Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 7
A Study of Adverse Drug Reactions in Tuberculosis Patients in a Tertiary Care Hospital
Shilpa Todkar* and Smita TiwariShilpa Todkar, Department of Pharmacology Government Medical College and General Hospital, Baramati, India, Email: shilpatodkar13@gmail.com
Received: 29-Jun-2022, Manuscript No. ijmrhs-22-68036; Editor assigned: 01-Jul-2022, Pre QC No. ijmrhs-22-68036(PQ); Reviewed: 08-Jul-2022, QC No. ijmrhs-22-68036(Q); Revised: 10-Jul-2022, Manuscript No. ijmrhs-22-68036(R); Published: 30-Jul-2022
Abstract
Background: Adverse drug reactions to anti-tubercular drugs cause significant morbidity, mortality, incurring substantial additional costs because of added outpatient visits, tests, and hospitalizations. Objectives: The study was carried out with the objectives of assessing the rate & type of Adverse Drug Reactions (ADRs) & detecting serious and preventable ADRs with a collection of demographic details of patients taking anti-tubercular drugs & developing ADRs. Methods: A Cross-sectional, prospective, observational study was conducted in the department of Chest & TB of tertiary Health care and teaching hospital in both Outpatient Department and Inpatient Department patients for 18 months. 480 patients monitored Results: Among 480 patients 120 i.e. 25% developed ADR. Frequency is significantly higher in males (58%) & adult age group (>18 years) amongst hospitalized compared to outdoor patients with the Gastrointestinal Tract (GIT) (39%) followed by, Generalized body disorders (19%) hepatobiliary system (17%) were organ systems most affected Majority (56%) ADRs reported in 0-2 month of starting therapy (63%) of cases were in “probable according to Naranjo causality assessment (37%) being possible. 55% of ADRs were moderate in severity followed by 36% mild & 9% severe. 30% of ADRs were preventable followed by 20% of probably prevented according to the schumock thronstone preventability scale. Conclusions: The study highlights the importance of routine monitoring and a robust pharmacovigilance system for the success of National Tuberculosis Programmes in India as well as worldwide.
Keywords
Adverse drug reactions, Tuberculosis, Pharmacovigilance
INTRODUCTION
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis; it is the most rambling communicable infectious disease on earth and remains out of control in many developing countries. It is the single most common cause of death in individuals aged 15 years to 49 years. India features among the 22 high TB burden countries and has accounted for an estimated one-quarter (26%) of all TB cases worldwide. Pulmonary tuberculosis is the most common presentation. Good bacteriological diagnosis and compliance with treatment are the two core stakes of successful treatment of pulmonary tuberculosis [1-3].
To strengthen the efforts to control TB, the Government of India introduced the Revised National Tuberculosis Control Program (RNTCP) in 1993, which implemented DOTS. One of the key components of DOTS therapy is the standard anti-TB short course chemotherapy regimen, which requires continually taking drug combinations for 6 months to 9 months. Despite all these initiatives and positive therapeutic effects, studies have shown that utilization of multidrug regimens can cause undesirable Adverse Drug Reactions (ADRs) of varying degrees of severity. Such as hepatotoxicity, Gastrointestinal (GI) disorders, etc [4-7].
It has achieved the global benchmark of treatment success consecutively for the last 5 years as the prevalence of ADRs observed in various studies conducted worldwide ranged from 8% to 85% and the prevalence of 2.3% to 35% in various Indian studies. Adherence to the long course of TB treatment is intricate, a dynamic phenomenon with a varied range of factors impacting treatment-taking behaviour. Treatment interruption among Tuberculosis (TB) patients and its implications are well known. One of the main reasons for treatment interruption among TB patients is Adverse Drug Reactions (ADRs). Adherence to anti-tubercular treatment is also a major challenge faced by both the policy creators and health authorities [8-10].
According to WHO “an adverse reaction is a response to a drug which is noxious & unintended & which occurs at doses normally used in man for prophylaxis, diagnosis or therapy of a disease or modification of physiological function [11]. It is likely that many of them particularly the avoidable and potentially avoidable ones may be minimized by patient and physician education and better prescribing practices and thus lead to considerable cost savings [2]. Considering adverse reactions to anti-tuberculosis drugs may be related to various factors such as the dose and time of day at which the medication is administered, patient age, nutritional status, the presence of pre-existing diseases or dysfunctions like impaired liver/kidney function, alcohol, etc. National TB programs are generally well structured to monitor patients using standardized indicators, but currently no system of pharmacovigilance to collect information on ADRs directly, treatment interruption & Loss to Follow-Up (LTFU). Once a patient is LTFU, the chances of favourable treatment decline, and the problem multiplies if drug resistance develops [12]. There is a dearth of published literature about anti-TB drug-induced mortality morbidity and reduced quality of life, particularly in low-resource settings. Data regarding ADRs related to anti-tubercular therapy are scant in the local population. [13].
Drug safety has been included in curriculum guidelines for Indian medical undergraduates (MCI Curriculum Guidelines, 1997) but little has been achieved in this regard [14]. Monitoring of adverse drug reactions should be a collaborative activity of both clinicians and pharmacologists. At present, in India, pharmacologists usually do it with or without the involvement of clinicians [2]. Physicians, however, continue to play a meaningful role in the entire monitoring process, as the cooperation of clinicians is needed to have access to patient data and interpretation of the reports of suspected adverse drug reactions Pharmacovigilance needs to be an integral accompaniment to treatment programs as they expand their geographical coverage, given that the frequency and expression of ADRs may be influenced by factors linked to the demographic, genetic and nutritional patterns, and the background comorbidity in a population [2].
Objectives
• To study adverse drug reactions in tuberculosis patients in a tertiary care hospital.
• Detecting, severe and preventable recognized ADR.
Methods
Study Design
Inclusion Criteria
This was a cross-sectional, prospective, observational study of adverse drug reactions in tuberculosis patients that was conducted in the Department of Chest &TB of tertiary health care and teaching hospital in both IPD & OPD patients Data was collected for over 18 months from December 2016 to July 2018.
Sample Size=4PQ/L (Sample size calculated by Open Epi software with (95% CI) (P-Prevalence, Q-(100-P), L (Error Percentage), wherein the prevalence of ADRs due to TB according to previous studies was 2.5% to 33% [8].
Detection and Monitoring were done by interviewing patients and reviewing laboratory tests and medical charts. Consulting with physicians about the patient’s clinical problems. Information regarding ADR was recorded as per the C.R.F (Case Record Form).
Selection Criteria
Inclusion criteria:
• Total 480 IPD & OPD patients of any age & both sex, who was diagnosed with Pulmonary Tuberculosis belonging to CAT-I & CAT-II (RNTCP guidelines 2010) with or without other respiratory co-morbidities taking drugs of Category as per DOTS.
• Willing to be part of the study was included.
Exclusion criteria:
• Patients with a non-pulmonary form of tuberculosis.
• Chronic hepatic illnesses such as cirrhosis, chronic hepatitis, and acute viral hepatitis.
• Patients with TB and HIV on HAART.
Analysis of Data
Hepatitis is defined as increased liver enzymes more than five times the baseline accompanied by clinical symptoms including jaundice, nausea, vomiting, abdominal pain, and anorexia. Hyperuricemia is defined as a Serum Uric Acid (SUA) level greater than 8.0 mg/dL, the approximate level at which urate is supersaturated in plasma.
Naranjo’s algorithm: scale used to assess causality or temporal relation between the adverse event and drug therapy. ADR is assigned to a probability category from the total score as follows Score of 9 or greater-Definite ADR, Score of 5-8-Probable ADR, Score of 1-4-Possible ADR, and Score of 0-Doubtful if the ADR.
Modified Hartwig and Siegel’s Scale: This scale is used to find the severity of ADR; Levels are decided by the answering relevant level of question and categorized as Mild-level 1and level 2, Moderate-level 3 and level 4. Severelevel 5, level 6, level 7.
Shock and Thornton Scale (preventability) Preventability of ADR is categorized as Definitely Preventable, Probably Preventable, and Not Preventable. Any answer of “yes” to any question suggesting ADR as preventable of that category (definitely/ probably) & none of the answers were yes that ADR was classified as not preventable.
ADRs were recorded in standard Central Drugs Standard Control Organisation (CDSCO) suspected adverse drug reaction form.
Data analysis
Data analysis was performed using Microsoft Excel 2013 results were expressed as numbers and percentages. p<0.05 was considered statistically significant.
Results
Demography
Among 480 patients that were observed during the study period, 120 patients developed a total of 122 adverse drug reactions. Demographic data analysis reveals that amongst the 480 patients-120 (25%) developed ADRs during the study. Amongst the 120 patients-70 (58%) were males and the rest were females. Only 15 (12%) belonged to the paediatric (<18yrs) age group and the majority 41% aged 41 years to 60 years. 92 patients (77%) belonged to <50kg weight Category A higher proportion i.e. 95 (79%) of patients were taking the CAT-I regime (Table 1).
| Category Demography | Patients with ADRs (120) | Patients without ADRS (-360) | Total (480) | Range & Mean | p-value |
|---|---|---|---|---|---|
| Male | 70 (58%) | 250 (70%) | 320 (67%) | **0.025 | |
| Female | 50 (42%) | 110 (30%) | 160(33%) | ||
| <18 years | 15 (12%) | 40 (11%) | 55 (22%) | 7 Years-70 Years | 0.68 |
| >18 years | 105 (88%) | 320 (89%) | 425 (88%) | Mean 39.5 ± 15 | |
| <50 kg | 92 (77%) | 280 (78%) | 372 (78%) | 13 kg -78 kg | 0.802 |
| >50 kg | 28 (23%) | 80 (22%) | 108 (22%) | Mean 40.25 ± 14.5 | |
| CAT-I | 95 (79%) | 265 (73%) | 360 (75%) | 0.57 | |
| CAT-II | 25 (21%) | 95 (27%) | 120 (25%) | ||
| IPD | 84 (70%) | 170 (47%) | 254 (53%) | **<0.0001 | |
| OPD | 36 (30%) | 190 (53%) | 226(47%) | ||
| Total | 120 (25%) | 360 (75%) | |||
| Z test, **p-value<0.05 is significant | |||||
Evaluations (Assessments) of ADRs
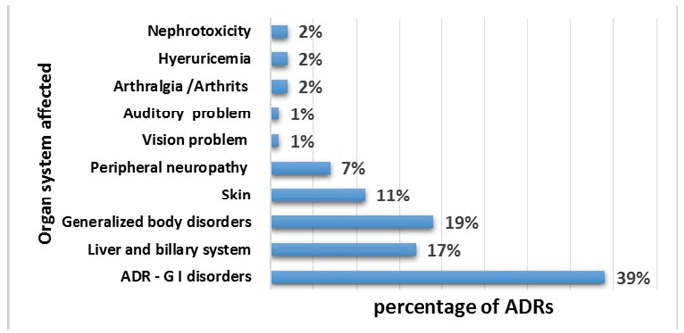
• Gastrointestinal system (39%) related ADRs were most commonly reported, followed by generalized body reactions (19%) (Fever, weakness, loss of weight, headache, etc.) liver and biliary systems contribute (17%) to ADR reporting (Figure 1). A total of 56% of ADRs like nausea vomiting rash generalized body disorders occurred within 2 months of starting therapy (Table 2 and Table 3). ADRs like hepatitis weight loss and Peripheral neuropathy were observed during 2 months-6 months of therapy initiation and after 6 months, ADRs like peripheral neuropathy and visual & auditory impairment were observed (Table 3) [3,5-7,13].
| Time of Onset | 0 Months-2 Months | 2 Months -6 Months | >6 Months | |
| <2 Week | >2 Week | |||
| % of ADRs | (22) 18% | (43) 38% | (47) 36% | (10) 8% |
| 56% | 36% | 8% | ||
| 0 Month-2 Month | 2 Month-6 Month | >6 Month | |||
|---|---|---|---|---|---|
| Headache | 2 | Hepatitis | 13 | Peripheral neuropathy | 3 |
| Rash | 6 | Peripheral neuropathy | 3 | Blurred vision | 1 |
| Nausea &vomiting | 7 | Weight loss | 5 | Auditory problem | 1 |
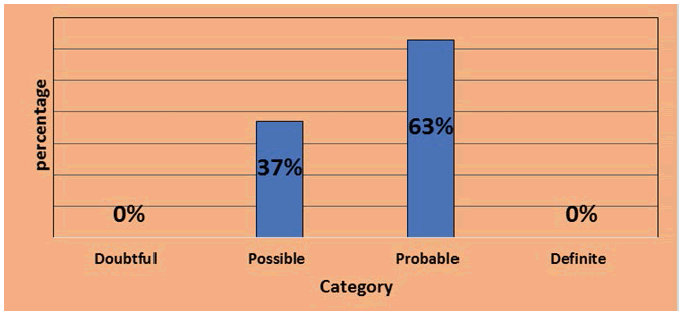
Causality assessment by Naranjo’s causality assessment questionnaire. The majority of ADRs 77 (63%) were from the Probable category and the second 45 (37%) was from the possible category (Figure 2) As lack of placebo testing, rechallenge and therapeutic drug monitoring or contribution of other reason for ADRs none of ADR was a definite category. Maximum ADRs in the Gastro-Intestinal System contribute to the probable group of Nausea and vomiting (29%) second to that were hepatitis (18%) and Rash (10%) were the most frequent ADRs in the probable group. Anorexia (13%) Nausea and Vomiting (11%) and other generalized body disorders like Headache, and hypotension anaemia were the most frequent ADRs in the possible category (Table 4).
| Probable group | Possible group | ||
|---|---|---|---|
| ADR | Incidence (%) | ADR | Incidence (%) |
| Nausea and vomiting | 29% | Weakness | 7% |
| Hepatitis | 18% | Hypotension | 9% |
| Rash | 10% | Nausea and vomiting | 11% |
| Others | 42% | Others | 73% |
• 55% of ADRs belong to the moderate category (level 3 and level 4), and 36% of ADRs fall in the mild category (level 1 and level 2) which doesn’t require any special treatment or antidote or to change the current regime but some patients by withholding it (Level 2) for the duration without other changes. Whereas the severe group entails 9% ADRs (Table 5).
| Level | Frequency | Total | Severity |
|---|---|---|---|
| Level-1 | 42 (34%) | 36% | Mild (36%) |
| Level-2 | 2 (2%) | ||
| Level-3 | 42 (34%) | 55% | Moderate (55%) |
| Level-4 | 25 (21%) | ||
| Level-5 | 10 (8%) | 9% | Severe (9%) |
| Level-6 | 1 (1%) |
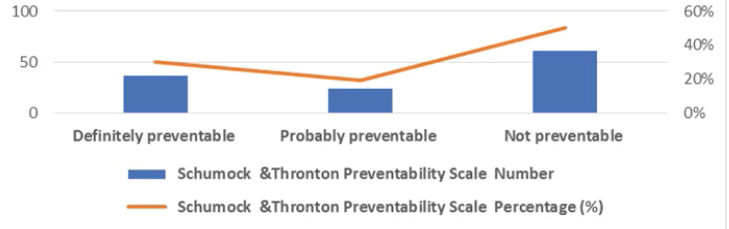
Out of 122 majorities, 62 (50%) ADRs were not preventable. Followed by 36 (30%) preventable and only 24 (20%) were probably preventable (Figure 3).
Discussion
The incidence of adverse drug reactions among Pulmonary Tuberculosis patients in our hospital during the study period was found to be 25% which is by earlier studies that reported a comparable incidence of 18.20% to 25.01% [15- 17]. Whereas some studies showed a higher incidence of ADRs 48%-80% [18,19]. This divergence can be ascribed to disparities in the study settings and differences in the geographical and physical factors of the sample population. Out of 120 patients, a statistically significant number of ADRs were observed in males (58%) in consonance with other Indian studies due to higher enrolment. Only 12% belonged to the paediatric age group i.e. 18 years due to hurdles in diagnosis & reporting of ADRs in children [17,20]. The highest reporting in the age group 40 years-60 years was in concordance with other Indian studies [15]. The majority of patients having ADRs were <50 kg accordance to an Indian study. About 79% of ADR was reported amongst patients taking the CATI regime which is to another study [21,22]. 70% of the ADR cases were reported from IPD because hospitalized participants were likely to have more complex and serious diseases and were monitored more frequently, thus increasing the chances of discovering ADRs [23]. The majority of ADRs were related to GIT (39%) followed by generalized body disorders (19%), liver and biliary system (17%), and others.
The increased incidence of GI side effects could be attributed to multiple drug therapy as a major predisposing factor for ADRs. Higher rate of ADRs occurrence with intensive phase treatment which matches with another study [24]. Certain ADRs like hepatitis, hyperuricemia and nephrotoxicity neurotoxicity are not recognizable easily by patients and require investigations hence reported in an intermediate period (2 months-6 months).
This observation rings a bell that there is a need for rigorous monitoring for early detection and subsequent prevention of such ADRs that are probably associated with anti-tubercular treatment which were seen to be reported late period >2/6 months. The majority of the reactions were found to be moderate as a proper treatment measure was required even after the suspected drug was held discontinued or changed i.e. antacids, NSAIDS, antibiotics, etc [25]. Contradicting the finding of the present study observed higher reporting of 73% of mild ADRs due to vigilant reporting [23].
Contradictory to reports in literature present shows 50% of ADRs were nonpreventable but the brighter side was that 30% of these reactions were preventable [25]. Noting a detailed history of reaction /known allergy may help reduce them.
In the 33 Cases of ADRS (27%) continues current treatment without any change or any symptomatic treatment similar to the study [26].
Conclusion
The present study highlights differences in ADR reporting based on parameters like sex and age. More males had been enrolled and had reported as compared to the female counterparts ADRs. Similar findings were observed in the age group 40 years-60 years. Who had a higher ADR reporting as compared to the paediatric age group? These observations thereby stress the importance of detecting and identifying Tuberculosis (TB) in the said groups. The most common ADRs were related to the gastrointestinal system but ranged from moderate to severe and therefore need symptomatic treatment. Unlike few ADRs that were of the severe category (e.g. peripheral neuropathy, auditory impairment) but were also probably related to the drug; were reported late after therapy initiation. This indicates that appropriate physical education and early detection or monitoring can play a role in preventing such consequences.
Declarations
Strengths
The study provides an insight into the need for implementation of a robust pharmacovigilance program and appropriate patient counselling that emphasize follow-up visits, which will help in the early identification of ADRs that occur within 2 weeks of initiation of treatment.
Limitation
Association of ADR with risk factors like alcohol, smoking, etc. could not be established due to missing data.
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Dale, David C., "Infectious diseases: the clinician's guide to diagnosis, treatment, and prevention." Webmd Prof Pub, 2003.
- Patidar, Dindayal, et al. "Implementation and evaluation of adverse drug reaction monitoring system in a tertiary care teaching hospital in Mumbai, India." Interdisciplinary toxicology, Vol.6, No. 1, 2013, p. 41.
Google Scholar Crossref - World Health Organization. "Global tuberculosis report 2013." World Health Organization, 2013.
Google Scholar - Chauhan, L. S., and S. P. Agarwal. "The revised national tuberculosis control programme." Tuberculosis control in India. New Delhi: Directorate General of Health Services, Ministry of Health and Family Welfare, 2005, pp. 23-34.
Google Scholar - World Health Organization. "An expanded DOTS framework for effective tuberculosis control." International Journal of Tuberculosis and Lung Disease, vol. 6, 2002, pp. 378-88.
Google Scholar - Agarwal, S. P., et al. "The history of Tuberculosis Control in India: Glimpses through decades." Tuberculosis Control in India. New Delhi, India, Directorate General of Health Services, Ministry of Health and Family Welfare, 2005, pp. 15-22.
Google Scholar - Zaka-Ur-Rehman, Z, Mohammad Jamshaid, and Akram Chaudhry. "Clinical evaluation and monitoring of adverse effects for fixed multidose combination against single drug therapy in pulmonary tuberculosis patients." Pakistan Journal of Pharmaceutical Sciences, Vol. 21, No. 2, 2008, pp. 185-94.
Google Scholar - Singh, Abhijeet, et al. "Prevalence of adverse drug reaction with first-line drugs among patients treated for pulmonary tuberculosis." Clinical epidemiology and global health, Vol. 3, 2015, pp. S80-S90.
Google Scholar Crossref - Marra, F., et al. "Adverse drug reactions associated with first-line anti-tuberculosis drug regimens." The International Journal of Tuberculosis and Lung Disease, Vol. 11, No. 8, 2007, pp. 868-75.
Google Scholar - Dalal, Nishant P., Yogita S. Karandikar, and Vijaya A. Pandit. "Safety evaluation of directly observed treatment short course (DOTS) regimen in a tertiary care hospital, Pune." International Journal of Basic & Clinical Pharmacology, Vol. 3, 2014, pp. 369-76.
Google Scholar Crossref - Edwards, I. Ralph, and Jeffrey K. Aronson. "Adverse drug reactions: definitions, diagnosis, and management." The lancet, Vol. 356, No. 9237, 2000, pp. 1255-59.
Google Scholar Crossref - Grammer, Leslie C., and Paul A. Greenberger. "Patterson's allergic diseases." Lippincott Williams & Wilkins, 2012, p.295.
Google Scholar - World Health Organization. "A practical handbook on the pharmacovigilance of medicines used in the treatment of tuberculosis: enhancing the safety of the TB patient." 2012.
Google Scholar Crossref - Bhatia, M. L., et al. "Comparison of Outcomes of Two Antitubercular Regimens in Pulmonary Tuberculosis at Tertiary Care Hospital." Medical Science, Vol. 3, No. 2, 2013, pp. 275-77.
Google Scholar Crossref - Leape, Lucian L. "Error in medicine." Jama, Vol. 272, No. 23, 1994, pp. 1851-57.
Google Scholar Crossref - Bai, G. P., P. Ravikumar, and U. Salma. "A study of adverse drug reaction among pulmonary tuberculosis patients treated under DOTS in a tertiary care hospital." International Journal of Basic and Clinical Pharmacology, Vol.6, No. 4, 2017, pp. 779-83.
Google Scholar Crossref - Nanda, Gurprit S., et al. "Adverse reactions due to directly observed treatment short course therapy: an Indian prospective study." International Archives of Integrated Medicine, Vol. 3, No. 1, 2016, pp. 6-12.
Google Scholar Crossref - Athira, B., C. S. Manju, and E. Jyothi. "A study on adverse drug reactions to first line antitubercular drugs in DOTS therapy." International journal of pharmacology and clinical sciences, Vol. 4, No. 1, 2015, pp. 7-11.
Google Scholar - Anusha, N., Isabella Topno, and Anil J. Purty. "Adverse drug reactions monitoring among TB patients on anti-tubercular drugs under RNTCP in Pondicherry." International Journal, Vol. 2, No. 12, 2014, pp. 165-73.
Google Scholar - Koju, Dinesh, et al. "Occurrence of side effects from anti-tuberculosis drugs in urban Nepalese population under DOTS treatment." Kathmandu University Journal of Engineering Science and Technology, Vol. 1, No. 1, 2005, pp. 1-2.
Google Scholar - Tak, D. K., et al. "Safety evaluation of antitubercular therapy under revised national tuberculosis control programme in India." Journal of Clinical and Diagnostic Research, Vol. 3, No. 2, 2009, pp. 1395-01.
Google Scholar - Dedun, Amit, and Dharmeshkumar Patel. "A Profile of Adverse Effects of Anti-Tubercular Drugs." GCSMC Journal of Medical Sciences, Vol. 5, No. 1, 2016, pp. 37-41.
Google Scholar Crossref - Sinha, Kumarjit, Izora T. Marak, and W. Asoka Singh. "Adverse drug reactions in tuberculosis patients due to directly observed treatment strategy therapy: Experience at an outpatient clinic of a teaching hospital in the city of Imphal, Manipur, India." The Journal of Association of Chest Physicians, Vol. 1, No. 2, 2013, p. 50.
Google Scholar - Gholami, Kheirollah, et al. "Evaluation of anti-tuberculosis induced adverse reactions in hospitalized patients." Pharmacy practice, Vol. 4, No. 3, 2006, p . 134.
Google Scholar - Hassan, Mohd Khalid, et al. "Incidence of Adverse Drug Reactions among the Tuberculosis Patients Treated under Directly Observed Treatment Short course (DOTS) regimen in North India." Indian Journal of Applied Research, Vol. 6, No. 7, 2016, pp. 598-600.
Google Scholar Crossref - Sreekanth AS. "A Pharmacovigilance Study on Antitubercular Therapy in the Department of Pulmonary Medicine at a Tertiary Care Hospital." IOSR Journal of Dental and Medical Sciences, Vol. 14, No. 8, 2015, pp. 2279–61.