and treatment which has the potential to prevent mortality among neonates.
Aims and Objectives
• To study the maternal, perinatal, and neonatal risk factors for respiratory distress
• To study the etiology, clinical course, and immediate outcome of infants admitted with respiratory distress
Materials and Methods
This was a prospective study conducted during one year in a level 3 NICU in a tertiary care hospital in semi-urban Hyderabad, India. 502 neonates were admitted to the NICU during the one-year study period from November 2019 to October 2020 at Princess Esra Hospital, Hyderabad, India, of which 292 infants presented with signs of respiratory distress. A written, well-informed consent was taken from the parents before enrollment into the study, Maternal and neonatal data were collected in predesigned and pretested proforma. Infants whose parents did not give consent for the study, and who left the hospital against medical advice before recovery were excluded from the study. Data was collected for all newborns included in the study with respiratory distress. General information, socioeconomic status, detailed history, including antenatal, intrapartum, and postnatal, including risk factors for sepsis, steroid coverage, antenatal scans, singleton or multiple gestations, and mode of delivery was recorded. At admission, a detailed physical examination including vitals, SPO2, Blood sugar, general physical examination, gestational assessment using New Ballard’s score, and clinical examination findings of these neonates was documented in a predesigned proforma. The basic evaluation included Chest X-ray and sepsis screen (Total leucocyte count, Absolute leucocyte count, I/T ratio, and CRP). Additional investigations like blood culture and other related investigations were done based on the diagnosis. The diagnosis, complications during NICU stay, and the outcome was duly recorded. The outcome measure was either in-hospital death (expired infants) or survival was defined as discharge of baby alive from the hospital (survivors).
Inclusion Criteria
• Neonates with symptoms of respiratory distress
• Infants whose parents are willing to give consent
Exclusion Criteria
• Neonates who were discharged against medical advice
• Neonates whose parents refused consent for participation in the study
Statistical Analysis
Using Microsoft Word, Microsoft excels and Epi Info 7 Statistical analysis was done.
Ethical Approval
Approval from the Institutional review board was obtained before the study was initiated.
Results
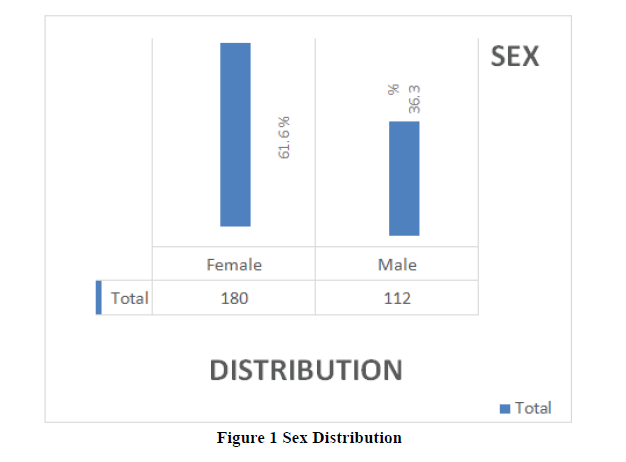
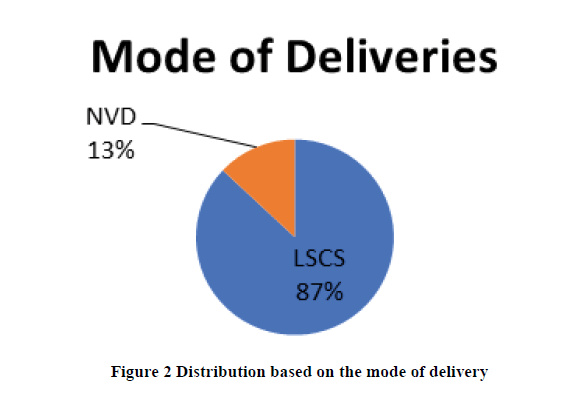
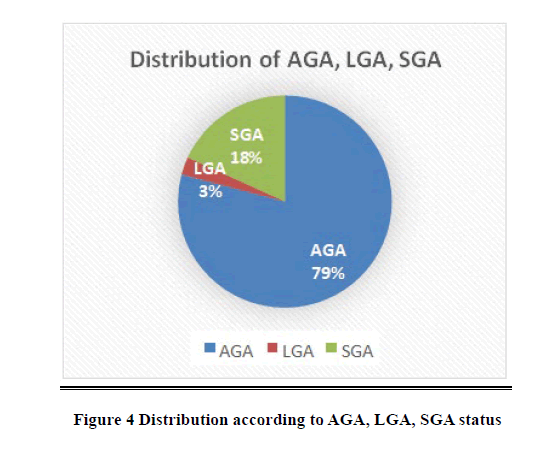
Out of 502 neonates admitted to the NICU during the study period, n=210 (41.8%) did not need any respiratory support while n=292 (58.16%) had signs of respiratory distress and they were studied. Out of the n=292, n=112 (38.36%) were males and n=180 (61.64%) were female as shown in Figure 1. The birth weight was appropriate to gestational age in n=231 (79.1%), large for gestational age in n=11 (3.76%), small for gestational age in n=50 (17.12%). Around n=151 (51.7%) babies were born prematurely. The mode of delivery was LSCS in n=254 (87.16%) neonates.
The mode of deliveries was found to be 13% in the LSCS while the majority of the deliveries has occurred via NVD around 87% shown in Figure 2.
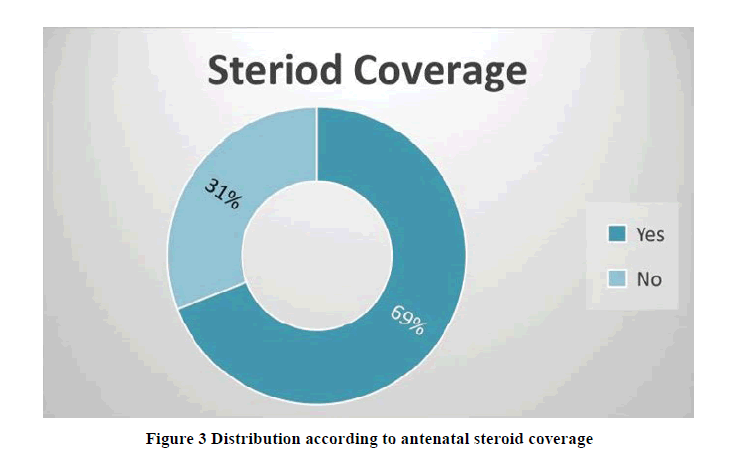
It was observed that most the pregnant mothers during the antenatal period are the steroid coverage which was found to be 69.%, while the pregnant mothers not on the steroid coverage was 31% as shown in Figure 3.
It was observed that majority of gestational age at delivery was found to be (n=78) 36.54% at 35 to 37 weeks. While the lowest less than 30 weeks with (n=14) 4.86% as detailed in Table 1.
Table 1 Distribution according to gestational age
| S. No. | Gestational age at delivery | Frequency | Percentage |
|---|---|---|---|
| 1 | <30 weeks | 14 | 4.86% |
| 2 | 31-34 weeks | 45 | 15.90% |
| 3 | 35-36 weeks | 77 | 26.54% |
| 4 | 37 weeks | 78 | 26.54% |
| 5 | 38 weeks | 61 | 20.79% |
| 6 | 39 weeks and above | 17 | 5.82% |
| 7 | Total | 292 | 100.00% |
The study reveals that the birth weight ranging between 2.5 to 4 kgs was found in (n=107) 26.54% of the babies, while (n=101) which is 15.9% was found in 1.5 kgs to 2.5 kgs range. And (n=18) 4.86% are less than 1.5 kgs as depicted in Table 2.
Table 2 Distribution based on birth weight
| S. No. | Birth weight | Frequency | Percentage |
|---|---|---|---|
| 1 | <1.5 kgs | 18 | 4.86% |
| 2 | 1.5 kgs-2.5 kgs | 101 | 15.90% |
| 3 | 2.5 kgs-4 kgs | 107 | 26.54% |
| 4 | Total | 226 | 100.00% |
The study reveals that the baby’s weight is (AGA) Appropriate for the Gestational Age was found to be in 79% of the babies, while a baby’s weight is more than expected for the (LGA) Large for Gestational Age was around 3% in present observation and a baby’s weight is less than expected for the (SGA) Small for Gestational Age was found in 18% of babies as shown in Figure 4.
The majority of the babies admitted with respiratory distress had normal Apgar scores of 90.41% as described in Table 3 below. Maternal risk factors included signs of infection, like fever, chorioamnionitis, uterine tenderness; prolonged rupture of membranes was major risk factors for respiratory distress 49.31%, followed by multiparity 19.8%. The majority of the mothers were steroid-covered 69.1% as shown in Table 4.
Table 3 Distribution according to Apgar scoring
| APGAR | 1 min | 5 min | ||
|---|---|---|---|---|
| No | % | No | % | |
| 0-3 | 5 | 1.71% | 1 | 0.34% |
| 4-6 | 23 | 7.87% | 3 | 1.02% |
| 7-10 | 264 | 90.41% | 288 | 98.63% |
| Total | 292 | 100.00% | 292 | 100.00% |
Table 4 Distribution according to maternal factors associated with complications
| S.no | Maternal risk factors | Frequency | Percentage |
|---|---|---|---|
| 1 | Age>30 yrs | 55 | 18.83% |
| 2 | Parity ≥ 3 | 58 | 19.86% |
| 3 | PIH | 40 | 13.69% |
| 4 | GDM | 22 | 7.53% |
| 5 | Oligo/Polyhydromnios | 32 | 10.95% |
| 6 | Antepartum Hemorrhage | 2 | 0.68% |
| 7 | Maternal infection | 144 | 49.31% |
It was observed that newborns with Transient tachypnea were found to be 45.2%, while congenital pneumonia was around 22.2% and late-onset sepsis was 10.95% were the major causes of respiratory distress in newborns in the present study. Rare causes included duct-dependent congenital heart diseases, congenital diaphragmatic hernia, and trachea-esophageal fistula. Respiratory distress syndrome accounted for only 3% of infants as shown in Table 5.
Table 5 Diagnosis of neonates with respiratory distress
| Diagnosis | Frequency | Percentage |
|---|---|---|
| Transient tachypnea of newborn | 132 | 45.2 |
| Congenital pneumonia | 65 | 22.26 |
| Sepsis | 32 | 10.95 |
| Hyaline Membrane Disease | 10 | 3.42 |
| Respiratory distress Syndrome | 9 | 3.08 |
| Meconium Aspiration Syndrome | 6 | 2.05 |
| Birth Asphyxia | 4 | 1.36 |
| Aspiration Pneumonia | 2 | 0.68 |
| Hypoxemic Ischemic Encephalopathy | 2 | 0.68 |
| Apnea of prematurity | 1 | 0.34 |
| Others | 29 | 9.93 |
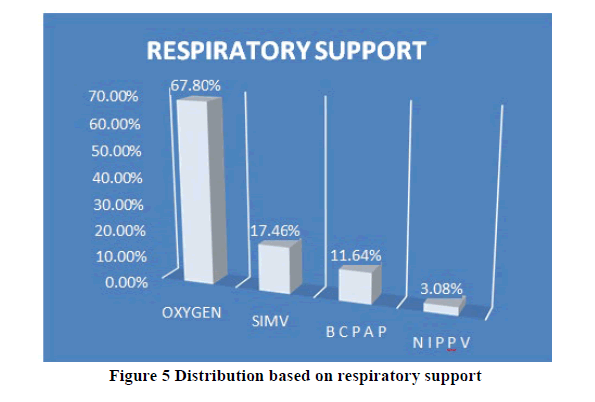
The majority of the infants required only minimal respiratory support in the form of Oxygen inhalation accounts for 67%, while 17% of the infants required invasive ventilatory support. 14.6% of the infants were put on non-invasive respiratory support in the form of CPAP and NIPPV as shown in Figure 5.
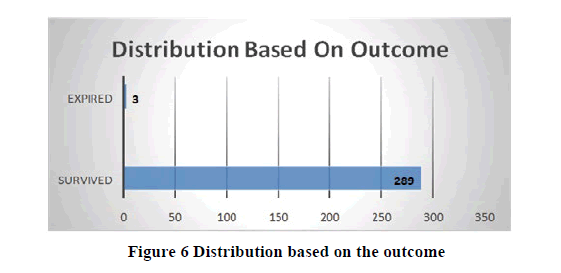
Most of the infants admitted with respiratory distress survived and were discharged on room air (98.97%), and 1% of infants expired, all preterm infants with severe Respiratory distress syndrome, extramural infants referred late to the NICU after 6-8 hours after birth as shown in Figure 6.
Discussion
Respiratory distress is one of the most common causes of NICU admission in the first 48 hours-72 hours. It occurs in 0.96% to 12% and accounts for approximately 20% of neonatal mortality. In the present study, 61.64% were females. The findings of the study were contrary to the findings of Kommawar A, et al. where the majority of the neonates were males [10]. This finding appears to be incidental. Causes for respiratory distress include transient neonatal tachypnea, hyaline membrane disease, meconium aspiration syndrome, pneumonia, and other miscellaneous causes [10].
According to Kommawar A, et al. the most common mode of delivery is LSCS, which was seen in the present study too [10]. 87.16% of them were delivered by LSCS. Our institution is a tertiary care teaching hospital and serves as a referral for high-risk pregnancies, which can account for the high incidence of caesarian sections. This can also explain the high incidence of antenatal steroid coverage as antenatal steroids are recommended not only for emergent preterm deliveries but also for elective caesarian section deliveries at term. Owing to widespread cesarean use of nonproven cephalopelvic disproportion, the reliable prevalence of obstructive labor is hard to estimate, but at least one million mothers a year have been estimated to be affected by this LSCS worldwide in a study by Benjamin, Santosh J., et al. [10,11].
Newborn transient tachypnea is the most frequent cause of neonatal respiratory distress where residual lung fluid persists even after birth. As fluid remains, the newborn presents with transient tachypnea. Maternal asthma, macrosomia, maternal diabetes, and cesarean birth are contributing factors. In the present study, the causes for respiratory distress were evaluated. The most common cause was transient tachypnea of the newborn, followed by sepsis, early-onset sepsis manifesting as congenital pneumonia, and late-onset sepsis. The findings of the present study are in concurrence with the findings of Sonawane, et al. where TTNB was the most common cause of respiratory distress [12]. Similar findings were observed by Kommawar A, et al. where Transient tachypnea of newborns contributed to 60% of the cases [10]. In the study done by Kumar A, Transient Tachypnea of Newborn (TTN) was found to be the commonest (42.7%) cause of RD followed by infection (17.0%), meconium aspiration syndrome (10.7%), hyaline membrane disease (9.3%) and birth asphyxia (3.3%) [13]. According to Tudehope et al TTN is the commonest cause of RD accounting for 41%, he also showed TTNB was more common following cesarean section before labor the reason given that is in absence of labor anticipatory lung fluid clearance will not have occurred [14]. As the incidence of cesarean sections was quite high in our institute, this could explain the high incidence of TTNB in our infants [10,12,14].
Our study reveals that the majority of the infants required minimal respiratory support in the form of oxygen inhalation as the commonest cause of respiratory distress observed was TTNB. Most of the infants requiring invasive ventilator support were infants with congenital pneumonia and severe sepsis. Most preterm infants with respiratory distress syndrome improved with non-invasive respiratory support like CPAP and NIPPV while it was observed in the other studies that pre-term babies also have respiratory insufficiency that needs respiratory support. Several short-term and long-term complications have been involved with invasive mechanical ventilation. The practice of non-invasive device use was then introduced at an early stage. As initial therapy for preterm babies, nasal CPAP proved successful. Non-invasive positive pressure breathing is a way to mitigate apnea in preterm infants or increased work of breathing [15].
Early respiratory support has a good outcome in infants with respiratory distress, as the majority of the infants recovered and were discharged. Three infants died during the study period, and these infants were diagnosed with severe Respiratory distress syndrome, and were extramural infants, referred to the NICU late in the course of the disease, and received inadequate respiratory support before transfer.
Hormones in Pregnancy
The placenta lacks all the enzymes needed to make estrogen from cholesterol and even lacks progesterone. Human trophoblasts lack 17-hydroxylase and therefore cannot convert C21 steroids into C19 steroids, the direct precursors of estrogen. DHA is converted to estradiol-17 by trophoblast cells from the fetal adrenal glands. When the placenta is a key position between the mother and the fetus, it can use the precursor of the mother and the fetus to avoid its lack of enzyme activity. Hormones act at the cellular level as catalysts for the chemical changes necessary for growth, development, and energy. The fetus lacks hydroxysteroid dehydrogenase 3B, so it cannot produce progesterone, but it is borrowed from the placenta. In return, the fetus will provide the placenta with a precursor of estrogen that it lacks (19 carbon compounds) [16].
Premature delivery should be foreseen and prevented to reduce perinatal morbidity and mortality. Women who have had a spontaneous preterm birth have a much higher risk of preterm delivery in the later stages of pregnancy. The results of several small trials have suggested that 17 alpha-hydroxyprogesterone caproates (17P) may reduce the risk of preterm delivery [16].
Conclusion
The most important risk factors for respiratory distress are delivery by caesarian section and maternal infection. The most common cause of respiratory distress is Transient tachypnea of newborns and neonatal sepsis. Early referral and early respiratory support help in better outcomes for infants with respiratory distress.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Edwards, Martin O., Sarah J. Kotecha, and Sailesh Kotecha. "Respiratory distress of the term newborn infant." Paediatric Respiratory Reviews, Vol. 14, No. 1, 2013, pp. 29-37.
- Hibbard, Judith U., et al. "Respiratory morbidity in late preterm births." JAMA: The Journal of the American Medical Association, Vol. 304, No. 4, 2010, pp. 419-25.
- Warren, Jamie B., and JoDee M. Anderson. "Newborn respiratory disorders." Pediatrics in Review, Vol. 31, No. 12, 2010, pp. 487-95.
- West, John Burnard. "Respiratory physiology: The essentials." Lippincott Williams and Wilkins, 2012.
- Williams, Olivia, et al. "Pulmonary effects of prolonged oligohydramnios following mid-trimester rupture of the membranes-antenatal and postnatal management." Neonatology, Vol. 101, No. 2, 2012, pp. 83-90.
- Piper, Jeanna M., Elly M‐J. Xenakis, and Oded Langer. "Delayed appearance of pulmonary maturation markers is associated with poor glucose control in diabetic pregnancies." The Journal of Maternal‐Fetal Medicine, Vol. 7, No. 3, 1998, pp. 148-53.
- Jobe, Alan H. "Effects of chorioamnionitis on the fetal lung." Clinics in Perinatology, Vol. 39, No. 3, 2012, pp. 441-57.
- Adzick, N. Scott, et al. "Fetal lung lesions: Management and outcome." American Journal of Obstetrics and Gynecology, Vol. 179, No. 4, 1998, pp. 884-89.
- Reuter, Suzanne, Chuanpit Moser, and Michelle Baack. "Respiratory distress in the newborn." Pediatrics in Review, Vol. 35, No. 10, 2014, pp. 417-28.
- Lakhkar, Bhavana, et al. "Study of respiratory distress in newborn." International Journal of Contemporary Pediatrics, Vol. 4, No. 2, 2017, pp. 490-94.
- Benjamin, Santosh J., et al. "Anthropometric measurements as predictors of cephalopelvic disproportion: can the diagnostic accuracy be improved?" Acta obstetricia et gynecologica Scandinavica, Vol. 91, No. 1, 2012, pp. 122-27.
- Sonawane, Ravindra, Akshay Patil, and Sagar Sonawane. "Clinical profile of respiratory distress in newborn." MVP Journal of Medical Science, Vol. 5, No. 2, 2019, pp. 151-55.
- Kumar, Alok, and B. Vishnu Bhat. "Epidemiology of respiratory distress of newborns." The Indian Journal of Pediatrics, Vol. 63, No. 1, 1996, pp. 93-98.
- Tudehope, D. I., and Margaret H. Smyth. "Is “transient tachypnoea of the newborn” always a benign disease? Report of 6 babies requiring mechanical ventilation." Journal of Paediatrics and Child Health, Vol. 15, No. 3, 1979, pp. 160-65.
- Nasef, Nehad, Hend ME Rashed, and Hany Aly. "Practical aspects on the use of non-invasive respiratory support in preterm infants." International Journal of Pediatrics and Adolescent Medicine, Vol. 7, No. 1, 2020, pp. 21-27.
- Pratap, Kumar, and M. Navneet. "Hormones in pregnancy." Nigerian Medical Journal, Vol. 53, No. 4, 2012, pp. 179-83.